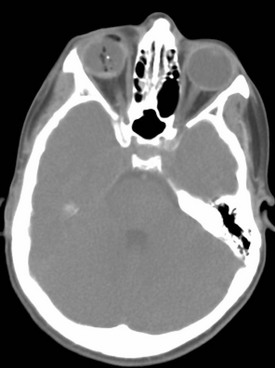
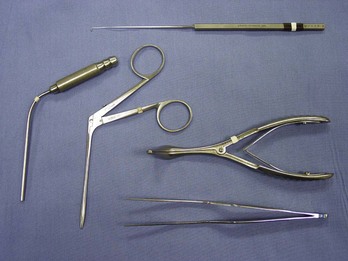
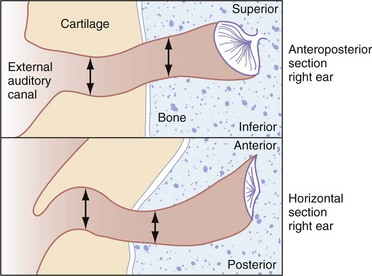
Chapter 60 When people ingest or insert foreign bodies, a brief history may be sufficient to establish the diagnosis, guide initial management decisions, and predict the process required for definitive removal. Sometimes, however, diagnosis and management of a foreign body might require a meticulous history and insightful care. Those at higher risk of having a foreign body include neurologically impaired patients, edentulous individuals, patients with certain psychiatric diagnoses, incarcerated individuals, and individuals at the extremes of age. In these same groups, definitive history is often elusive, and the clinician should use situational clues. Even when patients are fully cooperative, the diagnosis of foreign body ingestion or insertion can be difficult, especially when the expression of the foreign body is delayed. Although foreign body cases are usually not diagnostic dilemmas, the emergency physician should keep in mind the unusual possibility of “foreign body mimics” (e.g., angioedema manifesting as esophageal foreign body sensation).1 When the foreign body represents an immediate threat to the patient, as is the case with an airway foreign body, the need for urgent extraction is obvious. Trauma-related foreign bodies, such as knives and bullets, pose important management decisions (see other trauma chapters in this text). Even in cases in which no immediate life threat exists, some foreign bodies should be removed because of the threat of injury from the nature or constituents of the foreign body. For instance, cocaine can kill a body packer,2 an impacted button battery can cause fatal electrochemical tissue damage,3 and an insect can damage otic structures.4 Although wooden and metallic fragments are found most frequently, ophthalmic foreign objects vary widely. The diagnosis usually is self-evident. However, extraocular and intraocular foreign bodies may be subtle in presentation, with mild symptoms and uncharacteristic histories involving seemingly trivial trauma, such as brushing against a bush or falling. In some cases, foreign bodies are identified in intoxicated patients with abnormal ocular examination findings and no known history of trauma (Fig. 60-1). Early diagnosis, appropriate care, and follow-up minimize the risks of delayed sequelae, such as endophthalmitis (which may occur within 48 hours after foreign body introduction) or sight-threatening siderosis bulbi.5,6 Controversy regarding foreign body removal and its timing does not diminish the importance of making the initial diagnosis. Most patients report a foreign body sensation (often on blinking) and cannot see the foreign body. If the object is corneal, the patient may be able to see something in the visual field or may see the foreign body when looking in the mirror. The patient also may complain of frequent or constant lacrimation and conjunctival reddening. Foreign bodies that create corneal injury and are no longer present may account for symptoms identical to those noted in the presence of a foreign body. In addition, patients may have symptoms in the absence of any history of known foreign body. In these cases the occupational and social history, including pets and hobbies, may shed light on the diagnosis. Another important component of the history is whether radial keratotomy has been performed. This procedure is associated with potential for foreign body entrapment in the corneal incisions, which can gape as long as 6 or more years postprocedure.7 The initial survey includes standard elements of the emergency department (ED) eye examination. Early visual acuity is an important predictor of final visual outcome in cases of intraocular foreign body.8 During slit-lamp examination, the emergency physician may detect a corneal foreign body by the shadow it casts on the iris. The slit lamp can facilitate identification of rust rings, and fluorescein can aid in detecting abraded corneal epithelium. The inner aspects of both lids must be examined. The lower lid is often successfully exposed with gentle manual retraction outward and downward as the patient looks upward. The upper lid is usually exposed through eversion by instructing the patient to look downward while upward traction on the eyelashes is applied; an applicator stick is placed, to act as a fulcrum, on the proximal edge of the tarsal plate. After location and removal of one foreign body, complete examination should seek presence of other ocular objects. The foreign body may have penetrated the anterior eye structures and entered the globe (see Fig. 60-1). If the history and mechanism of injury are compatible with ocular penetration by radiopaque material, or if a small wound of the globe is noted, anteroposterior and lateral radiography of the orbit is a reasonable initial step. However, the multiple advantages of computed tomography (CT) render this technique the preferred first choice when intraocular penetration is strongly suspected.9 As compared with plain radiographs, CT delivers less radiation to the lens. Multiplanar reconstruction minimizes streak artifacts, affording better localization of intraorbital objects. When globe penetration is strongly suspected, staining with fluorescein is best avoided owing to obscuration of the physical examination. When perforation is judged unlikely and fluorescein is administered, identification of rivulets of fluorescein tracking from the puncture (i.e., positive Seidel test result) is helpful in identifying the fact that intraocular penetration has occurred. In one case series of 288 patients, Luo and Gardiner reported a near-zero incidence of intraocular foreign body in patients with corneal metal foreign bodies after low-velocity (nonexplosive) exposures.10 Ultrasound is a useful adjunct to CT scanning in patients with foreign bodies that are difficult to localize.11 When CT will be delayed, or if ionizing radiation is a concern, two ultrasound techniques can be useful in searching for foreign bodies. B-scan ultrasound, available in many EDs, has occasionally been reported successful in detecting foreign bodies missed on ophthalmologic examination.6,12 For patients in whom a foreign body is suspected despite negative ED workup and imaging, the more advanced technique of ultrasound biomicroscopy, available in ophthalmologic specialty centers, is helpful. The sensitivity of this modality is sufficient that it detects foreign bodies not visible by direct or indirect ophthalmologic examination, traditional B-scan ultrasound, or CT.13 Given the lack of reported case series and justifiable concerns about eye damage from mobilization of ferromagnetic foreign objects, use of magnetic resonance imaging (MRI) for ophthalmologic foreign body imaging remains controversial.5 In nearly all cases, therapy is removal of the foreign body. If the object is located on the bulbar or palpebral conjunctiva (not the cornea), it often can be removed easily by sweeping the site with a moist cotton-tipped applicator. Usually, other instruments are required (Fig. 60-2). Occasionally, if the foreign body is large, it may be extracted with forceps. For small corneal foreign bodies, after application of topical ocular anesthesia, it is often necessary to use an eye spud or small-gauge needle to move gently underneath one end of the object and pick it out; magnification is usually helpful. If the attempts at foreign body removal are unsuccessful or if the foreign body is deeply embedded, preventing removal, the patient should be referred for object removal within 24 to 48 hours. Although there is a paucity of evidence addressing the oxidation rate of metallic corneal foreign bodies, prudence dictates early “rust ring” to minimize growth of metallic oxides. Overly vigorous attempts at removal may cause anterior chamber perforation. It is prudent for the emergency physician to avoid significant corneal procedures in patients who have had a laser-assisted in situ keratomileusis (LASIK) procedure for nearsightedness. In patients with ear complaints with recent travel or camping history or poor living conditions, geographic information may suggest insects inhabiting the external ear canal; in most cases, the cockroach is the culprit.14 Patients with foreign bodies in the ear may have secondary symptoms related to pathology in adjacent structures. Malocclusion may be the chief complaint if the foreign body erodes to the temporomandibular joint.15 Similar erosion has caused otic foreign bodies to manifest as eustachian tube dysfunction, parapharyngeal abscess, or mastoiditis with progression to fatal brain abscess and meningitis.16 Such events are exceedingly rare. The external auditory canal is cylindrical with an elliptic cross section (Fig. 60-3). A thin layer of sensitive epithelium covers an outermost cartilaginous portion and an inner bony segment. There are two anatomic points of narrowing (and foreign object lodging) within the canal: (1) near the inner end of the cartilaginous portion of the canal and (2) at the point of bony narrowing called the isthmus. Figure 60-3 Horizontal and vertical cross sections of external ear canal showing points of anatomic narrowing. Inspection of the tympanic membrane is important because it may have been ruptured by the foreign object or by prior removal attempts. If so, medical documentation should indicate that this rupture was present before attempts at foreign object removal. As in other body locations (especially the nose), the risk of multiple foreign objects is such that if one foreign object is identified, the emergency physician should search for additional material.17 In most cases, foreign body removal attempts may be instituted in the ED. Presence of a foreign body for more than a day or in a very young patient (younger than 4 years) does not constitute an independent risk factor for foreign body removal failure or complication; the emergency physician may thus proceed with removal efforts if not otherwise contraindicated.18 The patient should be informed about the extreme sensitivity of the auditory passage and the likely discomfort and potential for minor bleeding. Sedation may be important to minimize patient discomfort and reduce