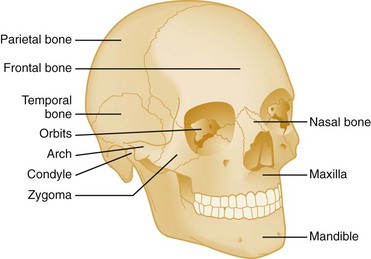
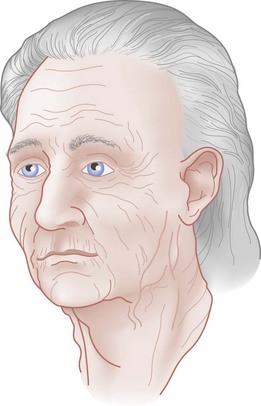
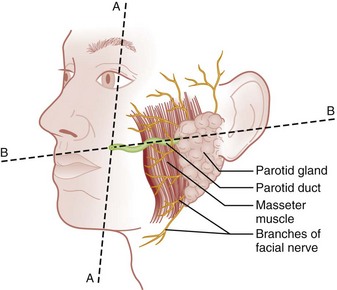
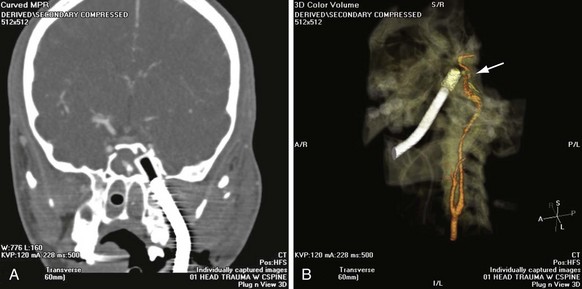
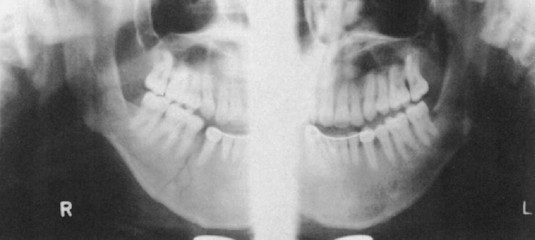
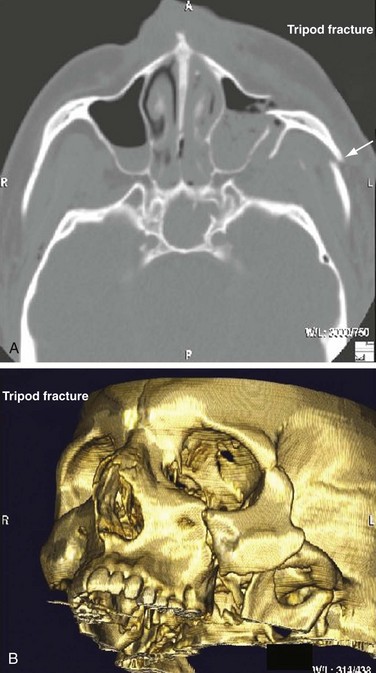
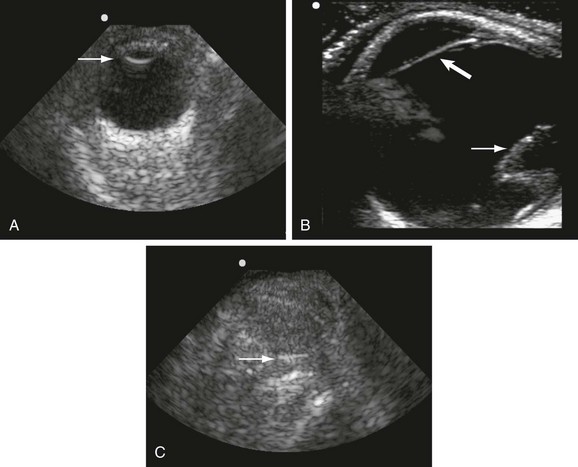
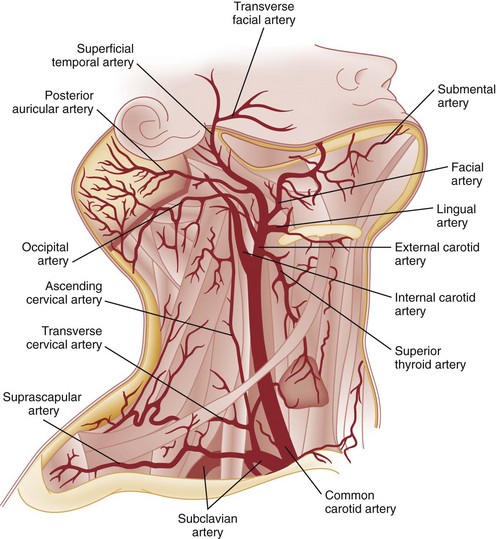
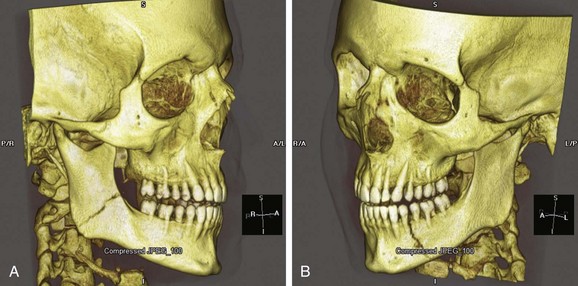
Chapter 42 This chapter discusses the epidemiology, diagnosis, and treatment of injuries to the skin, soft tissue, and bones of the face. A complex structure vital to the function of the person, the face comprises airway openings, entry to the gastrointestinal tract, and special sensory organs, including eyes, ears, and nose. Facial functioning is essential for eating, speaking, and effective nonverbal communication. The appearance and attractiveness of the face have significant implications for social interactions,1,2 sexual attraction,3 and self-esteem.4 In one study, patients who had sustained facial trauma experienced long-term sequelae including unemployment, incarceration, marital difficulties, and negative body image.3a Apart from immediate threat to the patient’s airway and special sense organs, injuries to the face can have serious implications for the patient’s mental health5,6 and future functioning. Post-traumatic patients with facial injuries often describe physical, financial, social, and psychological loss.7 In one study of predominantly unemployed young African American and Hispanic men, 25% had symptoms of post-traumatic stress disorder 1 month after having been treated emergently for a midface fracture.5,8,9 Some institutions are now including screening evaluations regarding supportive interventions as well as initiating support groups and online resources for facial trauma patients.7 Four main specialties—ophthalmology, plastic surgery, otolaryngology, and oral and maxillofacial surgery—participate in the care of facial injuries. In teaching hospitals, the specialties of plastic surgery, otolaryngology, and oral and maxillofacial surgery participate in approximately equal proportions.10 In level 1 trauma centers, plastic surgeons and oral and maxillofacial surgeons predominate.11 Early consultation with the appropriate specialist can expedite the care of facial injuries. In 2008 there were more than 40 million injury-related visits to U.S. emergency departments (EDs).12 Facial injuries accounted for a significant proportion of these visits and resulted from either intentional violence (assaults and attempted suicide) or unintentional trauma (falls, sports injuries, and motor vehicle crashes [MVCs]). The type of injury mechanism can be a good predictor of the extent of facial trauma sustained; for example, MVCs were related to multiple facial fractures, whereas assaults more often involved isolated mandibular fractures.13 Although MVCs used to be the most common cause of facial injuries, windshield improvements, increased use of safety belts, and the prevalence of air bags in vehicles are changing the epidemiology of facial trauma. Dual front-impact air bags have been required in all new vehicles since 1999, and safety belts are required for all passengers in the front row in 49 states (all except New Hampshire).14 Seat belts and air bags significantly reduce the incidence and severity of facial injury in adults.15–21 Because they effectively prevent ejection, safety belts specifically avert the extensive scalp and facial degloving injuries associated with being ejected through the windshield. Alcohol use by vehicle occupants decreases safety belt use and independently increases the risk of facial injury in MVCs.22 It also increases the risk of interpersonal violence. In one series, alcohol played a role in 49% of all maxillofacial fractures in patients requiring subspecialty care. Of the fractures related to alcohol use, 78% were a result of interpersonal violence and 13% of MVCs.23,24 Interpersonal violence is increasingly cited as the cause of facial injury, particularly in inner-city populations.25–28 Falls, dog bites, some athletic activities, and flying debris are other common causes of facial injuries. Because of the lack of external protection, facial injuries are common among riders of other motorized vehicles, particularly those who are not wearing helmets with face guards, including all-terrain vehicles (ATVs) and motorcycles. In one series in Alabama, 32% of injured ATV riders had a facial injury, and the presence of a facial injury was associated with increased overall injury severity.29 Among the youngest riders, facial injuries predominate: 31.1% of 0- to 5-year-olds injured while riding an ATV required emergency treatment for a facial injury in 2001 through 2003, although multiple safety and medical groups recommend no ATV use by people younger than age 16 years.30 In motorcyclists, there is a significant association between facial injury and brain injury.31 Helmets reduce the risk of brain injury but may not protect against facial trauma unless they include a face guard.32 Unfortunately, a separate group of the injured must now be considered: combat veterans. A review of injuries sustained in battle by combatants in Operation Iraqi Freedom and Operation Enduring Freedom and treated by U.S. military medical facilities for at least 72 hours revealed that 19% of patients sustained injuries to the face, ears, or eyes. Of all these injuries, 19% were caused by gunshots, 79% by explosive devices, and 2% by MVCs.33 In children younger than age 17 years, sports injuries account for 21% of facial and 29% of nasal fractures requiring specialist evaluation.34,35 Baseball and football helmets with face guards are successful at preventing childhood facial injuries, and their use should be encouraged by emergency physicians.36 Children younger than age 6 years seem to be at significant risk for severe facial injuries from bites from the family dog.37 Interactions between pet dogs and young children require careful supervision. Facial injuries are a common acute presentation for victims of domestic violence. In one series, 81% of domestic violence victims had maxillofacial injuries on presentation, 30% of them with facial fractures. The location of the injury was consistent with the predominance of fisted assaults; left-sided injuries predominated.38,39 Women visiting the ED with facial injuries should be interviewed privately to allow an opportunity for disclosure and intervention for domestic violence. Pediatric facial injury accounts for less than 10% of all facial trauma, and the face is the most common area of trauma in children suspected of being victims of abuse.40 However, the epidemiology of facial trauma among children reflects their physical development and behavioral patterns: toddlers learning to walk have a “falling zone” of trauma to the perioral region, nose, and forehead. Younger children are significantly more likely to have minor soft tissue injuries and to have been the recipient of a dog bite. Severe facial injuries in all pediatric age groups are more likely to be the result of an MVC or assault.41 Care should be taken by the emergency physician to correlate the child’s age and behavioral ability with the history of the injury and the physical findings. In particular, injuries to the lips or frenulum in a nonambulatory infant suggest “bottle jamming,” and bruises to the cheeks or neck are less common in falls. Although dental fractures in young children are relatively common, facial fractures before age 5 years are rare. If there is any question, the appropriate local authorities are contacted. Even in high-energy MVCs, appropriate use of child safety restraints protects against many facial injuries. The law in all 50 states requires the use of such restraints for children younger than age 4 years, and currently 48 states require booster seats until at least age 7 years and many beyond that age.14 Children younger than age 15 years involved in frontal crashes or exposed to a deploying frontal impact air bag had a higher incidence of minor facial and chest injuries and severe upper extremity injuries, mostly related to being struck by the bag.43 As part of preventing facial trauma, parents should be encouraged to ensure that children younger than 12 years ride in the rear seat of the vehicle and that all are properly restrained. The posterior portions of the face form the anterior wall of the calvaria, placing the face and its features in an intimate relationship with the structures of the central nervous system. The anterior facial skeleton is composed of the frontal bone, nasal bones, zygomata, maxillary bones, and mandible (Fig. 42-1). The sphenoid, ethmoid, lacrimal, vomer, and temporal bones lie deep within the facial structure, providing support and important sites for muscular attachments, including the muscles of mastication, speech, and deglutition. This musculature is innervated by cranial nerves IX and X. The structure of the globe and surrounding ocular musculature is discussed in detail in Chapter 71. The bony orbit is composed superiorly of the frontal bone. The zygoma forms the lateral wall and lateral floor of the orbit. The medial floor and anteromedial wall are formed by the maxilla. The lacrimal and ethmoid bones complete the medial wall, where the orbit is at its most delicate. The medial wall of the orbit forms the lateral walls of the intranasal space. The skin of the face is among the thinnest of the body, draping over the underlying musculature. Facial skin falls visibly into predictable creases with age, following Langer’s lines (Fig. 42-2). At the mouth, nares, and palpebral fissures, the skin is contiguous with the mucosa lining these structures. The skin of the lips is particularly thin and lined with vascular papillae, which give the lips their vermilion hue. Lips are particularly important as part of communication; understanding their movement can allow language without sound (lip reading). The face is a highly vascular structure; this can have grave implications for the treatment of facial injuries. With the exception of the ophthalmic artery, the superficial blood supply comes from the external carotid artery via the facial, superficial temporal, and maxillary arteries (Fig. 42-3). Soft tissue injuries and fractures that involve these vessels can lead to significant hematomas or exsanguinations. Because the face has extensive anastomotic connections across the midline and between arterial territories, however, ligation of major branches causes minimal ischemia. Figure 42-3 Vessels of the face. (Redrawn from Gray H: Gray’s Anatomy, Philadelphia, Lea & Febiger, 1918.) The salivary system consists of the parotid, sublingual, and submandibular glands. The parotid is the largest of these glands, lying just anterior to the ear and wrapping around the mandible. The parotid is superficial to the masseter muscle and drains via Stensen’s duct, a 5-cm tube that curves around the anterior edge of the masseter to enter the mouth opposite the second upper molar. In normal subjects, this duct is large enough to be palpated with the masseter clenched (Fig. 42-4). The sublingual glands lie entirely within the floor of the mouth and drain into the mouth via ductules. They surround the ducts draining the submandibular glands (Wharton’s ducts). The body of the submandibular gland is folded around the mylohyoid muscle so that a portion lies within the floor of the mouth and a portion lies external to it. The submandibular (Wharton’s) ducts run from the external portion of the gland to empty into the mouth on either side of the frenulum of the tongue. Traditional teaching has been that the face protects the brain from injury and that patients with facial trauma are less likely to have a significant brain injury. This does not appear to be correct. Instead, recent work suggests a significant increase in risk for brain injury among blunt trauma patients with facial fractures.44 The association between cervical injury and facial injury is unclear. The traditional teaching has been that the presence of a facial injury should increase the suspicion of an injury to the cervical spine. However, most of the studies supporting this idea are assessments of the incidence of cervical spine injury in patients with facial injury.45 When more sophisticated methods are used to assess any association between the two while correcting for the mechanism of injury, patients with facial injury appear to be less likely to have a significant cord injury, and there is no relationship with bony spinal injury.46 Thus in a particular patient, cervical and brain injuries should be considered based on the mechanism of injury and presentation of the patient without allowing the presence or absence of a facial injury to change the level of suspicion. Penetrating trauma to the face from gunshots, stab wounds, blast debris, or impalement is often obvious and dramatic (Fig. 42-5). The astute emergency physician should search avidly for associated intracranial, spinal, or vascular injuries, which are common in these cases.47 Facial penetration from pellets (BBs) or small blast debris or shrapnel may be less obvious, and the emergency physician should be alert to the possibility based on the history and should carefully search for small skin lesions.48 Recreational hobbies such as paintball and new law enforcement weapons such as the “flash ball,” which can have substantial kinetic energy, have caused significant facial and upper body trauma.48a–48b The integrity of the mouth and nasal complex may be evaluated by listening to the patient’s speech. A muffled or overly nasal voice may indicate occlusion of the nose or nasopharynx, whereas dysarthria may indicate a mandibular fracture, tongue injury, or neurologic problem. Oral injury may result in progressive airway compromise, and dysphonia should alert the clinician to the possible need for active airway management. The intraoral examination includes inspection of the palate, teeth, tongue, and gums and palpation with a gloved finger (the latter only if the patient is able to cooperate). The range of motion of the mandible should be determined. If the maximal incisor opening is less than 5 cm, a mandibular fracture may be present. Trismus is likely to indicate a fracture or significant hematoma within the face. If awake, the patient’s impression about the normalcy of bite occlusion is a more sensitive determinant of a fracture of the mandible than the physician’s impression. Being able to perform a tongue blade test (grasping and holding a tongue blade between the teeth while the examiner pulls gently) is associated with greatly reduced probability of mandibular fracture. If the patient is able to crack the tongue blade by biting on both sides of the mouth, the negative predictive value for a mandibular fracture is 95%.49 Injury to the parotid area should raise suspicion of disruption of Stensen’s duct. The opening of the duct opposite the second upper molar should be examined for bleeding while the gland is compressed. If blood is expressed from the duct or the severed ends of the duct are identified within a facial wound, specialized repair over a stent is required to prevent formation of a cutaneous fistula. Otoscopy is performed to evaluate the integrity of the external canal, look for hemotympanum, and assess for otorrhea. Clear fluid from the ear after trauma should raise the possibility of a cerebrospinal fluid (CSF) leak. At the bedside, a drop of the fluid may be placed onto filter paper. A rapidly advancing halo of clear fluid around red blood defines a positive test result. This is a quick bedside test with good sensitivity (>86%) as long as the mix is approximately 50 : 50 between blood and other fluid, but it does not differentiate between CSF and saline, saliva, or other clear fluids.50 The ear should be inspected for subcutaneous hematomas because these need to be drained. The choice of imaging for facial fractures depends on the patient’s stability, the patient’s ability to cooperate, and the availability of various options. The two main options are plain x-ray examination and computed tomography (CT). Fractures are better visualized with CT than with magnetic resonance imaging, so magnetic resonance imaging is not an optimal imaging choice. In patients who cannot cooperate for plain x-ray examination or in whom a fracture or penetrating injury is obvious from the physical examination, CT is the imaging modality of choice.51 For a complete evaluation, CT scans of the face should include coronal and sagittal reconstructions. Interpreting facial CT scans is an art that requires attention to bones, sinuses, orbital contents, and soft tissue and is best handled by radiologists. With the increasing use of CT in emergency medicine and the advent of telemedicine, most 24-hour EDs have access to CT scanners for facial injuries. CT is now the first choice for all patients in whom a midface fracture is suspected. However, when no scanner is available and in patients with low to moderate pretest probability of a midface or maxillary fracture and who are stable and able to cooperate, the current recommendation is for a single screening view (Water’s or occipitomental view), followed by CT if the film is positive for a fracture or air-fluid level in any sinus.52–54 The U shape of the mandible and the presence of nearby bony structures make isolating the mandible on flat film impossible. Simple radiographs of the mandible are less sensitive than panorex radiographs and particularly tend to miss fractures of the condyle (Fig. 42-6). If available, panorex imaging is indicated for isolated mandibular fractures, dental fractures, or fractures of the alveolar ridge. In children, if fracture of the condyle is suspected, coronal CT is more sensitive and specific than panorex studies.55 Although the traditional teaching has been that the mandible’s shape results in two fractures if it is fractured at all (Fig. 42-7), a case series using CT evaluation found that 42% of mandibular fractures were unifocal.56 Figure 42-7 Three-dimensional computed tomography reconstructions of minimally displaced mandibular fractures in the same patient as in Figure 42-5. For patients with complex fractures, new imaging techniques may help improve surgical planning and esthetic outcomes. In displaced orbital fractures, use of CT data to measure orbital volumes has shown that after repair an orbital volume greater than 4% larger than on the unfractured side is associated with visible postoperative enophthalmos.57 This method seems to be useful in predicting which patients might benefit from operative repair.58 In conjunction with more standard two-dimensional facial CT scans, three-dimensional CT scans seem to improve the diagnosis and aid preoperative planning for patients with complex fractures of the midface (Fig. 42-8B).59–62 Patients with suspected ocular injuries may benefit from a bedside ultrasound as a noninvasive and economical diagnostic tool, particularly if there is a need for urgent operative management of other injuries and no time for a dedicated facial CT. The different acoustic impedances of the orbit’s anatomic structures make the modality operator friendly, and an ultrasound of the eye can readily detect vitreous hemorrhage, retinal detachment, and globe rupture (Figs. 42-9 and 42-10). The operator should position the transducer in a transverse orientation, scanning in a cephalad-to-caudad direction, making sure to scan the entire anatomy of the eye, and using special care to minimize the pressure exerted over the eye, especially when evaluating for specific ocular emergencies. Prior findings have suggested that high-resolution ultrasound has at least a 94% correlation with axial and coronal CT imaging in the detection of orbital fractures and emphysema.63,64
Facial Trauma
Perspective
Epidemiology
Principles of Disease
Bones
Eyes
Mouth
Pathophysiology
Clinical Features
Physical Examination
Oropharynx
Ears
Diagnostic Strategies
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Facial Trauma
Only gold members can continue reading. Log In or Register to continue