Hyperthyroidism
Anesthesia for Hyperthyroidism
• Preop
• General: Euthyroid status preferred (risk of thyroid storm), check TFTs, continue antithyroid meds & β-blockers to the day of surgery
• Airway: Check for compression, tracheal deviation, & substernal thyroid mass consider awake fiberoptic intubation if airway looks challenging
• Benzodiazepines for preop sedation
• Intraop
• General: Avoid/use sympathetic nervous system stimulants cautiously
(epinephrine, ketamine, ephedrine, phenylephrine) → severe HTN/tachycardia
• Ensure patient eye protection (pt often have exophthalmos)
• Thiopental possesses antithyroid activity in high doses
• Watch for signs of thyroid storm (hyperthermia, tachycardia, ↑ BP)
• Autoimmune thyrotoxicosis may be associated with myopathies
• Postop
• Complications: Hormonal disturbances & airway management issues
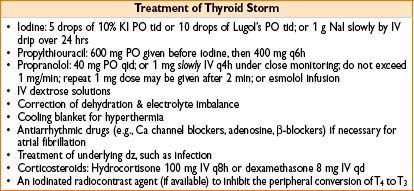
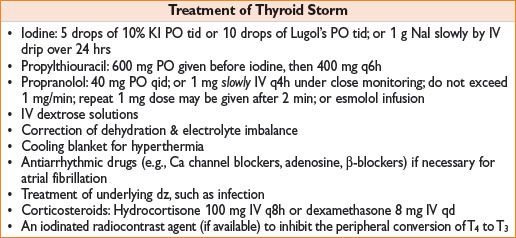
• Thyroid storm: Life-threatening condition, can develop 6–24 hrs after surgery; caused by massive release of T3 & T4
Signs: Tachycardia, fever, confusion, vomiting, dehydration, CHF, agitation
(unlike MH, not associated with ↑ CPK, muscle rigidity or acidosis)
• Parathyroid gland damage/removal → hypocalcemia in 24–72 hrs postop
• Recurrent laryngeal n. damage → causes hoarseness if unilateral, stridor if bilateral diagnosis by fiberoptic laryngoscopy
• Neck hematoma → partial/complete upper airway obstruction
Treatment = prompt opening of neck wound & drainage
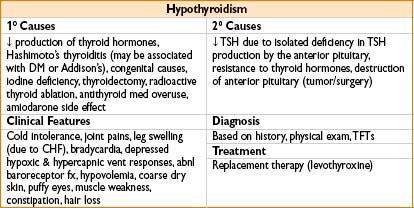
Hypothyroidism
Anesthesia for Hypothyroidism
• Preop
• Thyroid supplements should be continued through surgery
• Delay elective surgeries in case of untreated hypothyroidism (risk of cardiovascular instability & myxedema coma)
• Subclinical hypothyroidism not associated with ↑ surgical risk
• In emergency cases: Consider pretreatment with IV thyroxine & steroids
• Pts usually obese, may have large tongue, short neck, delayed gastric emptying
• Intraop
• Hypothyroid pts sensitive to narcotics & sedatives
• Induction: Maintain stable hemodynamics (consider ketamine or etomidate)
• Hypotension due to abnl baroreceptor fx, ↓ cardiac output, hypovolemia
• Hypothermia develops very fast & difficult to treat
• Metabolic disturbances common: ↓ Na & ↓ blood sugar
• Hypoventilation common (blunted response to hypoxia)
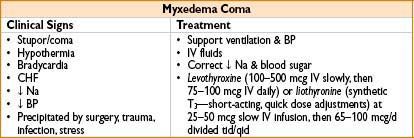
• Myxedema coma (severe form of decompensated hypothyroidism) can occur (see table below)
• Postop
• Hypothermia, slow drug metabolism, & resp depression may delay extubation
• Extubation should be done in awake & normothermic pt
• Regional anesthesia & ketorolac = preferable for pain control (use opioids with caution)
PARATHYROID GLANDS
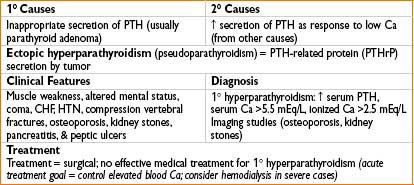
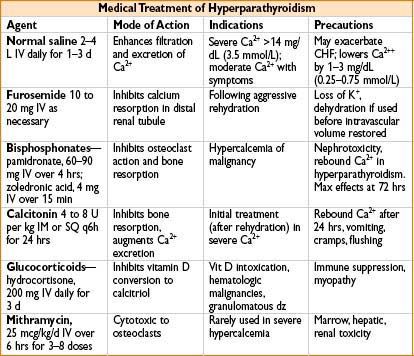
Hyperparathyroidism
Anesthesia for Hyperparathyroidism
• ECG: Short PR & QT intervals, cardiac conduction disorders (↑ Ca levels)
• Maintain hydration & good urine output
• Consider using lower doses of nondepolarizing muscle relaxants in weak/somnolent pts
Hypoparathyroidism
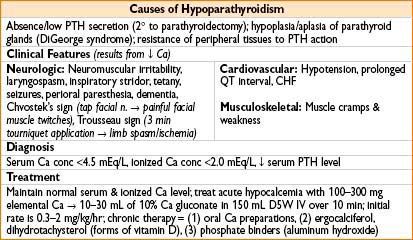
Anesthesia for Hypoparathyroidism
• Preop—serum & ionized Ca should be normalized, especially for pts with cardiac symptoms
• Intraop—preexisting hypocalcemia may augment neuromuscular block
• Blood products containing citrate (as well as 5% albumin) will ↓ serum Ca level
• Postop—hypocalcemia may cause prolonged recovery from neuromuscular blockade
Pheochromocytoma
• May be associated with autosomal dominant multiple endocrine neoplastic synd (MEN types 2a & b)
• Secretes epinephrine, norepinephrine, & occasionally dopamine
• Secretion may be intermittent or continuous
• Change in tumor blood flow, direct pressure, & meds can trigger catecholamine release
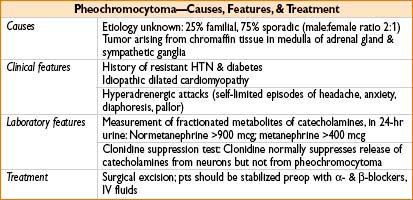
Anesthesia for Pheochromocytoma
• Preop: Goal = control BP & restore of intravascular volume
• Start α-blockade 10–14 d prior to surgery & prior to β-blockade
• If one accidentally starts β-blockade prior to α-blockade → severe HTN from unopposed α-stimulus
• Phenoxybenzamine = α-antagonist of choice (another option is prazosin)
• Starting dose = 10 mg qd or bid, then inc dose by 10–20 mg in divided doses every 2–3 d as needed to control BP (goal final dose = 20–100 mg qd)
• Propranolol 10 mg qid (should be initiated 3–4 d prior to the surgery)
• Ca-channel blockers—nicardipine 30 mg bid to supplement α- and β-blockade if BP is poorly controlled
• Hydrate all patients with pheochromocytoma—carefully in pts with signs of CHF
• Nitroprusside infusion (also phentolamine IV) for treatment of acute HTN crisis
• Metyrosine—catecholamine synthesis inhibitor, sometimes used preop
• Intraop
• GA vs. regional—no influence on patient outcome
• Avoid desflurane, sympathetic stimulants (ketamine, ephedrine), & hypoventilation (cause nonneurogenic release of catecholamines), atracurium & morphine (histamine release)
• Prepare nitroprusside & phenylephrine infusions in advance
• A-line before induction, ± central line (assessment of intravascular volume), ± PA line
• Gentle induction—intubation may cause massive release of catecholamines
• Tumor manipulation—may cause massive catecholamine release → HTN crisis
• Suprarenal vein ligation → acute drop in blood catecholamine level → cause hypotension (treat with fluid administration and direct sympathomimetics)
• Catecholamine-resistant vasoplegia: Can also use vasopressin to reverse
• Refractory tachycardia: Treat with esmolol (25–300 mcg/kg/min)
• Postop
• Maintain normal BP; in about 50% pts BP will remain elevated
• Bilateral adrenalectomy → steroid support may be necessary
DIABETES
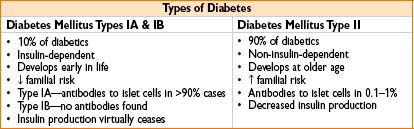
Anesthesia for Diabetes
• Preoperative
• Check type, duration, and severity of diabetes—the more severe, poorly controlled and longstanding is the disease, the higher is the risk of long-term complications
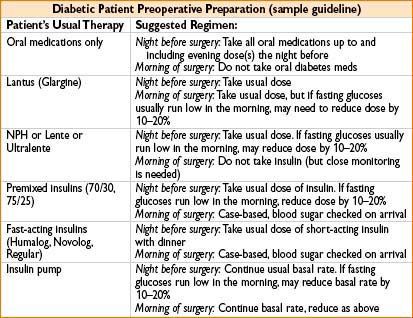
• Check current therapy for type and dose (diet, oral hypoglycemic drug or insulin)
• Morning blood sugar and HbA1c assay help to assess status of diabetic control. Creatinine level and electrolytes may reflect degree of nephropathy
• Check for the presence of coronary artery disease, HTN, cerebrovascular disease and peripheral vascular disease, check EKG for presence of rhythm disturbances and prior MIs
• Consider Na bicitrate and metoclopramide in pts with GERD and gastroparesis
• Severe peripheral neuropathy may preclude use of regional anesthesia
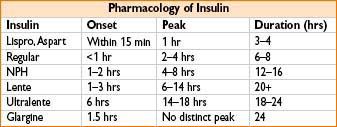
• Long-acting insulins should be stopped and substituted by protamine and lente insulins
• Long-acting sulfonylurea drugs such as chlorpropamide should be stopped and substituted by short-acting agents. Metformin stopped if concern for intraop metabolic acidosis. Type-2-diabetic patients with marked hyperglycemia on oral treatment should be switched to insulin before operation
• Emergency surgery
• Stabilize metabolic control/volume status as much as possible (delay surgery if possible)
• Maximize glucose, electrolyte, acid–base status—insulin & glucose infusions
• Saline infusion if volume is depleted (depending on renal function & cardiac status)
• K+ infusion if renal function is normal & serum K+ normal or low
• Bicarbonate infusion only in pts with severe acidosis
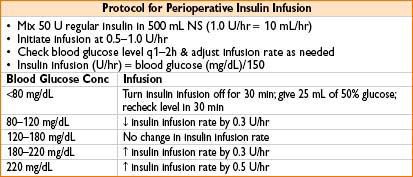
• Intraoperative management
• Monitoring blood sugar = mandatory for all insulin dependent pts & poorly controlled pts
• Pts on NPH (neutral protamine Hagedorn) or PZI (protamine zinc insulin)
• ↑ risk for anaphylactic protamine reactions (2° to prior sensitization)
• Insulin requirements in diabetics vary during surgery; must individualize
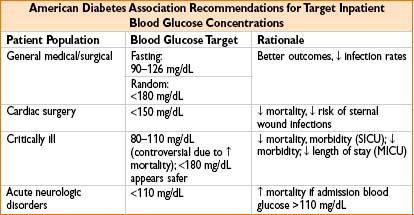
• Postop
• Treat N/V in pts with gastroparesis with metoclopramide as pts have increased risk of infection, MI, hyper/hypoglycemia, CV, and renal dysfunction
• Diabetic emergencies
• Diabetic ketoacidosis: Usually triggered by trauma or infection in Type I DM
• Nausea, vomiting, dehydration, polyuria, polydipsia, somnolence → coma
• Hyperglycemia, wide anion gap metabolic acidosis, ketones in blood & urine, ↓ K+
• Management: Place A-line, consider intubation for severe CNS depression
• Start insulin infusion (10 U IV, then 5–10 U/hr)
• Normal saline at 5–10 ml/kg/hr (fluid deficit of 3–8 L not uncommon) add 5% glucose when blood sugar <250 mg/dL
• Replenish K (0.3–0.5 meq/kg/hr)
• Bicarbonate not usually required
• Hyperosmolar, hyperglycemic, nonketotic coma (usually type II DM)
• Severe dehydration & associated with acute hyperglycemia (>600 mg/dL)
• Treatment: Correct hypovolemia & hyperglycemia
Fluid resuscitation with 0.45% saline
Give 10 U regular insulin IV stat → insulin drip (see protocol above)
• Hypoglycemia—result of stress, missed meal, exercise, alcohol consumption
• Hypoglycemia is much more dangerous in unconscious pt than hyperglycemia (safer to err on the side of hyperglycemia)
• Symptoms: Diaphoresis, tachy, impaired cognition, confusion, loc & seizures
• Treatment: 50% IV glucose, initial dose 25 mL
ADRENAL INSUFFICIENCY
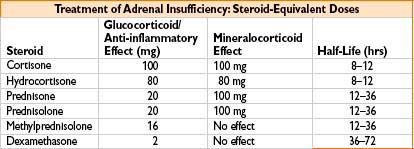
Anesthesia for Adrenal Insufficiency
• Preop—administer stress dose of corticosteroid (usually 100 mg hydrocortisone IV)
• Intraop
• Risk of poor fluid loading tolerance, hypoglycemia, ↑ K+, dysrhythmias
• Unexplained hypotension (that is unresponsive to fluids & vasopressors)
→ Treat with glucocorticoid
• Avoid etomidate (suppresses adrenal function)
• Postop
• Provide adequate corticosteroid supplementation
Excess of Corticosteroids (Cushing’s Syndrome)
• Causes
• 1°—Adrenal adenoma/hyperplasia
• 2°—ACTH-secreting pituitary microadenoma (Cushing’s dz), ACTH-secreting tumors, exogenous steroid usage
• Clinical features: Moon facies, buffalo hump, central obesity, hirsutism, skin atrophy, osteoporosis, easy bruising, diabetes, proximal myopathy, aseptic hip necrosis, mental status changes, pancreatitis, polyuria/polydipsia
Anesthesia for Cushing’s Syndrome
• Preop: Risk of hypokalemia & glucose intolerance (check both)
• Cushingoid pts may have HTN, CHF, fragile skin, osteoporosis
• Use stress dose steroids in case of iatrogenic Cushing’s syndrome
• Intraop
• Obese (potentially difficult airway/IV access), often HTN
• Special attention to positioning (skin breaks down easily)
• High-dose opioids may cause resp depression & difficulty with extubation
• Postop course
• Poor ventilatory performance (↓ FRC), poor mobilization, pressure sores, ↑ infections
Hyperaldosteronism (Conn’s Syndrome)
• Causes
• 1°—(Conn’s syndrome) excess secretion of aldosterone by an adrenal adenoma (60%), bilateral adrenal hyperplasia (30%), carcinoma (rare)
• 2°—high plasma levels of renin & aldosterone (due to CHF/liver cirrhosis)
• Clinical features
• Malignant HTN (centrally mediated or aldosterone-induced)
• ↓ K+ often severe & may be exacerbated by diuretics → weakness & tetany
• HTN pts often hypovolemic (hypovolemia & ↓ K+ indicate severe total K+ deficit)
• Metabolic alkalosis from H+ loss
Anesthesia for Conn’s Syndrome
• Preop: Correct ↑ BP, metabolic alkalosis, hypokalemia
• Spironolactone (up to 400 mg qd) may control HTN & moderate hypovolemia/ ↓ K+
• Intraop: If CHF, uncontrolled HTN, hypovolemia present → place A-line
• Surgical manipulation of adrenal may release catecholamines → CV instability
• Give corticosteroid & mineralocorticoids in cases of bilateral adrenalectomy
• Postop: Goal = maintain normal BP, electrolyte balance
• Continue corticosteroid & mineralocorticoids in cases of bilateral adrenalectomy
POSTERIOR PITUITARY GLAND
• Posterior pituitary releases oxytocin & antidiuretic hormone (ADH, vasopressin)
• ADH stimulates kidneys to conserve water
• Low ADH → diabetes insipidus
• High ADH → syndrome of inappropriate antidiuretic hormone (SIADH) secretion
Diabetes Insipidus (DI)
• Causes: Central DI—insufficient ADH by pituitary (damage from head injuries, genetic disorders, infections, vascular dz, tumors)
• Nephrogenic DI—lack of kidney response to ADH (from drugs, chronic kidney dz)
• Clinical features: Thirst, polyuria (up to 20 L/d), low BP, & dehydration
• Diagnosis: Urine specific gravity of ≤1.005, urine osmolality <200 mOsm/kg, random plasma osmolality > 287 mOsm/kg
• Treatment: SQ/nasal/PO vasopressin analogues (desmopressin), chlorpropamide, carbamazepine, thiazide diuretics
• Anesthetic management
• Preop—restore intravascular volume, nasal desmopressin 10 mcg bid–tid
• Intraop
• Total lack of ADH: 100 mU vasopressin before surgery followed by infusion (100–200 mU/hr titrated to urine output)
• Partial ADH deficiency: No vasopressin (unless plasma osmolality >290)
• Postop—continue desmopressin & monitor electrolyte balance
Syndrome of Inappropriate Antidiuretic Hormone (SIADH) Secretion
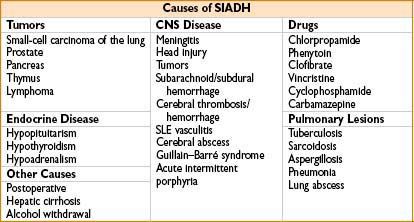
• Clinical features: ↓ Na superimposed upon symptoms of underlying pathology
• ↓ Na due to a dilutional effect, not Na depletion (may be no clinical symptoms)
• Symptoms: May include nausea, weakness, anorexia; Na <110 mmol/L → coma
• Diagnosis: Must distinguish SIADH from other causes (such as dilutional hyponatremia) (causes of dilutional ↓ Na: Excess infusion of dextrose/saline drips/use of diuretics)
• Diagnosis confirmed by serum Na <130 mmol/L, plasma osmolality <270 mOsm/L, urinary Na >20 mEq/L & elevated urine osmolality
• Treatment: Address underlying problem
• Release of ADH (from hypophysis or tumor) cannot be suppressed by medical therapy
• Symptomatic relief: Water intake restriction to 500–1000 mL per 24 hrs
(plasma & urine osmolality should be measured regularly)
• Fluid restriction may not be appropriate in SAH—may promote vasospasm
• Demeclocycline: When fluid restriction is difficult
• Anesthetic management
• Correct hyponatremia, monitor volume status by CVP or PA catheter
• Monitor electrolytes (urine osmolarity, plasma osmolarity, serum Na) (including immediately after surgery)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








