Cardiac Cycle: Definitions & Equations
• Systole = isovolumic ventricular contraction & ejection
• Diastole = isovolumic ventricular relaxation & filling
• Cardiac output = stroke volume × heart rate
→ volume of blood pumped by each ventricle per minute
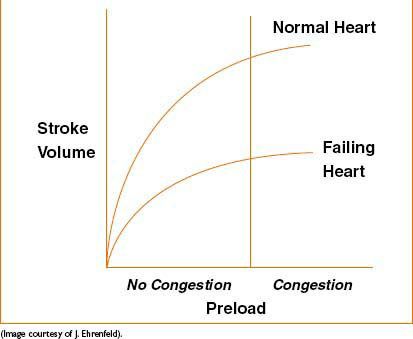
Figure 16-1. Frank–Starling relationship.
• Stroke volume = amount of blood pumped out of each ventricle with each contraction
• Cardiac reserve = difference between cardiac output at rest & the max volume of blood the heart is capable of pumping per minute
• Preload = volume of blood in ventricle before systole, used to estimate left ventricular end diastolic volume (LVEDP)
• Starling’s law = contractility depends on muscle fiber length
• Afterload = resistance to ejection of blood by each ventricle
• Coronary perfusion pressure (CPP) = aortic diastolic BP – LVEDP
• Left ventricular wall tension → Law of Laplace: T = p × r/(2 × t) where T = wall tension, p = pressure, r = radius, t = wall thickness
• Fick equation:
Cardiac output (C.O.) = O2 consumption/([arterial O2 content] – [venous O2 content])
COMMON DISEASE STATES AFFECTING THE HEART
Determinants of Myocardial Perfusion
Supply: CPP, HR, PaO2, coronary artery diameter
Demand: Myocardial O2 consumption, HR, LV wall tension, contractility, conduction, relaxation
Hypertension (HTN)
• Definition: >140/90 or 130/80 in high-risk pts
• Essential HTN (1° HTN)—no definable cause (95% of pts)
• 2° HTN: Iatrogenic (meds), renal, aortic coarctation, pheochromocytoma, adrenocortical hormone excess, thyroid hormone abnormal, estrogen therapy, Cushing’s disease
• Consequences of HTN
• Organ damage: Ventricular hypertrophy, systolic dysfunction, CAD, stroke, abd aortic aneurysm, aortic dissection
• Hypertensive crises: HTN encephalopathy—headache, blurred vision, confusion, somnolence, coma
• Treatment: Diuretics, sympatholytic agents (β-blockers/α-2 agonists/α-1 antagonists), vasodilators, (Ca-channel blockers, ACE inhibitors, ARBs), nitrates
• Anesthetic considerations
• Monitoring: BP cuff vs. arterial line as indicated
• Goal: Keep BP within 20% of baseline
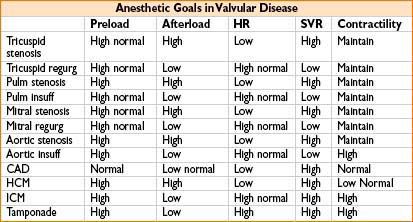
Valvular Disease
Mitral Stenosis
Causes: Rheumatic fever, congenital stenosis
Pathophysiology
• ↑ LA pressure → pulmonary edema, LV hypertrophy
• Atrial fibrillation may result from LA dilation, LA thrombus from stasis of flow
• Develop pulmonary HTN
• Atrial kick provides 40% of LV filling
• Stroke volume is fixed
Clinical feature
• High-pitched “opening snap” followed by low-frequency diastolic rumble
Classification
• Mild = valve area of ≤2 cm2; critical = valve area ≤1 cm2
Treatment
• Medical therapy; balloon mitral valvuloplasty; open mitral commissurotomy; mitral valve replacement
Anesthetic management
• Maintain sinus rhythm (atrial kick provides 40% vent filling)
• Maintain preload & SV to avoid drop in SVR
• Maintain normal HR (to allow time for filling)
• Prevent ↑ in PVR (avoid hypoxia, hypercarbia, acidosis)
Mitral Regurgitation
Causes: Myxomatous disease (mitral valve prolapse [MVP]), ischemic heart dz, heart failure, annular dilation, endocarditis, rheumatic heart dz, hypertrophic cardiomyopathy (SAM), myocardial infarction (necrotic papillary muscle, ruptured chordae)
Pathophysiology
• Severity determined by
• Systolic pressure gradient between LV and LA
• Systemic vascular resistance opposing forward LV blood flow
• Left atrial compliance
• Duration of regurgitation with each systole
• Regurgitant fraction = volume of MR/total LV stroke volume (>0.6 = severe)
• Acute MR: ↑ pulmonary pressure & pulmonary congestion
• Chronic MR: ↑ LA size & compliance
Clinical features
• Apical holosystolic murmur radiating to axilla
Treatment
