ATRIOVENTRICULAR CONDUCTION SYSTEM
• 1st-degree AV block—PR interval increased >0.2 sec
• 2nd-degree AV block
• Mobitz type I (Wenckebach)—AV delay (PR interval) increases with each beat, until QRS is dropped after P wave
• Treatment—only if symptomatic: Atropine, isoproterenol, permanent pace
• Mobitz type II—sudden unpredictable dropped QRS not associated with progressive PR interval prolongation
• Caution: May progress to 3rd-degree heart block
• Treatment—permanent pacemaker
• 3rd-degree AV block (complete heart block)
• No relationship between P wave & QRS—“AV dissociation”
• Treatment—permanent pacemaker
• Bundle branch block
• Right bundle branch block (RBBB)
• Examine QRS in V1 & V2
• Right ventricular depolarization delayed
• LBBB makes it difficult to determine infarction on ECG
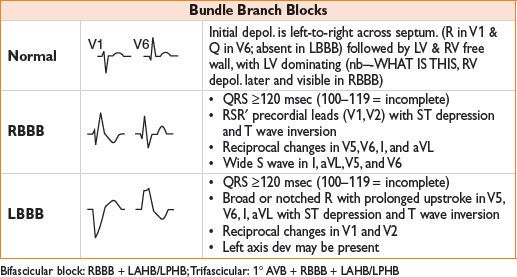
• Left bundle branch block (LBBB)
• Examine QRS in V5 or V6
• Left ventricular depolarization delayed
• Difficult to determine infarction on ECG
• Atrial flutter
• Regular atrial activity; 180–350 bpm; ventricular rate 150 bpm (2:1 AV block)
• ECG: “F waves,” “sawtooth” pattern, flutter waves
• Treatment
• Unstable → immediate electrical cardioversion
• Burst pacing (temporary or permanent pacemaker)
• Medical therapy (β-blockers, Ca2+-channel blockers)
• Radiofrequency catheter ablation (RFA)
• Atrial fibrillation
• Irregular atrial activity at 350–600 bpm, ventricular rate 160
• ECG: Wavy baseline, absent P waves
• Treatment
• Unstable → immediate electrical cardioversion
• Chemical cardioversion (Class IA, IV, III antiarrhythmics)
• Antiarrhythmic drugs
• Anticoagulation
• Rate control: β- or Ca2+-channel blockers, digoxin
• Maze procedure
• Paroxysmal SVT
• Ventricular rate 140–250 bpm
• ECG: Narrow complex, P waves hidden in QRS complexes (QRS may be slightly widened, not more than 0.14 sec)
• Treatment: Vagal maneuvers, β- or Ca2+-channel blockers, radiofrequency ablation
• AV reentrant tachycardia
• Wolff–Parkinson–White
• PR interval shortened, delta wave, wide QRS
• Treatment: β- or Ca2+-channel blockers, radiofrequency ablation
VENTRICULAR ARRHYTHMIAS
• Premature ventricular beats
• Widened QRS
• Couplet—two in a row; Bigeminy—every other beat is PVC
• Ventricular tachycardia—3 or more PVCs in a row, 100–200 bpm
• Nonsustained VT (NSVT)—persists for <30 sec
• Sustained VT—persists for ≥30 sec
• Treatment
• Symptomatic: Electrical cardioversion followed by antiarrhythmic drugs; follow ACLS protocol
• Asymptomatic NONSUSTAINED VT: β-blockers, implantable cardioverter-defibrillator (ICD) in pts at high risk
• Unstable: Defibrillation as if ventricular fibrillation
• Torsades de pointes
• Polymorphic VT with varying amplitudes of QRS twisting about the baseline
• Treatment: Magnesium 1–2 g IV followed by infusion
• Ventricular fibrillation
• Chaotic irregular appearance without discrete QRS waveforms
• Treatment: See ACLS protocol; ICD if arrhythmia not associated with acute MI
OTHER ECG ABNORMALITIES
Hypertrophy
• Right atrial hypertrophy
• Large, biphasic P wave with tall initial component
• ●Left atrial hypertrophy
• Large, biphasic P wave with wide terminal component
• Ventricular hypertrophy
• Right ventricular hypertrophy
• R wave >S in V1 (R wave becomes progressively smaller from V1 to V6)
• S wave persists in V5 & V6
• Right axis deviation with slightly widened QRS
• Rightward rotation in horizontal plane
• Left ventricular hypertrophy
• S wave in V1 + R wave in V5 >35 mm
• Left axis deviation with slightly widened QRS
• Leftward rotation in horizontal plane
• Inverted T wave that slants downward gradually but upward quickly
Electrolyte Imbalances
• Hypokalemia
• Flattened T wave
• U waves
• Hyperkalemia
• Peaked T waves
• Wide or flat P wave
• Wide QRS
• Hyper-/hypocalcemia
• Hypercalcemia—shortened QT
• Hypocalcemia—prolonged QT
Drug Effects
• Digitalis toxicity
• Inverted or flattened T waves
• Shortened QT interval
Pulmonary Embolism
• Right axis deviation
• Acute RBBB
• Inverted T waves in V1 to V4 from right ventricular overload
• Wide S in I large Q; and inverted T in III
Pericarditis
• Diffuse ST-segment elevation (looks similar to acute MI, usually more universal in nature)
• May see subsequent inverted T waves (similar to acute MI)
Hypothermia
• J wave or Osborne wave—J POINT ELEVATION WITH T WAVE INVERSION, ESPECIALLY IN THE SETTING OF SLOWED CONDUCTION
Biventricular Pacemaker
• Cardiac resynchronization therapy-–used to synchronize contraction of right and left ventricles to increase cardiac output in patients with heart failure.
Cardiac Transplantation
• 2 sets of P waves
• Increased SA node refractory period
• Prolonged atrial conduction
• 1st-degree AV block common
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