risks of iatrogenic trauma. Lidocaine instillation may aid in topical anesthesia; liquid 1% or 2% solution is preferred to gel preparations, which impair visualization needed for removal. Less often, foreign body removal requires local anesthesia of the external ear canal. The anesthesia instillation procedure, which may cause patient discomfort and iatrogenic injury, is performed by injecting all four quadrants of the canal with lidocaine via a tuberculin syringe inserted through an otic speculum. In cases of a refractory foreign body and an uncooperative patient, definitive management should be performed with procedural sedation or even general anesthesia. Although the evidence is not universally consistent, available data suggest that approximately 95% of aural foreign bodies can be removed without the need for general anesthesia.19 When the ear canal is inhabited by an insect, it is important to kill or immobilize the creature to facilitate its removal. Immobilization reduces the chance of patient discomfort or ear damage caused by an insect attempting to evade forceps introduced into the ear canal. Patient comfort may also be optimized by minimization of shining light into an ear canal inhabited by light-avoiding insects (such as cockroaches). Different immobilizing agents have different reported success rates. Efficacious formulations include lidocaine as a 10% spray or less concentrated liquid, 2% lidocaine gel, mineral oil with 2% or 4% lidocaine, and alcohol.4 One study suggests that microscope immersion oil is more efficacious than lidocaine preparations.20 Several extrication methods may prove effective, and various instruments may be useful (Fig. 60-4). Small objects often can be removed by the application of suction with a small plastic catheter. With soft or irregularly shaped objects, it is often possible to grasp the foreign body with forceps (alligator forceps may be best) and remove it either in one piece or in fragments. If the object cannot be grasped, it may be possible to remove it by passing a blunt-tipped right-angle hook beyond the foreign body and gently coaxing it out. Alternatively, a balloon-tipped catheter can be passed distal to the object, with subsequent attempts to withdraw the (inflated) balloon and extract the object. Any balloon-tipped catheter design may be used, as long as its caliber is small enough (about 18 gauge or smaller) to allow comfortable introduction into the ear canal; a typical commercial device is shown in Figure 60-5. Indirect methods for foreign body removal also have been used with some success. The irrigation technique takes advantage of the elliptic shape of the external ear canal. A stream of room-temperature water or saline should be directed at the (nonvegetable) foreign body’s periphery via a 20-mL syringe and a 14- or 16-gauge catheter (this setup is safe in terms of pressure on the tympanic membrane).21 The hope with irrigation is that the jet of water will be directed past the object, against the tympanic membrane, and finally against the posterior aspect of the foreign body, driving it out of the canal. There are no significant complications with use of the technique, and it is well tolerated by children and adults. This modality should not be used if there is a known history or clinical suspicion of tympanic membrane perforation. Removal of objects from the middle ear with cyanoacrylate adhesive-tipped swabs has been recommended in the past. This technique carries the risk, however, of contaminating the ear canal with a substance that is difficult to remove and has been associated with tympanic membrane rupture.22 Insufficient evidence exists to condone or condemn this technique. If these methods are unsuccessful or if the patient, especially a child, is uncooperative or in undue distress even with procedural sedation, the emergency physician should cease removal efforts and refer the patient to an otolaryngologist; timing is dependent on the acuity of the presentation. Rates of operative intervention vary in published series. Studies’ case mix differences are probably responsible for the varying rates (from 5-33%) of reported need for surgical removal of otic foreign bodies.18,19 Inappropriately prolonged efforts at foreign object removal can result in wasted time, unnecessary patient discomfort, and high potential for complications as previously noted. Patient apprehension, untoward foreign body movement, or damage to the ear canal (including induction of edema) may prompt surgical intervention that would have been otherwise unnecessary.23 Otic foreign bodies are associated with many sequelae, but these are usually not serious. The most commonly occurring complications in pediatric series are external ear canal bleeding (approximately 16%), otitis externa (6%), and tympanic membrane perforation (2%).19 One large series suggests that otitis externa is significantly more likely in adults than in children, perhaps because of relative delays in seeking medical attention.24 After removal of the foreign body, the canal examination is repeated to ensure the lack of retained material and to evaluate otic anatomy. In cases in which the tympanic membrane is ruptured and the middle ear is at risk for infection, appropriate oral antibiotics are recommended. Common practice is to prescribe topical antimicrobial therapy to decrease the risk of external otitis; the meatus may be packed with an ear wick or ribbon gauze impregnated with a broad-spectrum antibiotic.4 Follow-up evaluation within 2 to 3 days is recommended for cases in which there was tympanic membrane rupture or in which foreign body removal was traumatic (to assess for external otitis). The nose is perhaps the most common site for the insertion of foreign bodies by children. Perhaps because most people are right-handed, most nasal foreign bodies are right-sided.25 Compared with patients with ear canal foreign bodies, children with nasal foreign bodies tend to be younger (most commonly younger than 5 years).17 Nasal foreign bodies are less problematic than foreign bodies in other locations. ED removal is nearly always successful, and, with proper technique (e.g., care to avoid aspiration), serious sequelae are rare.25 Available data suggest that the overall risk that nasal foreign bodies will enter the bronchial tree is less than 0.06%.26 The infrequently encountered cases of intranasal magnets or alkaline button batteries, which may cause electrical or chemical burns and tissue necrosis, are exceptions to this rule of minimal risk.27 Although most patients seek medical attention within 24 hours, patients with nasal (versus otic) foreign bodies are more likely to have secondary symptoms and delays of 1 week.28 In fact, nasal foreign bodies may be asymptomatic, identified as incidental findings on imaging obtained for other purposes. Patients seen in the ED with nasal foreign bodies usually have one of two histories. With the first type of presentation, the patient admits to or was seen placing an intranasal object. This is the most common history. Other patients have a constellation of signs and symptoms: purulent, unilateral, malodorous nasal discharge or even persistent epistaxis. These patients often are misdiagnosed and treated with antibiotics for supposed sinusitis. Unresolving sinusitis despite appropriate antibiotic therapy is an alert to the possibility of a nasal foreign body.28 As with foreign bodies of the ear canal, preparing the patient (and the parents) for examination and subsequent removal attempts is an important component of the care plan. Because of risks of iatrogenic movement of the foreign body further posteriorly, children may need to be restrained to permit the examination. Physical examination sometimes can be delayed until after insufflation of the nares is attempted. The nasal mucosa is normally quite sensitive, and this sensitivity is increased by any infection or irritation. Examination is facilitated by provision of topical anesthesia and vasoconstriction to the nasal mucosa. Examination should include both nares, with adequate lighting and visualization with a nasal speculum. The emergency physician should note the presence of the foreign body and any secondary tissue damage. Necrosis of the nasal mucosa and septum may accompany button battery impaction.29 During the examination the emergency physician should take care not to dislodge or drive the foreign body posteriorly into the nasopharynx and risk aspiration. In some circumstances, it may be prudent to place patients in the lateral decubitus position, perhaps with additional Trendelenburg’s positioning, to help prevent aspiration of objects that are pushed into the posterior pharynx. Diagnostic imaging does not usually play a major role, although some have advocated for low-threshold use of plain radiography when button-battery foreign bodies are suspected.30 When intrasinus foreign bodies are suspected, CT can be helpful. Rarely, CT or MRI may be indicated to visualize suspected foreign bodies or their complications. The potential risk of MRI for detection of foreign bodies may become more relevant with increasing frequency of foreign bodies related to magnetic jewelry (i.e., nose rings and studs).31 The emergency physician can remove most nasal foreign bodies. Although the avoidance of iatrogenic injury is paramount, the structures local to an intranasal foreign body are not as sensitive or easily damaged as structures in other body cavities (e.g., the ear canal) that may harbor foreign objects. As a result, the need for subspecialty consultation and operating room removal is rare.17,28 Occasionally, positive pressure applied to the patient’s mouth achieves rapid foreign body dislodgment while obviating the need for restraint, sedation, and other requirements attendant to more invasive removal techniques. This technique is a quick and safe primary intervention. The underlying principle is that a short burst of air blown into the mouth of a child, with finger occlusion of the nonobstructed naris, may force the foreign object out of the nose. Pretreatment with vasoconstrictive spray may improve chances of success.32 The insufflation, preferably applied as a “kiss” from a parent, can also be provided by a manual ventilation bag. The insufflation technique is quite useful, particularly in preschoolers who are likely to be uncooperative with other removal modalities. Many children can be instructed to take a deep breath and blow hard through their nose, as a parent closes the unaffected naris. An otherwise troublesome removal can be accomplished quickly and easily.33 Recent data suggest that the “kissing” technique’s success rate of nearly 50% was associated with additional advantages of decreased use of resources (e.g., time, anesthetics).34 When positive-pressure insufflation is not warranted or is unsuccessful, instruments and removal techniques may be required (see Figs. 60-4 and 60-5). Regardless of the method, the patient (usually a child) may benefit from some combination of restraint, sedation, and pretreatment with vasoconstrictive agents (e.g., nebulized racemic epinephrine) and anesthetic (e.g., benzocaine spray).32 Adequate illumination is essential. Necessary instruments include a blunt-tipped right-angle probe, suction catheter, and alligator forceps. The forceps are used when the foreign body is to be directly grasped, and the right-angle probe is used in an attempt to reach behind the foreign object and displace it forward. Other useful instruments include Fogarty (vascular) and Foley catheters; “specialized” balloon-tipped catheters also are available in many EDs (see Fig. 60-5).17 Magnets may be useful when the intranasal foreign body is part of magnetic jewelry.31 Suction is primarily necessary for removing purulent secretions and any blood that may obscure the field. In some cases, suction can be used to withdraw foreign bodies directly. Suction may be useful with hard-to-grasp objects or small soft objects not tightly lodged in place. Cyanoacrylate-tipped swabs may be useful in certain circumstances. As noted previously with respect to otic foreign bodies, there is insufficient evidence to draw definitive conclusions about this approach. Although improved diagnostic and therapeutic techniques have markedly reduced fatality rates from foreign body inhalation, airway tract foreign objects still cause significant mortality and anoxic brain damage. One large-city series of ambulance-transported airway foreign body patients reports a 3.3% mortality (an average of one patient per month) in the prehospital phase alone.35 Alternatively, airway foreign objects can have a presentation that is less dramatic than acute respiratory distress and can go undiagnosed for years. Delay in presentation and correct diagnosis is, perhaps surprisingly, common. Only half of patients in one pediatric series of lower respiratory tract foreign body were seen within 1 day of aspiration; an additional 20% were seen during the first week, and another 20% were seen after a delay of more than 1 week.36 Another pediatric study identified a doubling of complication rates in patients who came to the hospital more than 48 hours postaspiration.37 Patients with uncharacteristic presentations may have unusual foreign body introduction mechanisms, such as ingestion or penetrating trauma.38 Patients with altered mental status from a variety of causes are at risk for occult aspiration, which may be difficult to diagnose. Even in large-series reports of aspiration, specific and reliable indicators of airway foreign body presence are elusive.39 The most common airway foreign bodies in one series were ingestible agents, primarily meats and medications.35 Airway foreign body series also identify pins, needles, jewelry, thermometers, pencils, and metal and plastic toys. The primary reason to characterize the type of airway foreign object is to determine the likelihood of radiopacity. Most airway foreign bodies are not visible with plain films.40 In one 8-year pediatric series of foreign body aspiration, the most commonly identified objects were nuts (59%) or other vegetable material (23%) not likely to be visualized on plain films. In another classic paper describing childhood asphyxiation with foreign bodies, nearly half of fatal choking cases were a result of food aspiration, with hot dogs (17%), candy (10%), nuts (9%), and grapes (8%) most prominent.41 In another report, more than 90% of pediatric aspiration cases were of organic classification (usually nuts).42 Airway foreign bodies are seen more commonly in pediatric patients.43 In one case series covering two decades, 75% of patients were younger than 9 years.42 Peak incidence of aspiration is in the second year of life, with a brisk decline after age 3.43 Mastication difficulty secondary to premature molar teeth contributes to pediatric food aspiration.36 Also, the fact that children explore their environment with their hands and mouth translates into aspiration of nonfood objects. In adults, the peak aspiration incidence is in the elderly.35 Some evidence suggests that adults are more likely than children to have nonfood items aspirated into the airway.44 Children and adults also differ with respect to anatomic location of aspirated foreign bodies. This is crucial because foreign body location plays a major role in determining associated morbidity or mortality risk. In adults, 75% of foreign bodies lodge in