• Medical therapy; mitral valve repair/replacement
Anesthetic management
• Maintain HR normal or high
• Avoid myocardial depression
• Avoid ↑ SVR (can worsen regurgitation)
• Initiate prophylaxis against endocarditis
• PA catheter v waves increase as regurgitant fraction increases
Aortic Stenosis
Causes: Bicuspid AV, senile degenerative disease, rheumatic fever
Risk factors: Male gender, hypercholesterolemia, smoking
Pathophysiology
• Blood flow across valve is obstructed during systole
• Concentric LV hypertrophy
• Dependence on atrial kick to fill stiff ventricle
• Stroke volume is fixed
• Compression of subendocardial vessels → ischemia
Symptoms & severity
• Angina—median survival 5 yrs
• Syncope—median survival 3 yrs
• Congestive heart failure—median survival 2 yrs
Clinical features
• Harsh, holosystolic, crescendo–decrescendo murmur
Classification
• Mild = valve area <2.5 cm2, moderate = 0.7–1.2 cm2, critical <0.7 cm2
Treatment
• Percutaneous balloon valvuloplasty, percutaneuous, transapical, or open aortic valve replacement
Anesthetic management
• Maintain sinus rhythm (atrial kick provides 40% of preload)
• Maintain HR slow to normal (allow time for ventricular filling)
• Avoid ↓ SVR (will ↓ CO because of fixed SV)
→ because of this, severe AS is a relative contraindication to spinal anesthesia
• Initiate prophylaxis against endocarditis
• Avoid myocardial depression as stroke volume is fixed
• Consider arterial line placement for severe AS
• Consider percutaneous pacing capability in case of cardiac arrest (chest compressions usually ineffective)
Aortic Regurgitation (AR)
Causes: Leaflet abnormalities (rheumatic heart dz, endocarditis, bicuspid valve), dilation of aortic root (aortic aneurysm/dissection, Marfan syndrome, syphilis, cystic medial necrosis)
Pathophysiology
• Acute = surgical emergency—sudden ↑ LV diastolic pressure rise backs up to pulm circulation causing pulm congestion, acute pulm HTN, & edema
• Chronic—LV compensates with dilation & hypertrophy → heart failure
Clinical features
• Bounding pulses
• Austin Flint murmur—turbulent flow across mitral valve during diastole due to AR jet
Treatment
• Asymptomatic—nifedipine, ACE inhibitor, diuretics
• Symptomatic—aortic valve replacement
Anesthetic management
• Maintain sinus rhythm
• Maintain normal to high normal heart rate
• Avoid ↑ SVR (will worsen regurgitant fraction)
• Avoid myocardial depression
• Initiate prophylaxis against endocarditis
• Consider vasodilators (nitroprusside) to ↓ afterload
Pulmonic Stenosis
Causes: Congenital deformity, carcinoid heart disease
Classification
• Mild: Pressure gradient <40 mm Hg, moderate 40–80 mm Hg, severe >80 mm Hg
Treatment
• Balloon valvuloplasty; valve replacement
Pulmonic Regurgitation
Causes: Annular dilation 2° enlarged pulm artery in pulm HTN, congenital/carcinoid heart dz
Tricuspid Stenosis
Causes: Congenital, rheumatic heart dz, right atrial tumor, endocarditis
Tricuspid Regurgitation
Causes: Congenital, endocarditis, carcinoid heart dz, secondary event from mitral valve or left-sided heart dz
Hypertrophic Cardiomyopathy (HCM)
Causes: Genetic, mixed, acquired
Pathophysiology
• LV outflow obstruction (asymmetrical hypertrophic septum interferes with LV ejection)
• LVH & RA enlargement, ↑ myocardial O2 consumption
→ subendocardial ischemia
Clinical features
• Mitral regurgitation from SAM (systolic anterior motion of anterior mitral leaflet)
• ↑ risk of sudden death
Anesthetic management
• Maintain slow HR (to allow for ventricular filling)
• Maintain sinus rhythm
• Maintain low to normal contractility (can cause/exacerbate SAM)
• Maintain preload & afterload
• Treatments include β-blockers, verapamil, pacing, ICD, surgical myectomy
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








