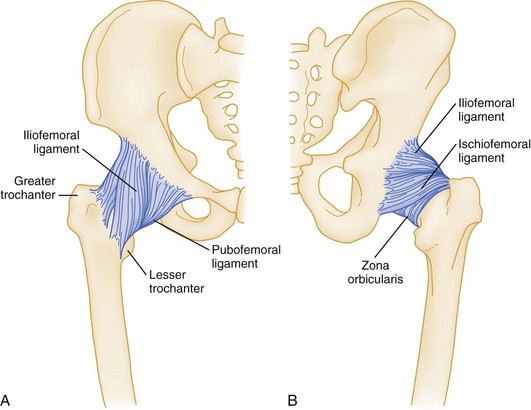
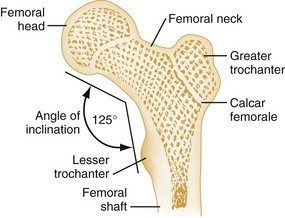
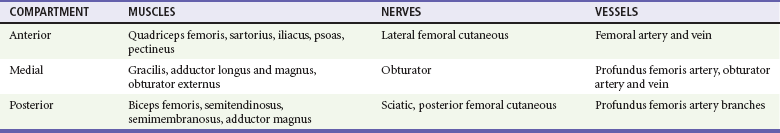
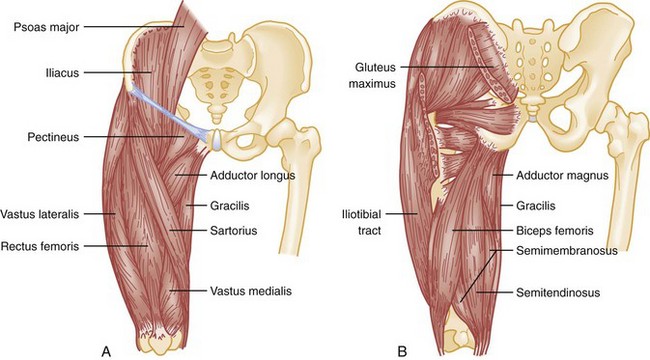
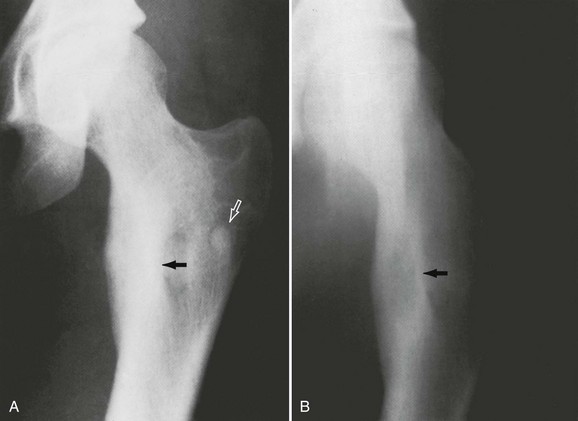
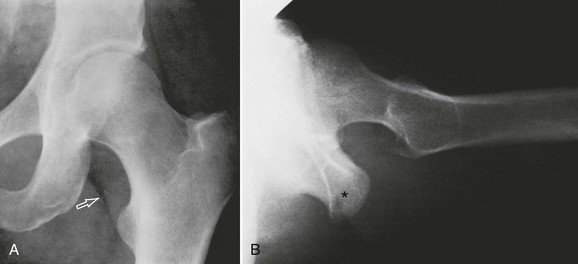
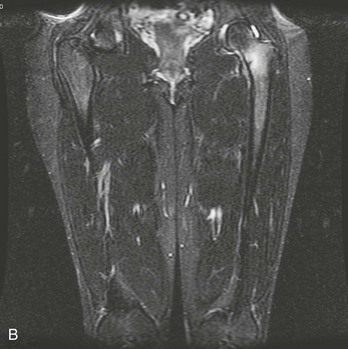
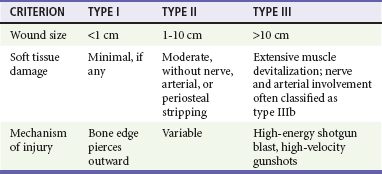
Chapter 56 Ancient Egyptian and Greek drawings depict persons with hip deformities ambulating with assistive crutches. The first available written description of a hip fracture was by the 16th-century French surgeon Ambroise Paré.1 In 1850, von Langenbeck was the first to attempt repair of a hip fracture with a nail for internal fixation. Later, Davis used ordinary wood screws in an attempt to aid the healing of femoral neck fractures.2 With the advent of radiography in the 19th century, the types of fractures and dislocations became easily identifiable, thus allowing discussion and investigation of management strategies, classification systems, and prognosis. Approximately 10 million adults in the United States have osteoporosis, and an additional 33.6 million have low bone density of the hip, both of which predispose to hip fracture.3 The annual incidence of hip fracture continues to grow as our population ages. During the late 1990s, approximately 250,000 patients a year sought treatment in emergency departments (EDs) after sustaining hip fractures.4 In 2005 alone, this number exceeded 290,600 patients.5 It is estimated that this number will surpass half a million patients a year by 2025.5 Although hip fractures represent only 14% of all fractures in adults, they account for 72% of medical costs related to fractures.5 Femoral neck fractures have a female to male ratio of 4 : 1 and typically occur in elderly patients with osteoporosis.6 There is an increasing incidence of intertrochanteric fractures with advancing age, and women are affected six times more often than men.3,7 Overall, more than three quarters of all hip fractures occur in postmenopausal women older than 50 years.3 The elderly are not the only population affected by hip and femur pathology. Perthes’ disease—avascular necrosis (AVN) of the femoral head—occurs from 2 to 14 years of age, with a peak age of onset of 5 years, and it is five times more common in boys than in girls.8 Slipped capital femoral epiphysis (SCFE) peaks at 13.5 years of age among boys and 12 years among girls, in association with the onset of puberty, and is nearly twice as common in boys.9 The femoral head is firmly seated in the acetabulum, which is reinforced by labral cartilage. The well-developed capsule, overlying ligaments, and proximal musculature of the lower extremity add strength to the joint (Fig. 56-1). The nearly spherical femoral head articulates with the acetabular cup in a variation of the ball-and-socket joint. The femur is the longest and strongest bone in the human body and is routinely subjected to substantial forces produced during powerful muscle contraction and weight transmission. In an anatomic position, the two femurs extend obliquely from the pelvis medially to the knee and bring the legs closer to the midline, where they can best support the body. Structurally, the femoral neck serves as an oblique strut between the pelvis (the horizontal beam) and the shaft of the femur (the vertical beam) (Fig. 56-2). The length, angle, and narrow circumference of the femoral neck permit substantial range of motion at the hip, but these same characteristics subject the neck to incredible shearing forces. A fracture results when these forces exceed the strength of the bone. As drawn on an anteroposterior (AP) radiograph, the intertrochanteric line, an oblique line connecting the greater and lesser trochanters, marks the junction of the femoral neck and its shaft. The musculature of the hip and thigh is the largest and most powerful in the human body. The muscles in this region of the body are located within three different compartments, each containing associated nerves and vessels (Table 56-1). The muscles also are grouped according to their primary action at the hip. Knowledge of the major muscle actions offers insight into the injury patterns and deformities commonly seen (Fig. 56-3). The arterial supply to the femoral head arises from two main sources (Fig. 56-4). The major source is the ascending cervical arteries as they branch off the extracapsular ring and run along the femoral neck beneath the synovium. Some blood is supplied to the femoral head from the second source, within the marrow spaces—the intraosseous cervical vessels. A third and minor source is the foveal artery, which lies within the ligamentum teres. As the external iliac artery passes beneath the inguinal ligament, it becomes the common femoral artery.10 At this point the artery is located midway between the anterior superior iliac spine (ASIS) and the symphysis pubis. Approximately 3 to 4 cm distal to the inguinal ligament, the common femoral artery branches to form the superficial and deep femoral arteries. The larger superficial femoral artery passes along the anteromedial aspect of the thigh and terminates at the junction of the middle third and lower third of the thigh. Here, the superficial femoral artery passes through the adductor hiatus and becomes the popliteal artery. The deep femoral artery runs posterolaterally to the superficial femoral artery, supplies the hamstrings, and terminates in the distal third of the thigh as small branches piercing the belly of the adductor magnus. These perforating branches constitute an additional site of potential injury. The abundant muscle coverage and blood supply of the thigh aid in healing fractures of the femoral shaft. In the proximal two thirds of the thigh, the common and superficial femoral veins lie adjacent to the common and superficial femoral arteries. At the inguinal ligament, the common femoral vein is posterior and medial to the common femoral artery and moves to the lateral position as it passes distally. The deep femoral vein and the greater saphenous vein are the two main tributaries to the common and superficial femoral veins. The deep femoral vein and artery run in parallel as the vein joins the superficial femoral vein just distal to the inguinal ligament. The greater saphenous vein arises in the dorsum of the foot and ascends anterior to the medial malleolus. This vein is relatively superficial as it passes up the medial aspect of the leg to join the common femoral vein distal to the inguinal ligament.10 The femoral and sciatic nerves are the major nerves within the thigh. The femoral nerve is the largest branch of the lumbar plexus; it passes under the inguinal ligament lateral to the femoral artery and divides into anterior and posterior branches soon after entering the thigh. The sensory divisions of the anterior branch, the intermediate and medial cutaneous nerves, supply sensation to the anteromedial aspect of the thigh. The motor division of the anterior branch innervates the pectineus and sartorius muscles. The posterior femoral branch gives off the saphenous nerve, which supplies sensation to the skin along the medial aspect of the lower part of the leg. The posterior branch also supplies motor function to the muscles of the quadriceps femoris group.10 The sciatic nerve is the largest peripheral nerve in the body. It arises from the sacral plexus. The sciatic nerve exits the pelvis through the greater sciatic foramen and travels through the posterior thigh; it extends from the inferior border of the piriformis to the distal third of the thigh. The sciatic nerve gives off articular branches that supply the hip joint. In the thigh, muscular branches innervate the adductor magnus and hamstring muscles. Just proximal to the popliteal fossa, the sciatic nerve divides to form the tibial and common peroneal nerves.10 Osteoporosis is the leading cause of hip fracture. Osteoporosis currently affects more than 10 million people in the United States and is projected to affect approximately 14 million adults older than 50 years by the year 2020. The number of hip fractures attributable to osteoporosis is expected to be 6.3 million by the year 2050, although the incidence in women has been decreasing in recent years, probably because of an increased awareness and more aggressive treatment of osteoporosis.3,11 Hip fractures can have a devastating impact. One in five patients dies during the first year after a hip fracture, mostly from causes other than the fracture itself; one third require nursing home placement after hospital discharge; and less than one third regain their prefracture level of physical function.12 The economic impact of these fractures is enormous. The pathophysiology of osteoporosis is not completely understood, but strong associations with hormonal changes related to aging, genetic predisposition, vitamin D deficiency, lack of physical activity, and smoking have been recognized.13 Severe osteoporosis and hip fractures are most common in elderly white women; however, a decrease in bone density after age 30 is seen across all demographic groups. Radiography of the head of the femur can quantify the degree of osteoporosis, even in the nonfractured hip. The trabeculae of the femoral head and neck strengthen the bone and support the large mechanical forces produced across the hip joint. As osteoporosis begins and then progresses, these trabeculae disappear. This loss of trabeculae weakens the bone and increases the risk of fracture. As the population ages, a greater percentage of the population will develop chronic pain from degenerative osteoarthritis of the hip. Overall, osteoarthritis ranks fifth in health impact (measured in years lost to disability) in high-income countries and ninth in low- and middle-income countries.14 Disability often results from persistent pain and limited physical mobility. The progression of osteoarthritis can be demonstrated with serial radiographs of the affected hip (Fig. 56-5); however, radiographic findings do not necessarily correlate with symptoms.15 When a patient has an increasingly painful hip, buttock, thigh, or knee and no history of recent trauma, AVN of the femoral head should be considered. AVN has been referred to as aseptic necrosis, ischemic necrosis, and osteonecrosis. It is the result of ischemic bone death of the femoral head after compromise of its blood supply (Fig. 56-6). AVN is bilateral in 40 to 80% of patients. It is common in relatively young patients, the mean age at diagnosis being 38 years.16 Although a specific causative disorder is not identified in 20% of the cases, known atraumatic causes include chronic corticosteroid therapy, chronic alcoholism, hemoglobinopathy (e.g., sickle cell anemia), dysbarism, and chronic pancreatitis.16,17 AVN also is an emerging complication associated with human immunodeficiency virus (HIV) infection. It is unclear whether the virus itself or the treatments are the pathogenic agents.17 Traumatic AVN is a subacute manifestation after hip dislocation or femoral neck fracture. It is a direct result of disruption of the blood supply to the femoral head. It is more common in males and African Americans. The incidence of AVN as a subacute complication is clearly related to both the initial degree of trauma and the amount of time the femoral head remains out of joint. Reduction of the hip within 6 hours after dislocation significantly decreases the incidence of AVN.18 Multiple studies have shown that there is relationship between the length of time the hip is dislocated and the rates of AVN, with as few as 4.8% of patients developing AVN with reduction within 6 hours, and as many as 58.8% developing AVN with reduction after more than 12 hours. For this reason, hip dislocation should be considered an orthopedic emergency. The emergency physician should perform reduction of the hip if there is any delay in orthopedic consultation. Even with optimal treatment, femoral neck fractures are complicated by AVN in 11 to 19% of cases. For all practical purposes, femoral neck fractures are effectively intra-articular fractures. Acutely, bleeding from the fracture site may cause high intracapsular pressure and a tamponade effect on the femoral head, thereby further impairing the blood supply to it.19 In addition, if the bone fragments are not impacted, synovial fluid will lyse the blood clot. Such lysis prevents the development of capillary buds and the scaffolding needed for osseous repair. These factors all contribute to make AVN of the femoral head a common complication. Conversely, intertrochanteric and subtrochanteric fractures are located in an area of rich blood supply provided by an extracapsular arterial supply. AVN rarely complicates these fractures. Myositis ossificans (heterotrophic ossification) is pathologic bone formation at a site where bone is not normally found. Traumatic myositis ossificans results most commonly from a direct blow to muscle. The thigh and hip muscles are often involved. The incidence of myositis has been reported as up to 17% of patients undergoing medical evaluation of thigh contusions, and the condition is thought to be related to the severity of the injury.20–22 The incidence of myositis ossificans after hip surgery is approximately 2%, but these lesions are clinically significant in only 10 to 20% of cases.21 Increased susceptibility to myositis ossificans has been described in persons with hemophilia or other bleeding disorders in conjunction with soft tissue injury.21 Radiographically, myositis ossificans appears as irregularly shaped masses of heterogeneous bone in the soft tissues around the joint or along fascial planes (Fig. 56-7). It may be seen as early as 10 to 21 days after injury, but radiographic evidence typically lags behind onset of symptoms by weeks.20 Its appearance may simulate primary bone neoplasm, especially when the periosteum is involved. Osteosarcoma and periosteal osteogenic sarcoma should be considered in the differential diagnosis. Computed tomography (CT) scan can sometimes be helpful in distinguishing between neoplasm and myositis ossificans, as the lesions of myositis ossificans begin to calcify at the periphery and progress toward the center, and those of osteosarcoma begin to calcify at the center first. Orthopedic follow-up should be arranged for these patients. Initial treatment of contusions is aimed at preventing myositis ossificans by use of the RICE principle of rest, ice, compression, and elevation. Immobilization of the extremity may prevent retraction of ruptured muscle and increasing size of hematoma formation but should be limited to less than 48 hours. Once a stable scar has formed, range of motion within limits of pain should be initiated. If myositis ossificans has already formed, the mainstay of treatment is supportive with rest, slow return to normal activity, and physical therapy. Although indomethacin is commonly used to prevent heterotopic ossification after surgery, it has not been validated for the prevention as well as the treatment of myositis ossificans.20,21 Its use based on the principle of inhibition of bone formation does not seem to be contraindicated.20 Operative removal of a mature lesion may be indicated if the lesion is near a joint or is causing permanent impairment or pain. Calcification surrounding tendons and bursae or occurring in the joint capsule is referred to as calcific bursitis or calcifying peritendinitis. The cause of these lesions is unknown. No relationship has been documented between the radiographic findings and acute symptoms. Calcific bursitis of the hip is uncommon, but when it does occur, it most frequently affects the trochanteric bursa (Fig. 56-8). Other possible affected areas include gluteal muscles and the hip flexors and adductors. The bursal calcification is seen on radiographs as an amorphous, poorly marginated line that is clearly separate from the cortex of the femur. Treatment should focus on stretching and strengthening of the hip. The most common neoplastic disease of bone is metastatic, generally from breast, kidney, lung, thyroid, or prostate tumors. Primary bone lesions also occur, with the most common being osteoid osteoma (Fig. 56-9). Bone lesions may be osteoblastic or osteolytic. Patients may come to the ED with significant bone pain or a large bothersome mass, such as a solitary osteochondroma (Fig. 56-10). Neoplasms place the patient at higher risk for pathologic fracture, especially if the lesions are large or lytic or have eroded the cortex. Age and gender are predisposing factors for certain injuries. A detailed description of any antecedent trauma or other precipitating events is often helpful. With trauma, details of the mechanism of injury may aid in predicting injury patterns. With stress fractures, an alteration in physical activity or exercise routine provides a clue to the diagnosis. Systemic illnesses or known metabolic disorders should be noted. Previous cancer, irradiation, and chemotherapy are clues to pathologic fractures. Any past steroid use, including inhaled steroids, is important to identify because it predisposes patients to AVN of the femoral head. A linear relationship has been recognized between the cumulative steroid dose and the incidence and severity of osteoporosis and hip fracture.23 Ascertainment of the location of the patient’s pain is paramount; true hip joint pain is often groin pain. However, pediatric patients with hip pathology often have knee pain as the sole presenting complaint. A review of systems should include information that may help in ascertaining hip or femur pathology versus another cause. Atypical pain may be the result of nephrolithiasis, pelvic inflammation, infection or tumor, inguinal and femoral hernia, or adenopathy from genital or cutaneous infection. A history of low back pain may suggest radiculopathy as the cause of the patient’s pain. A differential diagnosis of hip pain without obvious fracture on radiographs is listed in Box 56-1. The history should also focus on comorbid conditions and injuries. Elderly patients with a hip fracture sustained in a fall at home may be unable to summon help for hours to days. They often have severe dehydration, electrolyte abnormalities, rhabdomyolysis, and renal insufficiency and require a thorough evaluation of these metabolic parameters before surgery is considered.24 In addition, the reason for the fall should be determined, as it may reveal other comorbid conditions (e.g., syncope, cardiac dysrhythmias, polypharmacy, alcoholism). Sedative or antihypertensive medications predispose elderly patients to falling and should be prescribed carefully. In a fall, elderly patients may have sustained additional injuries; most commonly, these injuries involve fracture of a vertebral body or wrist. Cervical spine and intracranial injuries also are considered. Young patients with a hip fracture resulting from high-energy mechanisms have concomitant injuries in 40 to 75% of cases.18 Systematic examination of the injured extremity will reveal any focal tenderness or warmth that may indicate injury or infection. Active and passive range of motion, and muscle strength, though offering important information, are frequently limited by pain. Detailed neurovascular assessment is vital. Femoral nerve and arterial injury often occur with subtrochanteric and femoral shaft fractures or anterior hip dislocation. The sciatic nerve can be injured with a hip fracture or posterior hip dislocation. Neurologic examination includes evaluation of light touch and pinprick sensation. Femoral, popliteal, dorsalis pedis, and posterior tibial pulses are assessed. Comparative blood pressures obtained by Doppler examination in the injured and uninjured extremities (arterial pressure index) may be useful in diagnosing occult femoral arterial injuries. If the systolic pressure in the affected extremity is 90% or less (ratio less than 0.9) than that in the unaffected extremity, additional diagnostic studies should be undertaken. Additional diagnostic studies include Doppler flow ultrasound imaging, CT angiography, or angiography alone. The ankle-brachial index (ABI) also can be similarly determined by comparing the systolic pressures of the affected extremity and of the ipsilateral arm. An index less than 0.9 necessitates further diagnostic studies.25,26 Radiographic Anatomy and Evaluation Normal radiographic and skeletal anatomy is familiar to emergency physicians (Fig. 56-11). True AP and lateral radiographs of the femur are usually adequate for the evaluation of potential fractures. The femur should be in as much internal rotation as possible. Fracture lines may be very subtle, particularly with femoral neck fractures. Experts have found three methods useful for identifying inconspicuous fractures. The use of Shenton’s line is described in a subsequent section on hip dislocations. (A second method is illustrated in Fig. 56-15.) In searching for a fracture of the femoral neck, both the medial and lateral cortical margins of the femoral head and neck should be carefully examined for the normal S and reverse S curves seen on radiographs of nonfractured hips. The convex outline of a normal femoral head smoothly joins the concave outline of the femoral neck when in anatomic position. This produces an S curve and a reverse S curve, regardless of the orientation of the radiographic projection. A fracture produces a tangential or sharp angle, indicative of disruption of the normal anatomic relationship. A third method, useful in the evaluation of seemingly unremarkable hip radiographs, is to trace the trabecular lines as they pass from the femoral shaft to the femoral head. These lines will be disrupted as they pass through the fracture site, and such disruption often provides the only, albeit subtle, clue. If a fracture is found, radiographs of the knee should be obtained as well. It is a basic orthopedic principle to image the joint above and below any fracture.25 One common inaccuracy in hip radiography merits clarification: The soft tissue linear radiolucencies superolateral and inferomedial to the femoral head and neck do not represent the hip capsule, as is commonly believed. Instead, they represent the fat within the fascial plane covering the gluteus minimus superiorly and the tendon of the iliopsoas muscle inferiorly.27 Comparison of these lines on the symptomatic side with those on the unaffected side should not be used to determine whether an effusion of the hip is present. If radiographs do not show a fracture, or suggestion of injury, ambulation may be attempted. Inability to ambulate or difficulty in ambulation heightens the suspicion of occult fracture. Approximately 2 to 10% of all hip fractures are radiographically “occult” on plain films.28 Failure to detect these injuries results in increased mortality, risk of subsequent displacement of the fracture, and a higher incidence of AVN.29,30 When a painful hip prevents ambulation and plain radiographs do not reveal a fracture, magnetic resonance imaging (MRI) should be performed.28,29 In addition, elderly patients with unexplained chronic hip pain for more than 3 weeks may harbor an occult fracture even if they continue to ambulate. T1-weighted MRI will reveal a fracture that was imperceptible at the time of injury with 100% accuracy and has been found to be cost-effective when compared with other strategies.29 A small study comparing CT scans with MRI in the diagnosis of occult hip fractures revealed a 66% misdiagnosis rate for CT scans.29 MRI remains the “gold standard” modality for diagnosing occult hip fractures and helps determine the treatment of these fractures (Fig. 56-12). Patients with traumatic fracture of the hip or femur should have blood typed and crossmatched for at least 2 units of blood. The potential for significant blood loss and the multiple common associated injuries constitute important justification for this recommendation. Hemodynamic instability may result from dehydration and blood loss of up to 3 units into the fracture site. Currently, treatment of these fractures is hemiarthroplasty or open reduction and internal fixation for femoral neck fractures. Internal fixation with a sliding compression screw generally is used to treat intertrochanteric fractures. The goal is to promote immediate postoperative mobilization. It has become widely accepted that the risks of surgery in elderly patients are minimal when compared with the risks of prolonged bed rest, deep vein thrombosis, pulmonary embolism, pneumonia, and urosepsis from an indwelling Foley catheter. If possible, the repair is conducted with use of spinal anesthesia to decrease the operative risk. Operative repair should be performed after the patient is resuscitated and is in optimal preoperative condition. Care of an elderly patient with a hip fracture requires a multidisciplinary approach and often involves coordination of the efforts of the emergency physician, orthopedist, internist, neurologist, and cardiologist to stabilize the patient before surgery. Comprehensive hip fracture programs for the elderly that include comanagement by geriatricians and orthopedic surgeons have been shown to improve short-term outcomes and may even lower mortality, highlighting the importance of medical management of these complex patients.31,32 Contraindications to the use of traction splints include pelvic fractures, patellar fractures, ligamentous knee injuries, and tibia or fibula fractures. Traction in the prehospital setting should not be applied to any open fracture that has exposed bone. Such reduction pulls grossly contaminated bone fragments back into the wound before adequate débridement can be undertaken in the operating room. A study that evaluated patients with multisystem trauma in whom traction splints were placed in the field for femur fractures showed that up to 38% of the cases had contraindications to the splints that were placed.33 With or without traction, the injured extremity should be immobilized when the patient is moved, to prevent further damage from mobile bone fragments. This can be done with simple splinting in the prehospital setting. In the ED, maintaining the leg in slight flexion at the hip reduces intracapsular pressure, whereas extension of the leg increases pressure and potential for ischemic necrosis of the femoral head. Therefore traction for proximal femur fractures may be discontinued once the patient has arrived in the ED. The leg may be supported in a position of comfort with a pillow placed under the thigh. The theoretic advantages for continuation of traction in the ED are pain control and fracture reduction, making operations easier to perform. This is likely true in femoral shaft fractures; however, a Cochrane systematic review looking at preoperative traction for fractures of the proximal femur in adults found no evidence to support these proposed advantages.34 By definition, an open fracture is any fracture in which a break in the integrity of the skin and soft tissue allows communication with the fracture and its hematoma. Any nearby wound or break in the skin must be considered to communicate with the fracture. Open fractures are divided into three categories (Table 56-2). A bone piercing from the inside outward often causes only a small wound. The contaminated bone tip may then slip deceptively back into the soft tissue; therefore any break in the integrity of the skin makes the fracture an open one. Open wounds should be irrigated and then covered with sterile saline-moistened gauze. Table 56-2 Classification of Open Fractures From Hoff WS, Bonadies JA, Cachecho R, Dorlac W: East Practice Management Guidelines Work Group: update to practice management guidelines for prophylactic antibiotic use in open fractures. J Trauma 70:751-754, 2011. For all type I open fractures, a first-generation cephalosporin should be administered intravenously. Types II and III may require additional gram-negative coverage because of the amount of devitalized tissue and increased gram-negative skin flora found in the groin.35 This additional coverage could be provided by an aminoglycoside such as gentamicin or tobramycin. The use of perioperative first-generation cephalosporins has been shown to reduce postoperative infection even in closed fractures in patients who are to undergo surgery.35 Because of the thigh’s larger volume, compartment syndrome within the thigh is far less common than in the lower part of the leg. A large amount of bleeding into the compartment is required before the pressure rises above capillary perfusion pressure. When compartment syndrome does occur in the thigh, only 50% of the cases are associated with a femur fracture.36 It is difficult to clinically differentiate the expected swelling after an injury from early compartment syndrome. Clinical examination and the use of direct compartment pressure measurements can detect the development of compartment syndrome at an early stage. It is well known that control of pain in EDs is often inadequate.37 In the case of femoral fractures, narcotic analgesia is often indicated in combination with other pain-relief strategies including immobilization of the injured extremity, placement of the injured extremity in a position of comfort, and the consideration of local analgesia in the form of nerve blocks. Femoral nerve blocks have been used to treat femoral shaft fractures for more than 50 years. Despite proven effectiveness and a low complication rate, this technique has not been widely embraced by emergency physicians or surgeons.38 The femoral nerve block is an excellent option as an adjunct or alternative to systemic analgesics in patients at risk for hypotension. It has been shown to significantly decrease time to lowest pain score as compared with intravenous narcotics, and patients have been found to require significantly lower doses of narcotics in conjunction with femoral nerve blocks.38,39 The block can be performed with the assistance of a peripheral nerve stimulator to localize the nerve, or bedside ultrasound to directly visualize the nerve before anesthetic injection.40 Femoral nerve blocks have been shown to be effective when performed by newly trained emergency physicians without the assistance of peripheral nerve stimulators or ultrasound.39 If a long-acting anesthetic such as bupivacaine is used, the expected onset of analgesia is within 30 minutes, and its duration is 6 to 8 hours.41 Sir John Charnley first described the modern form of total hip arthroplasty (THA) in 1961. Despite many changes in both the design and materials used, Charnley’s essential design has been established as the standard.42 The number of THA procedures performed annually in the United States rose from 65,000 in 1982 to more than 230,000 in 2007.43 The most common indication for THA is joint failure resulting from severe osteoarthritis. Other indications include rheumatoid arthritis, certain types of hip fracture, AVN, and certain tumors. Arthritis associated with Paget’s disease, trauma, ankylosing spondylitis, and juvenile rheumatoid arthritis are also relative indications for THA or partial hip arthroplasty. THA provides an immediate, substantial reduction of pain and improvement in functional ability and overall quality of life. A 10-year follow-up study of patient outcomes, including gait, perception of pain, physical mobility, sleep patterns, and energy scores, showed positive results in more than 90% of cases.44 Despite the tremendous success of THA, numerous complications have been reported. Aseptic loosening of the prosthesis is the most common. Other complications include component wear, infection, adjacent femoral fractures, deep vein thrombosis, and postoperative dislocation of the femoral component. In general, flexion past 90 degrees, adduction, and internal rotation place the hip at risk for dislocation. This combination can occur when patients bend at the waist (e.g., to sit on a normal low toilet or to get out of a chair) or cross the legs45 (Fig. 56-13). Fractures of the Hip and Femur The pain of avulsion injuries of the hip may manifest as referred pain to the thigh; these fractures are most common in adolescents and young adult athletes. The incidence of avulsion fractures is increasing as a result of the growth of competitive sports participation, especially in teenage athletes.46,47 The muscular origin of this type of injury commonly involves the pelvic apophyses, which may not fully ossify until age 25. Avulsion at the site of the growth plate is the result of sudden maximal muscular exertion. It may occur with rapid acceleration or sudden changes in speed or direction. The athlete classically experiences a sudden piercing pain at the site of injury, along with a “snapping” or “popping,” and frequently falls to the ground because of the intensity of this pain. As depicted in Figure 56-14, avulsion at the ASIS involves the separation of a thin piece of bone as the sartorius muscle suddenly contracts (see Fig. 56-14A). The anterior inferior iliac spine (AIIS) is avulsed by the rectus femoris, and the hamstring group may pull off the ischial tuberosity (see Fig. 56-14B). Avulsion fractures of the ASIS and AIIS are managed nonoperatively with conservative treatment. Treatment of avulsion fractures of the ischial tuberosity is more controversial. Most experts recommend conservative treatment for avulsion injuries with less than 2 cm of displacement. Fractures with more than 2 cm of displacement may benefit from operative fixation to prevent nonunion, as well as union with exuberant callus formation.47,48 Classification Systems.: Fractures of the proximal end of the femur have been classified on the basis of their relationship to the hip capsule (e.g., intracapsular and extracapsular), anatomic location (neck, trochanteric, intertrochanteric, subtrochanteric, and shaft fractures), and degree of displacement. A working knowledge of the classification system will allow the emergency physician to communicate with the consulting orthopedist regarding the fracture’s pattern and stability and treatment options.
Femur and Hip
Perspective
Epidemiology
Principles of Disease
Skeletal Anatomy
Musculature
Vascular Anatomy
Venous System
Nerves
Pathophysiology
Osteoporosis of the Femur
Osteoarthritis of the Hip
Avascular Necrosis
Myositis Ossificans
Calcific Bursitis and Calcifying Peritendinitis
Neoplastic Disease in the Hip
Clinical Features
Physical Examination
Diagnostic Strategies
Occult Hip Fracture
Management
Traction and Immobilization
Open Fracture Care
Compartment Syndrome
Pain Management
Femoral Nerve Block
Hip Arthroplasty
Outcomes and Complications
Specific Injury Patterns
Avulsion Fractures
Proximal Femoral Fractures
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Femur and Hip
Only gold members can continue reading. Log In or Register to continue