the proximal airways (larynx, trachea, main bronchi). In children, fewer than half of foreign objects are located proximally, with bronchial tree locations the most common.42 Foreign bodies can be located as proximally as the oropharynx, with retained intraoral bodies having been found in the medial pterygoid space.45 The foreign object can be slightly distal, causing airway obstruction at the laryngeal or subglottic level. Foreign body impaction at this level often is caused by inappropriately executed attempts to finger sweep an oropharyngeal foreign body.44 Subglottic foreign bodies are difficult to identify and may be associated with diagnostic delay in most cases.46 The emergency physician needs to be able to glean historical clues to differentiate epiglottitis, asthma, and laryngotracheobronchitis from subglottic foreign body. Airway foreign bodies usually pass beyond the laryngeal inlet44 and may cause drastic obstruction. Unfortunately, tracheal foreign bodies have a surprisingly high incidence of lack of symptoms or worrisome clinical findings. Foreign bodies passing beyond the trachea are less likely to cause acute hypoxic crisis but can cause substantial respiratory embarrassment and can be difficult to remove. In adults, bronchial foreign bodies are found more often in the right bronchial tree. In one large series, 69% of bronchial foreign bodies were right sided.42 The preferential passage of foreign bodies to the right side of the bronchial tree is usually reported to be less common for children than for adults. Some series report roughly equal left-right distribution of lower airway foreign bodies.36 The explanation may be that whereas the carina is positioned right of the midtrachea in a third of children (and in 40% of infants), the proximal right bronchus is both wider and more steeply angled than the left.47 Foreign objects can be bilateral, with 3.6% of patients in one series having foreign bodies in the right and left main bronchi.42 Clinical presentation can range from chronic nonspecific respiratory complaints to acute airway obstruction.48 In most aspiration cases, foreign body presence is suspected after a thorough history. In the most dramatic cases, patients have a history of what is commonly termed the “cafe coronary.” The patient attempts to swallow a food bolus (usually meat) larger than the esophagus can accept. The bolus lodges in the hypopharynx or trachea. Often there is confusion over whether the patient is having a myocardial infarction or has an obstructing foreign body, but the conscious cardiac patient is able to speak. Patients with airway foreign bodies may have noisy breathing, inspiratory stridor, vomiting, and possibly slight hemoptysis.35 Some patients may give a history similar to cafe coronary, with resolution of major symptoms. These symptoms, known as the penetration syndrome, occur in half of patients aspirating and include a choking sensation accompanied by respiratory distress with coughing, wheezing, and dyspnea.42 Symptom resolution may result from the patient spontaneously clearing the foreign body by coughing. In some cases, coughing does not eject the foreign body completely, but rather impacts it in the subglottic region.44 The emergency physician should maintain concern for retained airway foreign object in cases in which the patient history is one of perceived foreign body followed by cough with incomplete (or even complete) post-tussive symptom resolution. In a 20-year series of adult and pediatric patients with suspected foreign body aspiration, sudden onset of choking and intractable cough were present in half, with eventual foreign body identification.42 In addition to coughing and choking, stridor is a frequent component of an acute aspiration episode in patients of all ages.44 Symptom distribution is similar in adult and pediatric patients,42 but choking and wheezing appear more prominently in the pediatric literature. In one series of 87 pediatric patients with suspected foreign body, 96% had a history of a choking crisis.49 Wheezing is common, having been reported in up to 75% of patients aged 8 to 66 months with airway foreign bodies.36,43 Most patients aspirating objects have persistent symptoms (e.g., cough, wheezing, dyspnea) after manifesting penetration syndrome, but 20% have no ongoing symptoms.42 Many patients have a history of alarming symptoms followed by few ongoing complaints; the emergency physician should not dismiss aspirated foreign body from consideration in such patients. With sudden onset of dyspnea and odynophagia, an impacted subglottic object may be present. If the object is known to be sharp and thin, the emergency physician should suspect embedding between the vocal cords or in the subglottic region, with resultant partial obstruction.44 Other components of the history may provide clues to airway foreign body presence and location. Even when the history cannot be obtained directly or does not suggest aspirated foreign object, the emergency physician can infer foreign body presence in certain patients. Trauma patients in the ED with injured and loose teeth may have aspirated in the field or during emergency laryngoscopy for oral intubation.42 The incidence of airway aspiration of avulsed teeth or prosthetic dental appliances is low (0.5% of 1411 facial trauma patients), but both the initial trauma and subsequent airway management pose risks for airway embarrassment owing to lodged dental matter.50 Besides the intubated or obtunded patient with only indirect historical evidence of aspiration, conscious and alert patients may not give a direct history of aspiration owing to lack of dramatic airway symptoms or remoteness of the aspiration event and secondary problems (e.g., pneumonia). In some cases, such as penetrating trauma or blast injuries, the patient may be unaware of the potential for aspiration and not attribute symptoms to this entity.40 Patients aspirating needles may have minimal or no symptoms, with chronic hemoptysis or odynophagia the only manifestation of these or similar foreign bodies.42 There is conflicting evidence regarding the role of neurologic disease in aspiration. Patients with deficits may be unaware or unable to report problems such as denture displacement; this inability has been associated with disastrous results in the case of airway obstruction from dental hardware.51 Neurologic impairment may result in atypical or absent histories in cases of foreign body aspiration.40 Reports of adult42 and pediatric49 series have identified little role, however, for neurologic impairment in foreign body aspiration. An atypical history is a concern in neurologically impaired patients, but the problem of foreign body aspiration with atypical history is uncommon in this patient population. The child with respiratory difficulty after eating can represent a diagnostic dilemma. Children with stridor or other respiratory symptoms may have esophageal bolus impaction. The pediatric trachea is soft, especially posteriorly, and may be compressed by a large esophageal body pressing anteriorly on the trachea. In addition, the trachea itself may be displaced anteriorly and kinked, causing a partial obstruction. Fever and localized infection may indicate bony aspiration (e.g., into the piriform fossa) that may occur when bone-containing foods are fed to very young children.52 Unfortunately, missed esophageal foreign bodies in children can result in long-term, yet mistaken, treatment for asthma (owing to wheezing and stridor from fistula formation).53 Cyanosis is present in 10% of patients, and coughing, audible wheezing, or overt respiratory distress occurs in 25 to 37% of patients with aspirated objects.42,43 Unilateral diminution of breath sounds, when present, is a useful identifier of aspirated foreign body.48 Patients may be stridorous or hoarse with upper airway foreign objects, and sternal retractions may be noted in patients with intratracheal foreign bodies.35 More than half of children in one series had initial oxygen saturation values of 95% or lower.42 Patients with secondary infection may have fever. Oropharyngeal examination may reveal a foreign body posteriorly or “donor sites” of fractured teeth. The examination should include a search for fractured or missing dental prostheses, which sometimes can be lodged in pharyngeal areas for days and can account for sudden deterioration in status when the airway becomes occluded, as can occur after coughing.51 Oropharyngeal examination frequently can be augmented by indirect or direct laryngoscopy or nasopharyngoscopy, but these procedures should be performed only if the emergency physician judges that procedural stress does not pose undue risk of airway compromise. Furthermore, laryngoscopy or nasopharyngoscopy should be undertaken only if definitive airway management equipment and expertise are readily available. The advantage of these modalities is that they allow excellent visualization of the proximal airway, which is important diagnostically and therapeutically. Indirect laryngoscopy can prove useful in detection of radiolucent structures. Assessment of the neck may reveal accessory muscle use. Tracheal palpation may reveal a thud, indicating movement of a mobile foreign body against the tracheal wall. Abnormal inspiratory sounds may be heard on tracheal auscultation.44 Coughing may result from local irritation caused by bronchial foreign bodies. Localized or apparently generalized wheezing is frequently auscultated in patients with lower respiratory tract foreign bodies.43 The emergency physician should keep in mind the dictum that “all that wheezes is not asthma.” If a mainstem bronchus is completely obstructed, breath sounds are absent on the involved side. Occasionally a foreign body acts as a one-way valve, allowing air into the lung during inspiration but permitting none to exit during expiration. The involved lung becomes hyperexpanded, which may be detected as hyper-resonance to percussion.
Foreign Bodies
Perspective
Principles of Disease
Eye
History
Physical Examination
Diagnostic Strategies
Management
Ear
History
Physical Examination
Management
Nose
History
Physical Examination
Diagnostic Strategies
Management
Airway
History
Physical Examination
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree