POSITIONING
• Important to prevent tissue & nerve injury, especially in pts with arthritis & spine dz
• Common peripheral nerve injuries occur with the following frequency:
ulnar > brachial plexus > lumbosacral root > spinal cord
• Supine—most surgeries, including knee, hip, pelvis, arm, hand, foot
• Prone—spine surgery
• Check pressure points—face/eyes, breasts/genitalia, abdomen, brachial plexus
• Endotracheal tube dislodgement & kinking can occur
• Stretcher should be immediately available if need to flip supine emergently
• ↑ risk of perioperative visual loss
• Associated with spinal surgery, although frequency is <0.2%
• Mechanism: Unknown, may include anterior & posterior ischemic optic neuropathy (A/PION) or central retinal artery occlusion (CRAO)
• Risk factors: Prolonged surgical time (>6 hrs) & blood loss (>40% EBV)
• Avoid direct pressure on eye orbits to ↓ risk of CRAO & venous congestion
• Lateral—neck, hip surgeries
• Need to protect pressure points & maintain neutral neck alignment
• Axillary roll ↓ brachial plexus & vascular compression in dependent arm
• Sitting/beach chair—shoulder, clavicle surgeries
• Provides full surgical access to the shoulder, ↑ risk of air embolism (5–25%)
Concern of hypotension causing stroke as brain perfusion is lowered
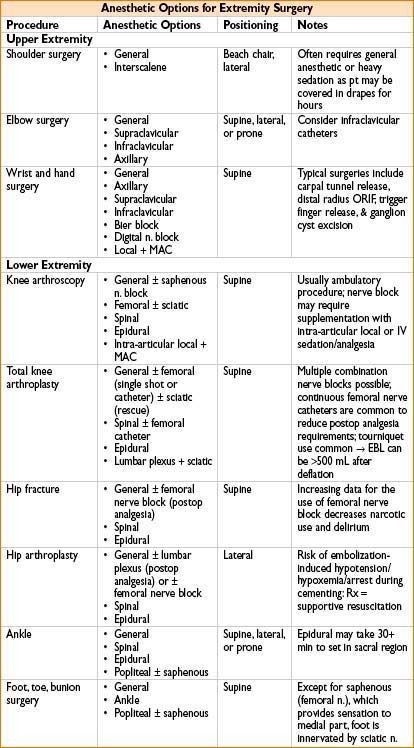
• Extremity Surgery(also see Chapter 6, on Regional Anesthesia)
• Consider regional anesthesia, especially continuous catheter techniques
• Combined general/regional may maximize speed, amnesia, & analgesia
• See table below, Anesthetic Options for Extremity Surgery
SPINE SURGERY
Cervical Spine Surgery
• Indications: Instability (trauma, tumor), arthritis/osteophytes, spinal stenosis
• Intubation precautions
• Consider fiberoptic intubation or techniques that avoid neck hyperextension (intubating LMA, videoscope) although almost all airway instrumentation does cause some degree of cervical spine movement. For extremely unstable spine, may even consider “awake” intubation or tracheostomy
• All laryngoscopies → neck extension; LMA placement may ↑ spinal cord pressure
Thoracic/lumbar Spine Surgery
• Laminectomy/laminotomy: Excision of vertebral lamina to relieve nerve pressure
• Fusion
• Instrumentation with hardware to stabilize spine until bony fusion (facilitated by inserted bone graft) can occur (6–12 mos postop)
• Indications: Spondylolisthesis, scoliosis, recurrent disc herniation, spinal instability
• Often large operations with large blood loss & periop complications
(Consider A-line, good IV access, blood & cell saver)
NEUROMONITORING (ALSO SEE CHAPTER 20)
• Indication: Detection of neural pathway compromise during surgery helps guide intraop surgical decision making
• Communication between surgeon, anesthesiologist, & neurophysiologist important
• Definition: Evoked potentials are measurements of nerve conduction in response to stimulation of a neural pathway
• Technique: Waveforms evaluated for amplitude, latency, & morphology; baseline measurements performed after anesthetic stabilized (avoid boluses/rapid changes in anesthetic depth → infusions can be beneficial)
• Outcomes: No evidence of improved outcomes in lumbar decompression or lumbar fusion for degenerative spine dz according to the American Assoc. of Neurological Surgeons/Congress of Neurological Surgeons
Types of Monitoring
Somatosensory Evoked Potentials (SSEP)
• Detect injury/ischemia to dorsal columns of spinal cord
• Stimulation of common peripheral nerves (posterior tibial, median, ulnar) recorded at scalp (sensory strip)
• Rare false negatives but common false positives
• Useful in monitoring compromise of blood supply to dorsal columns (sensory tract) supplied by posterior spinal arteries
• Does not directly monitor motor tracts (anterior spinal artery)
→ Motor injury possible with normal SSEPs
→ Artery of Adamkiewicz supplies lower 2/3 of spinal cord via anterior spinal artery
• Results may be delayed (20 min)
Corticospinal Motor Evoked Potentials (MEP)
• Used to monitor integrity of spinal cord motor tracts
• Used for aortic, intramedullary spinal cord tumor, spinal deformity, posterior fossa tumor, & intracranial aneurysms
• Useful in monitoring compromise of blood supply to anterior motor tracts supplied by anterior spinal artery
• Scalp or epidural lead placement to stimulate upper & lower extremities
• Muscle relaxants should be avoided
• Results immediate
• Safety issues: Burns, movement-induced injuries, seizures, bite injuries (0.2%), contraindicated with pacemakers
Electromyography (EMG)
• Measures electrical activity of muscles
• Used in tethered cord release, tumor excision, acoustic neuroma resection, & facial nerve procedures
• Also performed preoperatively with nerve conduction studies to help diagnose nerve compression injuries (carpal tunnel or sciatica) or neuromuscular diseases (myasthenia gravis, muscular dystrophy, ALS)
• Muscle relaxants should be avoided
Factors Affecting Monitoring
• Baseline measurements may be poor
• MEPs more sensitive to anesthetics than SSEPs
• Muscle relaxants relatively contraindicated in MEPs, but enhance SSEP signals by ↓ EMG artifact
• ↑ latency or ↓ amplitude may indicate neurologic dysfunction
• Bilateral & equal changes likely 2° to temp, hypotension, or anesthetic effects
• Unilateral changes likely 2° to ischemia/technical factors
• Temperature (SSEP): Hypothermia: ↔ amplitude, ↑ latencyHyperthermia: ↓ amplitude, ↔ latency
• Hypoxia(SSEP): ↓ amplitude, ↑ latency may ↑ amplitude early (injury potential)
• CO2 (SSEP): PaCO2 25–50 with minimal changesPaCO2 >100 ↓ amplitude, ↑ latency
• Anemia: ↓ amplitude
• Hypotension (SSEP): Rapid BP ↓ will ↓ amplitude, ↔ latency
• Anesthetic agent (SSEP); IV effects < volatile anesthetic effects
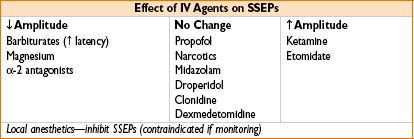
• Volatile anesthetics: Dose-dependent ↑ latency & ↓ amplitude
(N2O will depress monitoring, often more than volatiles)
• Anesthesia techniques in monitored surgeries (SSEP/MEP)
• Halogenated anesthetics vs. TIVA
• Propofol/narcotic (i.e., remifentanil) infusions have little or no interference with neuromonitoring (SSEP and MEP) at steady state
• Infusions can ↓ amount of volatile agent used to <0.5 MAC
• Deliberate hypotension
• Reducing MAP 20–30% below baseline to ↓ blood loss
• Techniques: Deep volatile anesthesia, β-blockers, arterial or venous vasodilators
• Risks: ↓ perfusion & O2 to vital organs (heart, brain, spinal cord)
• Frequent monitoring of pressure points needed
(↓ perfusion pressure may ↑ risk of pressure necrosis)
• Wakeup test
• Most reliable assessment of intact spine
• Involves gentle, slow wakeup with continued analgesia coordinated with surgical team following instrumentation
• Pt asked to follow commands upon emergence with reestablishment of general anesthesia after neuroassessment
• Plan should be outlined with pt prior to surgery
(explain possibility of intraoperative recall)
• Common techniques for rapid awakening include TIVA (propofol, remifentanil, and/or dexmedetomidine), N2O-narcotic, short-acting inhalational agent (desflurane)
COMPLICATIONS IN ORTHOPEDIC SURGERY
• Methyl methacrylate bone cement
• Polymer creates strong bond between bone & implanted hardware
• Expands into cancellous bone when applied, can result in ↑ intramedullary pressures → displacement of intramedullary fat → fat embolism
• Cement monomers can cause ↓ SVR/↓ BP if enters systemic circulation
• Signs: Hypoxia, ↓ BP, dysrhythmias, pulmonary HTN, ↓ cardiac output
• Therapy: High FiO2, euvolemia, & hemodynamic support
• Fat embolus syndrome (FES)
• Often occurs with long bone fractures and intramedullary reaming
• Risk ↑ 24-hr post-injury without proper bone fixation
• Signs: Skin petechiae, rash, urine fat globules, hypotension, tachycardia, hypoxia/dyspnea, altered mental status, lung infiltrates on CXR
• Therapy: Supportive to correct hypoxia & hemodynamic instability; intubation with PEEP for refractory hypoxemia; steroids controversial
• Management of blood loss in orthopedic surgery
• Autologous blood donation collected several weeks prior to elective procedure
• Preop erythropoietin
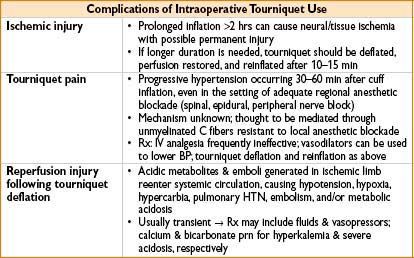
• Tourniquet for extremity surgery
• Application proximal to surgical site to ↓ blood flow (bloodless surgical field)
• Complications include ischemic injury, tourniquet pain, & reperfusion injury
• Relatively contraindicated in sickle cell pts (limb ischemia promotes sickling)
• Acute normovolemic hemodilution—pt’s blood collected at start of surgery with concomitant replacement with IV fluids; blood is returned to pt at end of surgery
• Intraoperative blood salvage/cell saver
• Antifibrinolytics—aminocaproic acid, tranexamic acid
• Deliberate hypotension
• DVT/PE
• Prophylaxis = best prevention
• Major cause of perioperative morbidity/mortality in orthopedic surgery
• Risk factors: Prolonged surgery, hip/knee replacement, tourniquet use, ↓ mobility postop
• With new anticoagulants (i.e., fondaparinux) used perioperatively, neuraxial techniques should be avoided and the risks of peripheral nerve blocks should be weighed with risks and benefits
• Encourage early ambulation/physical therapy
• Use intermittent leg-compression devices throughout perioperative period
• Initiate low-dose anticoagulation (warfarin/LMWH) preoperatively
• Consider prophylactic IVC filter in high-risk patients
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








