ACROMIOCLAVICULAR JOINT SEPARATION
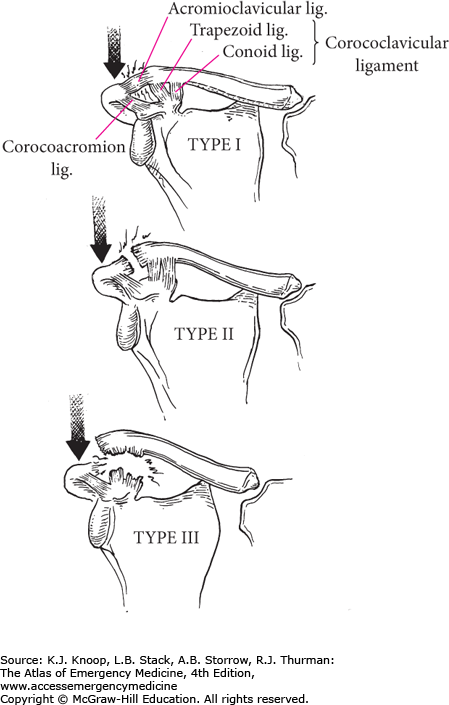
Injury to the acromioclavicular (AC) joint usually results from an impact on the superior aspect of the acromion. The classification system for AC joint includes six types. A type I injury is equivalent to a stretching of the AC ligament. A type II injury consists of tearing of the AC ligaments and stretching of the coracoclavicular ligaments. Complete disruption of the AC and coracoclavicular ligaments is seen in types III to VI.
Patients complain of pain at the AC joint and will actively splint the injured shoulder. Ecchymosis may be present; however, an obvious deformity is not always seen. There is significant tenderness upon palpation of the AC joint.
Standard radiographs should include anteroposterior (AP) and axillary lateral views of the shoulder. Type I injuries will appear normal. Type II injuries may show 0% to 50% displacement at the AC joint but no increase in the coracoclavicular interval. Types III to VI will demonstrate displacement at the AC joint and the clavicle will appear to be displaced superiorly (the acromion actually is rotated inferiorly) 50% to greater than 100% its width when compared with the normal side.
Type I and type II injuries are treated with rest, ice, analgesics, and a simple sling until acute pain with movement is relieved. Treatment of type III injuries may be nonoperative or operative. However, these patients can be discharged from the emergency department in a sling without an emergent orthopedic consult. Types IV, V, and VI are treated operatively. Referral to a musculoskeletal specialist is essential for all AC joint injuries since many patients who initially appear to have minor injuries will have more obvious deformity after the swelling and pain have subsided.
The early AC joint stress radiograph can be negative due to splinting of the shoulder girdle muscles and does not add anything to the acute patient management.
Differentiating between types I and II versus types IV to VI is the goal of the ED physician, since the latter will require an emergency orthopedic consult.
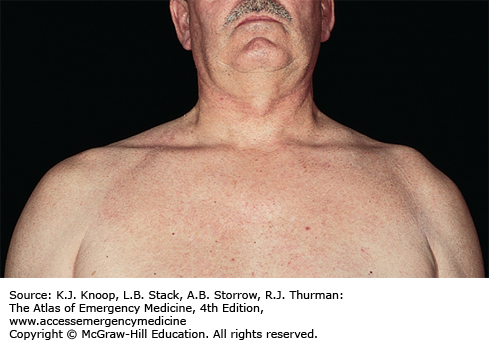
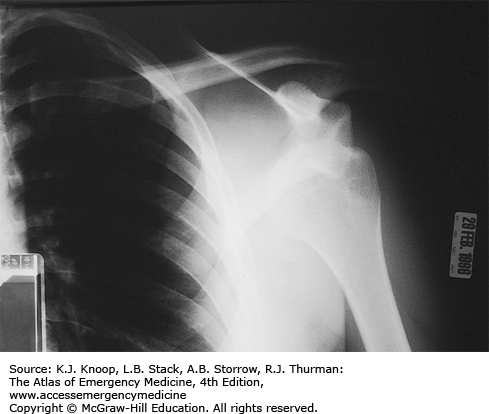
FIGURE 11.4
AC Joint Separation, Third Degree. A wide AC joint and the clavicle displaced from the acromion. (Reproduced with permission from Simon RR, Sherman SC, Koenigsknecht SJ. Emergency Orthopedics: The Extremities. New York: McGraw-Hill; 2007: p 297, Fig. 11-54.)
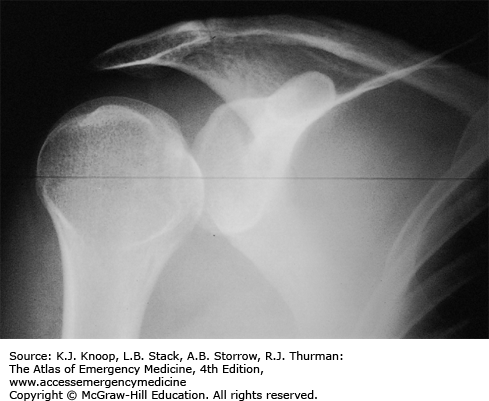
SHOULDER DISLOCATION
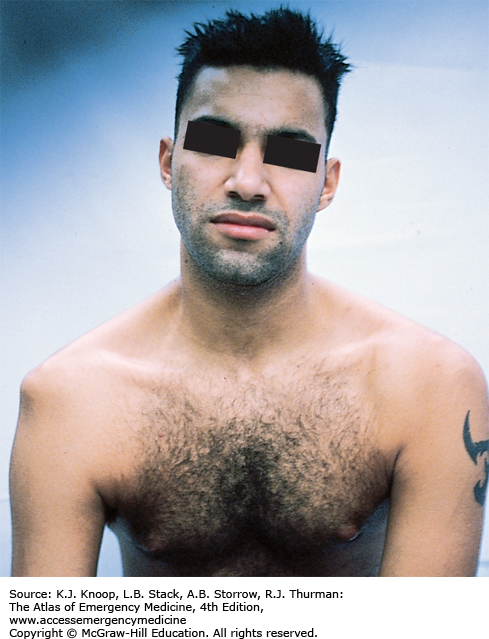
Anterior shoulder dislocations are the most common and frequently caused by falling with the arm externally rotated and abducted. Patients present with the affected extremity held in adduction and internal rotation. Often, they complain of shoulder pain, refuse to move the affected arm, and may support the dislocated shoulder with the other arm. The acromion becomes prominent with loss of the rounded contour of the deltoid. A neurovascular examination of the upper extremity should be performed to rule out associated injury, most commonly of the axillary nerve (sensation over the deltoid) and of the musculocutaneous nerve (sensation on the anterolateral forearm). Vascular injuries have rarely been reported to occur. Standard radiographic examination to evaluate for associated fracture should include AP and either axillary lateral or scapular Y views.
Posterior shoulder dislocations are commonly missed because of subtle radiographic findings. The arm is held internally rotated and slightly abducted. Patients are unable to externally rotate their shoulder. On examination, a posterior prominence exists. Posterior dislocations can occur with a posterior-directed force as seen during grand mal seizures or electric shock.
The Hill-Sachs lesion (an impaction of the humeral head) can occur in up to 50% of patients.
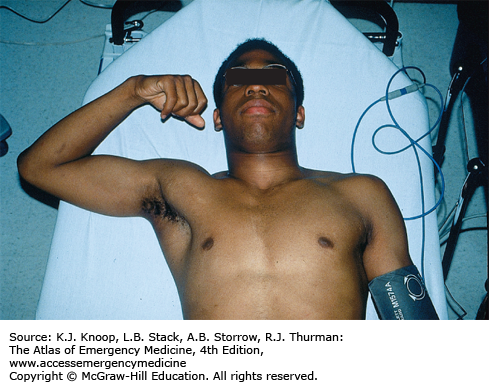
Closed reduction is the treatment for all types of shoulder dislocations and should be completed as soon as possible to avoid avascular necrosis to the humeral head. Due to shoulder girdle spasm, conscious sedation is often required. There are many methods to reduce anterior shoulder dislocations, including Stimson, Rockwood traction and countertraction, and Milch. The basic premise is to apply axial traction, externally rotate, and abduct. Scapular manipulation and the Stimson method are successful techniques, especially in the thin patient. Neurovascular and radiographic examination should occur before and after reduction. The patient should be placed in a sling after reduction and follow-up with a musculoskeletal specialist should be recommended.
Occult, nondisplaced greater tuberosity fracture can be identified on postreduction radiographs. These usually occur during the traumatic event but not seen on initial radiographs. They are not the result of the reduction and usually only identified when there is no bony overlap on the x-rays.
Luxatio erecta is inferior glenohumeral dislocation that is rarely encountered. The humeral head is forced below the inferior aspect of the glenoid fossa due to a hyperabduction of the arm. These patients present with the arm locked fully abducted and externally rotated. Axillary nerve injury is reported to occur in 60%. Vascular injury occurs most frequently with this type of dislocation. Reduction is accomplished with overhead traction.
Posterior shoulder dislocations can be bilateral and are often missed due to preserved symmetry on standard chest x-rays.
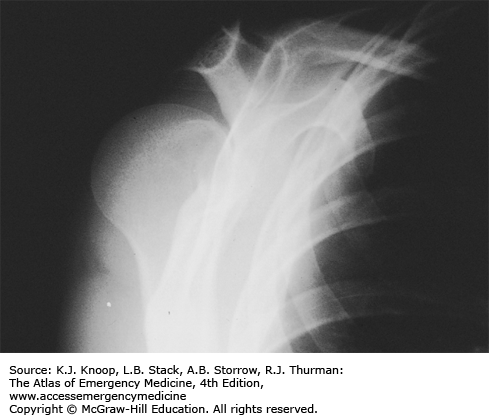
FIGURE 11.8
Posterior Shoulder Dislocation. A scapular Y view of the same patient in Fig. 11.7 confirms the diagnosis. (Photo contributor: Alan B. Storrow, MD.)
ELBOW FRACTURES
Direct trauma or fall on an outstretched hand may result in elbow fractures. The patient may be unable to extend the elbow and have pain on supination/pronation. AP, lateral, and oblique radiographic views visualize most. The radial head should be aligned with the capitellum on all views. The anterior fat pad may be seen on normal radiographs but displacement anteriorly and superiorly (sail sign) suggests effusion or hemarthrosis. The posterior fat pad is not normally visualized and, if seen, is indicative of effusion or hemarthrosis; it is often associated with a radial head fracture in adults.
Supracondylar fractures often occur in pediatric patients. Neurovascular insult occurs in 7%, with the anterior interosseous nerve most commonly injured. This can be checked by having the patient make an “ok” sign. This neuropraxia usually resolves in 6 months. Arterial injury to the brachial artery occurs in approximately 5% to 20%, with less than 1% of these complicated by compartment syndrome. Arteriography is indicated if the radial pulse is decreased after reduction; however, it should not delay operative evaluation.
Capitellum fractures represent less than 1% of adult elbow fractures, occur with high-energy trauma, and are difficult to diagnose radiographically; a CT scan may be required. This fracture is commonly associated with fractures of the radial head.
Treatment of supracondylar fractures is influenced by stability of the fracture pattern as well as associated neurovascular injuries. If neurovascular compromise exists, the emergency physician may need to apply forearm traction to reestablish distal pulses. If the pulse is not restored with traction, emergent operative intervention for brachial artery exploration or fasciotomy is indicated. In children, nondisplaced fractures can be splinted in 90 degrees of flexion. Angulated or displaced fractures often require operative intervention.
Capitellum fractures are treated with immobilization in a posterior long-arm splint with the elbow in 90 degrees flexion and the forearm in supination. Complications of displaced capitellum fractures include arthritis, avascular necrosis, and decreased range of motion.
Radial head fractures can be treated with a sling for comfort and patients should be told to discontinue the sling as early as possible. Fractures that are greater than 2 mm displaced, those that have greater than 20% of articular depression, or open fractures may need operative treatment and should follow up within a week with an orthopedic surgeon.
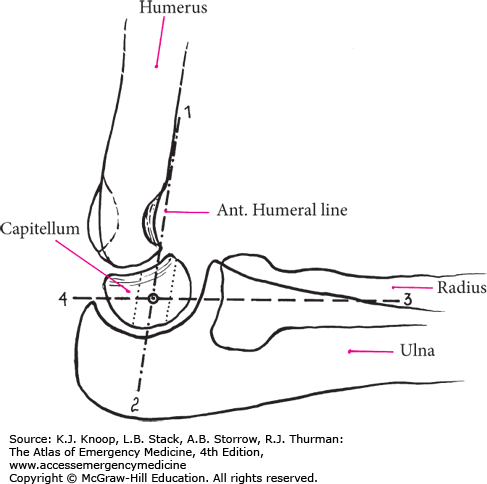
FIGURE 11.11
Radiographic Elbow Relationships. In lateral views, the anterior humeral line (1-2) should bisect the middle third of the capitellum. The radiocapitellar line (drawn through the center of the radius, 3-4) should also pass through the center of the capitellum. Disruption of these relationships may indicate fracture.
An intimal arterial injury may not be initially apparent and frequent radial artery checks are warranted in the pediatric population. Some practitioners opt to admit supracondylar fractures so these neurovascular checks can be done.
Capitellum and radial head fractures often occur together.
The presence of a joint effusion or a posterior fat pad with a history of trauma is presumptive evidence of a fracture.
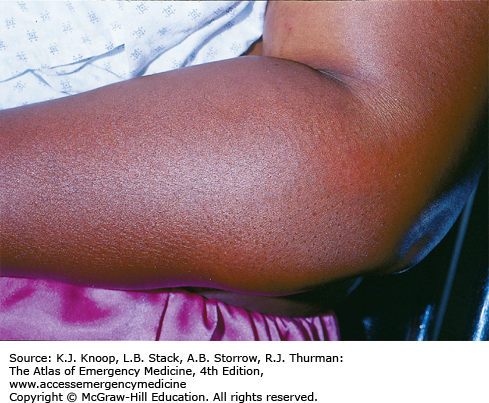
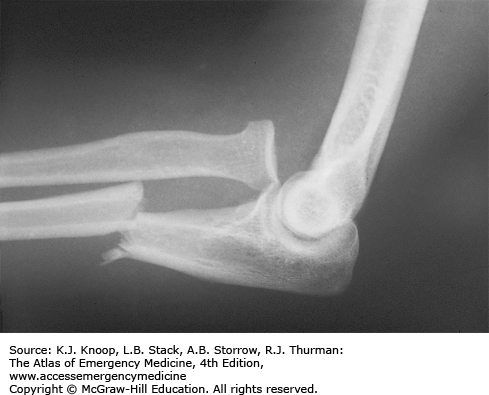
FIGURE 11.13
Supracondylar Fracture. (A) Clinical picture with marked soft tissue swelling in a child with a history of falling on an outstretched arm. (B and C) AP and lateral views of the elbow, demonstrating a distal humerus fracture with posterior displacement of the medial and lateral condyles. (Reproduced with permission from Shah BR, Lucchesi M. Atlas of Pediatric Emergency Medicine. New York: McGraw-Hill; 2006.)
ELBOW DISLOCATION
Elbow dislocations are the second most common major joint dislocation and usually occur posteriorly, although they can be anterior, medial, or lateral. All require immediate reduction to relieve pain and prevent neurovascular compromise. Brachial artery function and ulnar, median, and radial nerve integrity must be evaluated when examining any patient. Elbow dislocations are often associated with a radial head fracture. Patients with posterior dislocation present with their elbow held in flexion and examination reveals a swollen, tender, and deformed elbow with a prominent olecranon. Anterior dislocations, though rare, present with the elbow extended with the forearm supinated and elongated.
Radiographic evaluation should include an AP and a lateral view. The presence of fractures should be noted, as this may complicate reduction.
Most patients require conscious sedation prior to reduction. Posterior dislocations are accomplished by applying posterior pressure to the humerus while an assistant applies longitudinal forearm traction. Alternatively, the patient is placed in the prone position so the humerus hangs perpendicular to the stretcher. A 5- to 10-lb weight is applied to the wrist or axial traction is applied to the wrist while the elbow at the humerus is stabilized. After a few minutes, the olecranon slips back into place. It is possible to entrap the nerve while attempting reduction, so neurovascular integrity must be checked before and after reduction. If this occurs, an orthopaedic surgeon should be consulted immediately. After successful reduction, the elbow should be immobilized in 90 degrees of flexion in a posterior splint and sling. Elbow dislocations with associated fractures may make closed reduction difficult and also leave the joint unstable. In these cases, consultation with an orthopedic surgeon is recommended prior to reduction attempts.
The ulnar nerve is the most common nerve injured.
The olecranon should form a straight line with the two epicondyles when the elbow is extended. At 90 degrees of flexion, the olecranon and the two epicondyles should form a triangle. This relationship is disrupted in the dislocated elbow.
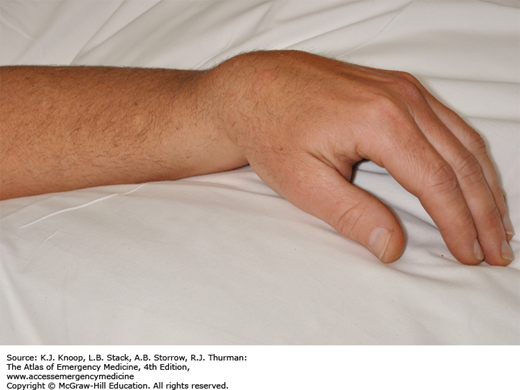
BICEPS TENDON RUPTURE
The biceps has two origins, crosses the shoulder and elbow joints, and inserts on the proximal radius. The long head of the biceps is much more susceptible to injury and rupture may occur anywhere along its route. Clinically, patients with proximal rupture present with pain along the anteromedial aspect of the shoulder. On inspection, ecchymosis is often acutely noted. Muscle retraction within the arm may create a “Popeye” deformity. Due to the two proximal attachments, the short head of the biceps can allow for maintenance of forearm supination strength. Rupture may also occur at the tendon insertion into the radial tuberosity at the elbow. This diagnosis is made on the basis of a history of a painful, tearing sensation in the antecubital region. A snap or pop may also occur. The ability to palpate the tendon in the antecubital fossa may indicate partial tearing.
Proximal and distal biceps tendon ruptures can be discharged with a sling, pain control, physical therapy, and referral for operative repair consideration. Distal biceps tendon ruptures often require surgical management due to the significant loss of forearm supination strength. Partial proximal biceps tendon ruptures should also be referred to a specialist.
Functional deficits from a long head rupture are usually temporary and are influenced by coexistent tears.
Biceps rupture occurs most commonly in the dominant extremity of men between 40 and 60 years of age when an unexpected extension force is applied to the flexed arm.
FOREARM FRACTURES
Fractures of the wrist and elbow usually involve a fall onto the outstretched arm, while isolated fractures of the ulnar shaft are more commonly from a direct blow. AP and lateral views of the wrist, forearm, and elbow are required when a forearm fracture is suspected. Functional deficits in the hand are important clues to identification of occult injury to forearm neurovascular structures, and could require immediate surgical intervention. The Monteggia fracture-dislocation is a fracture of the ulna (usually proximal third) with an associated proximal radial head dislocation; it is occasionally associated with radial nerve injury.
Galeazzi fracture-dislocation is a fracture of the distal one-third of the radius with dislocation of the distal radioulnar joint. It occurs three times more often than a Monteggia fracture and can be associated with ulnar nerve injury.
Isolated fractures of the ulna’s middle third may result from direct trauma, while the forearm is used to block the blow (nightstick fractures). Fractures of the forearm may result in compartment syndrome.
Both Monteggia and Galeazzi fracture-dislocations require emergent orthopedic consultation and are treated with immobilization in a long-arm splint (with elbow flexed at 90 degrees). The forearm is placed in a neutral position for a Monteggia fracture and supinated for a Galeazzi fracture. Treatment is usually surgical for both injuries, although children may be treated by reduction and casting.
Any ulnar fracture with greater than 10 degrees of angulation or with a bony fragment displaced more than 50% usually requires surgical correction.
Do not be satisfied with the diagnosis of an isolated proximal third ulnar shaft fracture. A line drawn through the radial shaft and head must align with the capitellum in all views to exclude dislocation.
An ulnar styloid base fracture, if found, can be a clue to a Galeazzi fracture.
Since the radius and the ulna create a ring, injury to one of the bones of the forearm is often associated with fracture or dislocation of the other. Consequently, upon recognition, one must continue to seek out the other half of the injury by examining both the elbow and wrist joints.
FRACTURES OF THE DISTAL RADIUS
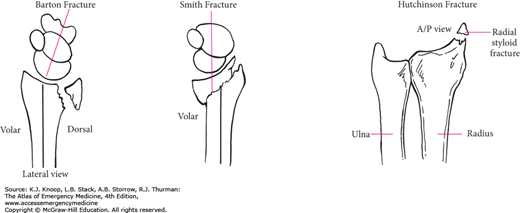
Falls on an outstretched arm are common and, often, the radius is first to fracture. If there is a supinating component to the fall, the distal ulna may also fracture. In the elderly, distal radius fractures are usually extra-articular metaphyseal fractures, whereas in younger patients they are usually intra-articular with displacement of the joint surface. There are four types of radial fractures, associated with commonly known eponyms: Colles, Smith, Barton, and Hutchinson (chauffeur).
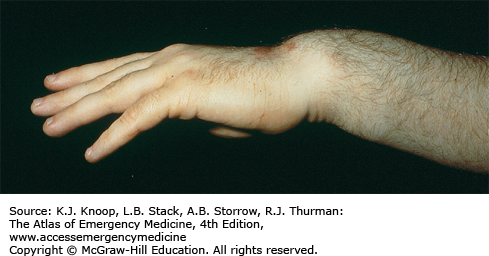
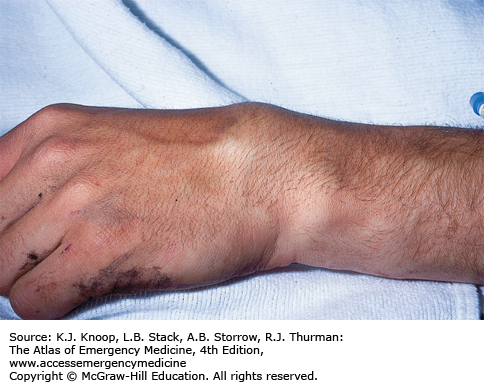
Colles fracture is the most common. There is dorsal displacement of the distal fragment and apex palmer angulation of the distal fracture fragments; on examination, a “dinner fork” deformity is often described.
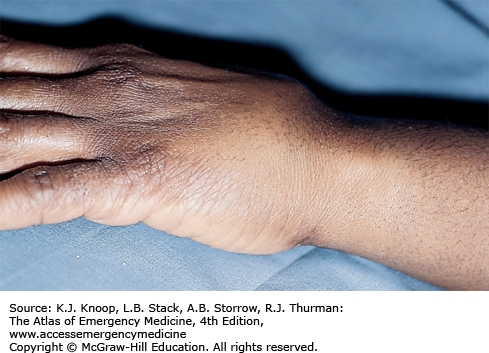
The Smith fracture is of the distal metaphysis with volar displacement and apex dorsal angulation. This usually results from a blow to the dorsum of the wrist or a hyperflexion injury. Examination reveals a reverse dinner fork deformity. Barton fracture is a fracture of the dorsal or palmer rim of the distal radius. It may be associated with dislocation of the radiocarpal joint. A Hutchinson fracture is due to a direct impact to, or an avulsion of, the radial styloid.
Evaluation requires AP, lateral, and oblique views. Orthopedic consultation is required for comminuted, displaced, unstable, or open fractures, as well as those with >20 degrees of angulation or more than 1 cm of shortening. The patient can be immobilized in a sugar-tong splint. Detailed discharge instructions should be given regarding symptoms of median nerve impingement, including paresthesias and hand weakness, which should prompt return evaluation.
All fractures of the distal radius must be evaluated for median nerve function before and after reduction.
Colles fractures warrant a high index of suspicion for intra-articular injury, especially when a radial styloid fracture is noted.
With a Hutchinson fracture, associated ligamentous injuries should be sought, especially scapholunate dissociation, and perilunate or lunate dislocation.
CARPAL AND CARPOMETACARPAL DISLOCATIONS
Carpal and carpometacarpal dislocations are serious wrist injuries usually occurring from hyperextension. Patients complain of decreased range of motion, pain, swelling, and ecchymosis.
Lunate dislocation can occur in a palmer or dorsal position with the lunate displaced relative to the other carpals (“spilled tea cup sign”). The normal lunoradial relationship is disrupted. The median nerve is commonly involved.
If the lunoradial articulation is intact and the other carpal bones are dislocated relative to the lunate, it is termed a perilunate dislocation.
Another potentially serious injury is scapholunate dissociation, often mistakenly diagnosed as a sprained wrist. Although examination may be unremarkable except for wrist pain, an AP radiograph reveals a widening of the scapholunate joint space. A space of ≥4 mm should prompt suspicion of disruption of the scapholunate ligament. The lateral radiograph may reveal an increase of the scapholunate angle to greater than 60 to 65 degrees (normal 45-50 degrees). All these injuries may present with concomitant fractures of the carpal bones or distal forearm.
Carpometacarpal dislocations of the index and long metacarpals are fortunately rare since functional loss is often marked. Thumb, ring, and small finger carpometacarpal dislocations are more common and are frequently missed injuries.
Initial management includes adequate radiographic evaluation followed by ice, elevation, and splinting. Referral to a hand specialist is essential for adequate reduction and long-term care.
A true lateral wrist radiograph best demonstrates a lunate dislocation by exhibiting the usual cup-shaped lunate bone as lying on its side and displaced either dorsally or palmerly.
On lateral wrist radiographs, the metacarpal, capitate, lunate, and radius should all align within a line drawn through their long axes. If this is not found, some element of dislocation, subluxation, or ligamentous instability likely exists.
Carpometacarpal dislocations are frequently difficult to reduce and require open reduction and fixation in approximately 50%.
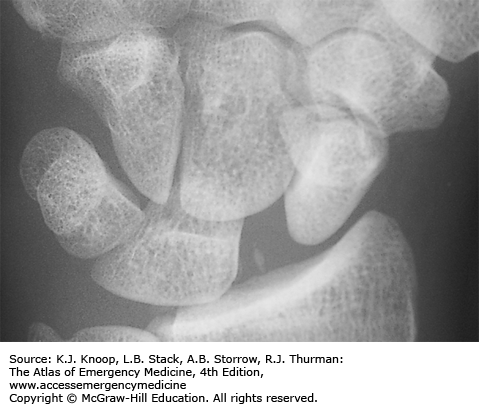
FIGURE 11.27
Lunate Dislocation. (A) PA wrist view shows disruption of the carpal arcs. (B) Lateral reveals volar displacement of the lunate. The radius, capitate, and third metacarpal align. (Reproduced with permission of Block J, Jordanov MI, Stack LB, Thurman RJ. The Atlas of Emergency Radiology. McGraw-Hill; 2013.)
FIGURE 11.31
Perilunate Dislocation. (A) PA wrist view shows disruption of the carpal arcs. (B) Lateral reveals the lunate aligns with the distal radius, while the capitate and metacarpals are dislocated dorsal to the lunate. (Reproduced with permission of Block J, Jordanov MI, Stack LB, Thurman RJ. The Atlas of Emergency Radiology. McGraw-Hill; 2013.)
SCAPHOID FRACTURE
The scaphoid is the most common carpal bone fractured. Injuries result from either a fall on an outstretched dorsiflexed hand or an axial load along the thumb’s metacarpal. Misdiagnosis of a scaphoid fracture can result in delayed healing or avascular necrosis due to lack of a direct blood supply to the proximal portion of the bone. Tenderness on palpation of the anatomic snuffbox is a common finding. Examination of the wrist in ulnar deviation exposes more of the scaphoid to palpation within the anatomic snuffbox. Eliciting pain in this area when the patient resists supination or pronation of the hand, or pain with axial pressure directed along the thumb’s metacarpal, is also suggestive of injury.
Negative radiographs do not rule out an occult scaphoid fracture.
Initial management includes adequate radiographic evaluation followed by ice, elevation, and a thumb spica splint. Referral to a hand specialist is essential.
Patients in whom there is a clinical suspicion of an occult scaphoid fracture should receive a thumb spica splint and a repeat examination in 7 to 10 days.
Avascular necrosis can lead to disabling arthritis.
MRI is the gold standard for diagnosis.
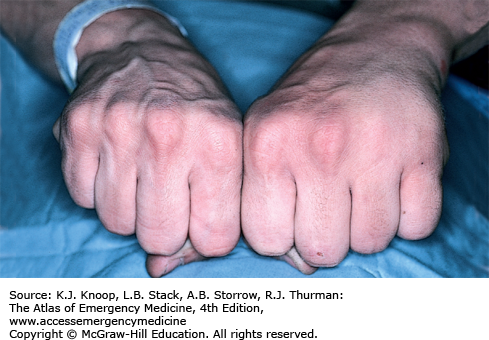
CLENCHED FIST INJURY (FIGHT BITE)
The clenched fist injury classically occurs when the metacarpophalangeal (MCP) joint contacts human teeth, resulting in a laceration. Many patients will not divulge the true circumstances surrounding the injury; therefore, all wounds at the MCP joint must be considered a clenched fist injury until proven otherwise. These wounds occur most often in the dominant hand. Serious complications can result, including infection, loss of function, and amputation. Most wounds are polymicrobial. Patients who present early may have little evidence of intra-articular injury on examination, whereas those who present more than 18 hours after injury are more likely to have evidence of infection, including pain, swelling, erythema, and purulent drainage.
All wounds should be irrigated, debrided, explored, and immobilized. Patients should receive antibiotics directed at both oral and skin flora. Tetanus prophylaxis is given if needed. Radiographs should be obtained to evaluate for fractures and foreign bodies. These wounds should never be closed and should be allowed to heal by secondary intention. Reliable patients who present early, without evidence of infection or significant comorbidity, and no involvement of bone, joint, or tendon, may be treated on an outpatient basis with 24-hour follow-up. Any patient who does not meet these requirements must be hospitalized for intravenous antibiotics and wound care.
Complications include cellulitis, lymphangitis, septic arthritis, abscess formation, osteomyelitis, and flexor tenosynovitis.
All wounds need to be examined in full flexion and extension to evaluate for tendon injuries.
BOXER’S FRACTURE
A boxer’s fracture is a metacarpal neck fracture of the fifth digit, which commonly occurs after a direct blow to the MCP joints of the clenched fist. The apex of the fractured metacarpal bone is dorsal. On physical examination, the “knuckle” is flattened and can be palpated on the volar surface.
Examination should address neurovascular integrity and rotational deformity. Rotational deformity is evaluated by having the patient flex the digits at the proximal interphalangeal (PIP) and distal interphalangeal (DIP) joints; the four digits should point towards the scaphoid. If the involved digit overlaps another digit or does not point toward the scaphoid, a rotational deformity is present and needs to be corrected.
Radiographic evaluation is needed to determine the degree of angulation. Angular deformity of up to 40 degrees is acceptable for the fourth and fifth metacarpals, while 10 to 20 degrees is acceptable for the second and third metacarpals. Closed reduction for angulation that exceeds the limits should be attempted in the ED under appropriate nerve block.
Treatment includes ice, elevation, and immobilization in a short-arm gutter splint in the intrinsic plus position. For reduction, the MCP joint is held in 90 degrees of flexion and pressure exerted on the metacarpal head, directed dorsally. Simultaneously, the apex of the fracture is directed palmerly. Postreduction radiographs are needed to ensure adequate reduction. Early follow-up (within 7 days) with a hand specialist is essential, as the reduction can be lost with simple splinting. Higher degrees of angulation and fractures with any rotational deformity require follow-up for possible open reduction and fixation.
Subtle malrotation can be recognized by looking at the alignment of the nail beds with the digits flexed.
Complications include collateral ligamentous damage, extensor injury damage, and malposition or clawing of the fingers secondary to incomplete reduction.
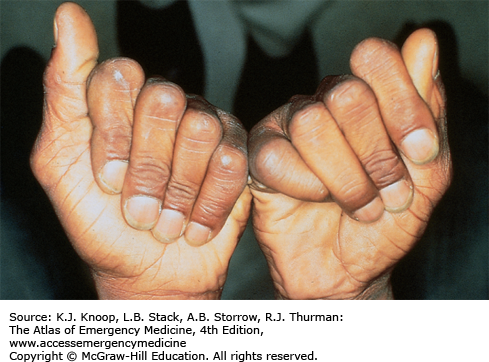
PERIPHERAL NERVE INJURY
Chronic ulnar nerve injury results in the classic claw-hand (intrinsic minus) deformity due to atrophy and contracture of the lumbrical and interosseus hand muscles. The deformity is formed by hyperextension of the MCP joint and flexion at the PIP and DIP joints of the fourth and fifth digits. There is wasting of the interosseous and hypothenar muscles, as well as the hypothenar eminence. The acutely injured patient is unable to abduct or adduct the digits.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree