113 Fluids and Electrolytes in Children
 Body Water Distribution in Children
Body Water Distribution in Children
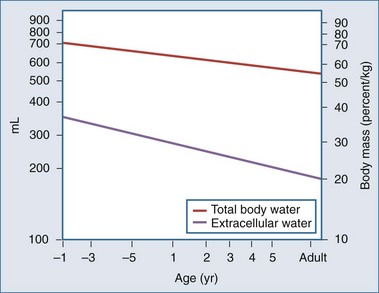
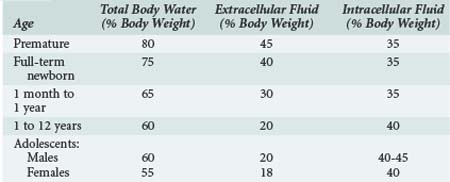
Body water content changes significantly with age in children.1,2 Total body water (TBW) is high in the fetus and preterm infant. During early fetal life, TBW represents 90% of total body weight, with 65% being in the extracellular fluid (ECF) compartment. By term, ECF and intracellular fluid (ICF) volume has fallen to 45% and 30% of TBW, respectively (Figure 113-1). The preterm infant has a relative expansion of both TBW and ECF volume expansion, and a diuresis in the first few days of postnatal life is a common finding. Fractional excretion of sodium is inversely correlated with age in the preterm, who is susceptible to both sodium loss and sodium and volume overload.3 In addition, glomerular filtration rate is lower than in the term infant, and the large surface area–to–body weight ratio leads to considerable evaporative losses.4–7 Further discussion of fluid and electrolyte physiology in the preterm infant is beyond the scope of this chapter.
Significant changes occur in TBW over the first year of life, from 75% of body weight at birth to 65% at 6 months and 60% at 1 year (Table 113-1). Some of this is accounted for by an increase in body fat. By puberty, TBW is approximately 60% of body weight in males, with a slightly lower percentage in females. Extracellular fluid volume decreases over the first year of life to 30% of TBW and decreases with age thereafter, reaching adult values early in childhood. The relatively high ECF volume in infancy is largely due to the larger interstitial lymph space. In contrast, the ICF volume remains relatively constant during childhood.
 Fluid Homeostasis in Children
Fluid Homeostasis in Children
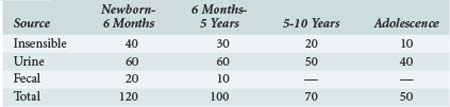
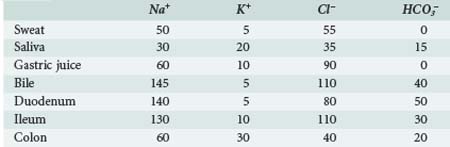
To achieve normal fluid homeostasis, fluid intake must balance losses. The latter consist of urine output plus insensible losses (evaporative from the skin surface and respiratory tract), with the addition of fluid loss in the stool, which in the absence of diarrhea should be minimal. Insensible losses are mainly in the form of electrolyte-free water (EFW) from the respiratory tract (15 mL/100 kcal/d). This loss is eliminated during positive-pressure ventilation. Sweat contains mainly water with a small amount of sodium, except in situations where sweat glands contain excessive amounts of sodium, such as in patients with cystic fibrosis. Evaporative losses also increase with elevations in body temperature; during thermal stress, water losses may increase to as much as 25 mL/100 kcal/d (Table 113-2).
Obligate water excretion in the urine is dependent upon solute load and the ability to concentrate and dilute urine. The average osmolar excretion in newborn infants receiving infant formula is 16 to 20 mOsm/kg/d.2 Infants are somewhat disadvantaged compared to the older child and adult in that they cannot maximally dilute (infant 200 mOsm/L versus adult 80 mOsm/L) and concentrate urine (infant 800 mOsm/L versus adult 1200 mOsm/L). In addition, the infant’s high metabolic rate and the solute load from enteral feeding formula means they require more water excretion per unit solute amount. High solute load and limited urine concentrating ability makes them prone to significant ECF contraction (dehydration) when there are excessive amounts of water loss. Typically this occurs in gastroenteritis, where reduced oral intake is combined with excessive water and electrolyte loss in the stool.
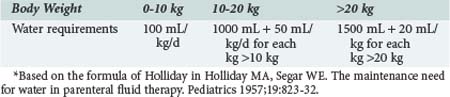
In the normal healthy individual, water intake is regulated by thirst stimulated via osmoreceptors in the hypothalamus. Infants and small children are unable to regulate their intake because they do not have access to water for the same reasons that apply in older children or adults in coma or with reduced levels of consciousness. When oral intake is replaced by parenteral fluids in children, the amount of fluid (i.e., water) given depends on body weight and energy expenditure. In 1957, Holliday8 published a formula that linked body weight to energy expenditure (Table 113-3). An allowance of 100 mL/100 kcal/d was made for insensible water loss, with 66.7 mL/100 kcal/d to replace urine output. Factoring in water of oxidation of 16.7 mL/100 kcal/d leaves a total of 100 mL/100 kcal/d for replacement of normal losses. The estimates for Na (3 mmol/100 kcal/d) and K (2 mmol/100 kcal/day) in maintenance fluids were calculated from the sodium and potassium concentration of cow’s milk and breast milk.
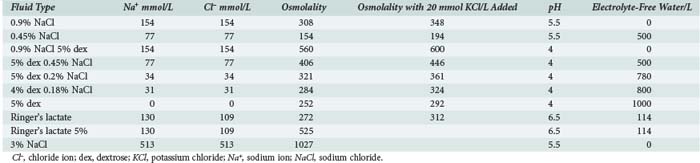
This paper by Holliday became the standard reference text for parenteral fluid administration in pediatrics. Although convenient and simple to use, the assumptions made about daily requirements for sodium, potassium, and EFW mandate the use of hypotonic intravenous (IV) solutions, which has been almost universal practice in pediatric medicine for almost 50 years (Table 113-4). However, nonphysiologic stimuli for antidiuretic hormone (ADH) secretion, which inhibits excretion of EFW (e.g., pain, anxiety, narcotics, positive-pressure ventilation), are common in critically ill patients. It is therefore not surprising that mild degrees of hyponatremia are a common finding in pediatric patients receiving parenteral fluid therapy. In a study by Gerigk9 of 103 children admitted to the hospital with acute medical illnesses, the median plasma Na value was 136 mmol/L, with plasma ADH levels that were higher than would be expected for that degree of hyponatremia. In 31 control patients (elective surgical admissions), median serum Na levels were 139 mmol/L, with lower ADH levels. We have made a similar observation in patients with hospital-acquired hyponatremia, who received twice as much EFW compared with a control group.10 The nonphysiologic secretion of ADH has been reported in association with many acute medical illnesses including meningitis, bronchiolitis, encephalitis, traumatic brain injury, and gastroenteritis.11–22 An increasing number of publications are now recommending the use of isotonic or near-isotonic fluids for standard maintenance in pediatrics to avoid administration of EFW, which is potentially hazardous in situations where ADH secretion is not inhibited.10,23–26 Hypotonic fluids should be reserved for patients with a demonstrated need for EFW (serum Na+ > 145 mmol/L).
 Perioperative Fluid Management
Perioperative Fluid Management
Standard practice in perioperative fluid management has been to replace intravascular volume loss with blood or colloid solutions and to use electrolyte solutions to provide for ongoing fluid requirements, replacement of losses from exposed serosal surfaces in open body cavities in thoracic and abdominal surgery, and losses from third-space fluid sequestration (Table 113-5). Extra fluid is also frequently administered to treat hypotension due to the vasodilating effects of anesthetic agents. The preferred electrolyte solution used by most anesthesiologists for intraoperative fluid administration is now Ringer’s lactate or isotonic saline because of concerns about the development of postoperative fluid retention and hyponatremia associated with elevated ADH levels.27–29 The potential for this is increased when hypotonic dextrose/saline solutions are used.28,30–32 This inability to excrete a sodium-free water load is amply illustrated in scoliosis surgery, where patients seem to be particularly at risk for the development of hyponatremia postoperatively.33 Two nonrandomized studies have shown that the degree of hyponatremia is less when isotonic or near-isotonic solutions are used.34,35 In a nonrandomized trial, Burrows35 compared Ringer’s lactate with 0.2% sodium chloride (NaCl) infusion in a group of children following scoliosis surgery. He found that the postoperative plasma Na level fell in both groups, but that the reduction was marked in those patients receiving the hypotonic fluid. Although at first glance, the explanation for this is EFW retention due to nonphysiologic stimulation of ADH secretion, it does not explain the reduction in plasma Na seen with Ringer’s lactate.
Further insights to explain this observation come from the study by Steele,36 where plasma and urine Na were measured in adult patients undergoing elective surgery, all of whom received Ringer’s lactate as their perioperative fluid. They found that the urine Na concentration was consistently above 150 mmol/L and as high as 350 mmol/L in some instances. This was associated with a significant positive water balance and a fall in the plasma Na, a process they termed postoperative desalination. In a similar study of children undergoing elective surgery, all of whom received Ringer’s lactate, we found similar levels of urinary Na loss (unpublished observations). We think that this desalination process is consistent with the kidney’s attempts to deal with a volume overload situation after the vasodilating effects of anesthetic agents are no longer present, but ADH is still being actively secreted. In this situation, it would be unwise to prescribe hypotonic fluids in the postoperative period and impose an extra burden of more EFW to be excreted by the kidney.
Further evidence has now emerged that supports the use of isotonic rather than hypotonic fluid in the perioperative period. A prospective observational study in patients admitted to the intensive care unit (ICU) postoperatively documented an increased risk of development of hyponatremia associated with use of hypotonic saline; water retention and increased sodium excretion are to blame.37 Two recent prospective randomized trials have compared the use of isotonic with hypotonic saline. Both have shown that the incidence of hyponatremia was significantly reduced with isotonic saline, and in neither study did the patients develop hypernatemia.38,39
 Disorders of Sodium Homeostasis
Disorders of Sodium Homeostasis
Hyponatremia
Hyponatremia (serum Na <136 mmol/L) is the commonest electrolyte disorder seen in a hospitalized population and implies an expansion of the ICF compartment. It is caused by either water gain (e.g., use of hypotonic fluids) or salt loss (e.g., gastroenteritis) (Table 113-6).
TABLE 113-6 Principal Causes of Hyponatremia
| Water Gain |
| Salt Loss |
Acute hyponatremia, defined as a fall in plasma Na to less than 130 mmol/L within 48 hrs, leads to rapid movement of water from the ECF to the ICF compartment and can cause cerebral edema, with catastrophic outcomes reported in children.30,40,41 Clinical findings are those of raised intracranial pressure (nausea, vomiting, headache), frequently undiagnosed until the onset of seizures. This is usually followed by apnea, indicating that brainstem coning has occurred. Symptomatic hyponatremia rarely occurs below a serum Na level of 125 mmol/L, but when it does, it constitutes a medical emergency. The primary objective is to raise serum Na to above this level to prevent brainstem herniation. This can be most effectively achieved with the use of hypertonic saline.42 Once this threshold has been reached, the serum Na can be allowed to correct by fluid restriction with or without the use of furosemide. IV mannitol has also been used successfully in the emergency treatment of acute symptomatic hyponatremia.43
Chronic hyponatremia is a common finding in patients with heart failure and renal failure and is associated with increased TBW and salt retention. It is not associated with cerebral edema, but correction of chronic hyponatremia with isotonic or hypertonic saline has been associated with central pontine demyelination.44–46
Hypernatremia
Hypernatremia is defined as a serum Na greater than 145 mmol/L and is caused by either water deficit or salt gain (Table 113-7). The former is seen in infants with severe gastroenteritis with a loss of water in excess of sodium, sometimes compounded by increased solute intake from incorrect mixing of infant formula. The absence of ADH secretion causing diabetes insipidus is seen in patients with pituitary tumors, traumatic brain injury, and central nervous system (CNS) infections.47–50 Water loss in critically ill children may also be associated with the use of loop diuretics or mannitol. Hypernatremia secondary to salt gain is seen with the excessive use of isotonic or hypertonic saline solutions or with the administration of IV bicarbonate.
TABLE 113-7 Causes of Hypernatremia
| Water Loss |
| Salt Gain |
A rise in serum Na is associated with movement of water from the ICF to the ECF compartment and development of a hyperosmolar state. Brain cells adapt with an increase in electrolytes and “ideogenic” osmoles (inositol, taurine), which tends to mitigate the fluid shift with partial restoration of intracellular osmolality and brain cell volume.51–53 Levels of Na over 155 mmol/L are frequently associated with abnormal CNS findings, and there is an increased risk of subdural hemorrhage and infarction in infants with hypernatremic dehydration and serum Na levels higher than 160 mmol/L.54–57 There is also the added danger of development of brain edema during the attempt to correct these hyperosmolar states rapidly, using solutions that are hypo-osmolar compared to the ICF compartment.58–63 Published recommendations suggest that the rate of correction of serum Na should be less than 0.5 mmol/L/h using the following formula for correction, which estimates the effect of 1 L of any infusate on serum Na:
In severe hypernatremia (serum Na > 170 mmol/L), it is recommended that the maximum Na concentration not be corrected to below 150 mmol/L in the first 48 to 72 hrs.64
The epidemiology of hypernatremia in children has changed recently from gastroenteritis with dehydration as the principal cause to one of a hospital-acquired problem in association with either excess salt administration or a free-water deficit. In a study by Moritz of children with a serum Na above 150 mmol/L, the problem was hospital acquired in 60%, and the mortality was 11%.65 In a similar series of adult patients, the ICU mortality rate for patients with plasma Na levels above 150 mmol/L was 30%.66
 Management of Acute Water and Sodium Deficits in Children
Management of Acute Water and Sodium Deficits in Children
Water and Electrolyte Deficits in Diabetic Ketoacidosis
Diabetic ketoacidosis (DKA) is characterized by losses of water and electrolytes due to hyperglycemia-induced osmotic diuresis. The high osmolality of the ECF results in shift of water from the ICF compartment. Studies performed in adult humans with type 1 diabetes where insulin therapy has been withheld have shown fluid deficits of 5 to 10 L together with up to 20% loss of total body sodium and potassium.67 At the time of presentation, patients are ECF contracted, and clinical estimates of the deficit are usually in the range of 7% to 10%, although shock with hemodynamic compromise is a rare event in DKA in children. The hyperglycemia in DKA results in a hyperosmolar state, but serum Na concentration is an unreliable measure of the degree of ECF contraction, owing to the dilutional effect of fluid shift from the ICF to the ECF compartment. The effective osmolality (2 [Na + K] + glucose, all in mmol/L) at the time of presentation is frequently in the range of 300 to 350 mOsm/L. An elevated hematocrit may be a useful marker of severe ECF contraction. Urea is not an effective osmole because it moves freely across the cell membrane and is therefore not included in the calculation. An estimate of true ECF deficit can be made by “correcting” the measured serum Na for the increase in ECF water using the formula developed by Katz68:
The ECF contraction is associated with a reduction in GFR which results in reduced glucose and ketone clearance from the blood and worsening DKA. Studies in humans have shown that IV fluid administration alone results in substantial falls in blood glucose before insulin has been given; this is due to the increase in GFR.69 Serum K is also frequently elevated at the time of presentation70 but falls rapidly as GFR increases and insulin re-primes the Na+/K+-ATPase cell membrane pump.71
Cerebral edema as a complication of diabetic ketoacidosis (CE-DKA) was first described by Dillon in 1936.72 Although originally reported in adults,73–76 it is much more common in children and accounts for the majority of morbidity and mortality associated with DKA in this age group.77 The reported occurrence rate in the pediatric literature varies between 0.2% and 1%.78–81 However, this is likely to be an underestimate, as it is based on retrospective reviews relying on the clinical diagnosis of increased intracranial pressure. The incidence is also reported to be higher in new-onset diabetes and in younger children.78,81,82 Series of brain imaging studies in children with DKA have shown decreased ventricular size either early (<12 hours) in the treatment course83 or even before therapy has commenced.84 The ultimate consequence of this, namely brainstem herniation, has been reported to be 5.8% (9/153) in one series of all children presenting with DKA.85 The total adverse outcome rate (death or permanent neurologic injury) in CE-DKA is as high as 40% to 50% in some series, with few intact survivors where brainstem herniation has occurred.78,86,87 For these reasons, children with severe DKA (pH < 7.2) should be admitted to the ICU for close monitoring of CNS status during the first 24 hours of correction of the fluid deficit. Symptoms such as diminished level of consciousness, headache, or vomiting are signs of impending cerebral edema.
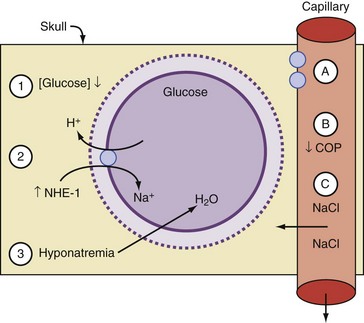
Many theories have been advanced to explain brain swelling in association with DKA, including overzealous rehydration with hypotonic IV fluids, rapid reduction of blood glucose with insulin, activation of the sodium/hydrogen ion (Na+/H+) transporter system, change in oncotic pressure, increased permeability of the blood-brain barrier, and changes in cerebral blood flow.78,81,85,86,88 Most of these have been developed from individual case reports or small case series. Although the precise cause is not fully understood, there is general agreement that the pathogenesis of CE-DKA involves an osmolar shift that results in fluid accumulation in the ICF compartment and cell swelling.
Although the cause of cerebral edema in DKA is a subject of much controversy,89 several case series have focused on fluid rehydration. The standard approach formerly was to give a bolus of between 10 and 30 mL/kg of fluid at the time of presentation, often with a bolus of insulin (0.1 units/kg). IV fluids were then administered depending on the clinical diagnosis of the degree of dehydration. This was done by calculating the fluid deficit and replacing this over 24 to 36 hours using a hypotonic fluid, generally 0.45% NaCl with added potassium. In the late 1980s and early 90s, a number of groups began to question the wisdom of this approach86,90,91 based on experiences with CE-DKA. They noted that in many cases of CE-DKA, the measured serum Na failed to rise during fluid resuscitation as expected, indicating a failure to protect against a rapid fall in the effective osmolality. As a result, they advocated a more conservative therapeutic approach, limiting the total fluid to under 4 L/m2/d and increasing the tonicity of IV fluids. Using this approach, Harris et al. reported a decrease in the incidence of symptomatic cerebral edema but not its elimination.90 In a second series by the same authors using the same approach, mannitol was administered for increasing obtundation in only 4/231 episodes, and there were no adverse outcomes in the total series.91 However, the practice of aggressive fluid resuscitation still persists. Roberts92 has recently reported a case series of 11 children who developed CE-DKA, most of whom received large amounts of IV fluid (>40 mL/kg in the first 4 hours). All received mannitol and, with one exception, recovered.
The issue of changes in serum osmolality as a risk factor has been identified in several series (Figure 113-2). A rapid reduction in effective osmolality is associated with either a fall in blood glucose or serum Na, or both, due to the rapid administration of IV fluid and possibly by bolus-dose insulin. Insulin administration is also known to activate the Na+/H+ ion exchanger, increasing the ICF Na concentration.88 Water follows the osmotic gradient back into the ICF compartment. Hale,93 in a retrospective series, found that CE-DKA developed in children when there was a progressive fall in serum Na and osmolality compared to patients without brain swelling, where effective osmolality did not change. In a large series that included age-matched controls, other identified risk factors for development of cerebral edema were a low PaCO2 and a high urea at the time of presentation.81 These are probably reflective of the severity of the acidosis and ECF contraction. The only treatment variable that was associated with CE-DKA in this series was the use of bicarbonate therapy.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree