Fig. 7.1
Air flow during the three steps of cough effort: (1) deep inspiration, (2) compression step with glottis occlusion and contraction of expiratory muscles, and (3) exhalation step with sudden glottis opening and forced expiration characterized by the peak of expiratory flow (PCEF)
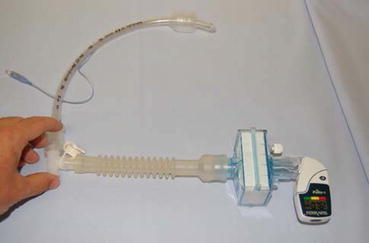
Fig. 7.2
Measure of the peak cough expiratory flow with the PiKo-1 (E-Ness, Aix-en-Provence, France). The patient, who was in the semi-recumbent position, was instructed to inspire deeply through a three-way connector positioned between the proximal tip of the tracheal tube and the PiKo-1. The external port of the connector was then occluded, and the patient was instructed to cough as strongly as possible through the tracheal tube
7.2 Predicting Extubation Outcome
Some studies found an association between the volume of secretions and extubation outcome [4, 7], whereas others did not [3, 6]. In a study with a large sample size, the frequency of secretions during the last 24 h was associated with extubation outcome [5]. Moreover, when focusing on patients with excessive secretions, the patients requiring suctioning every 2 h or more were at risk of extubation failure [4, 9].
When the evaluation of cough is subjective, the results are conflicting: in some studies the efficacy of cough is associated with outcome of extubation [4], in other studies not [3, 5]. Similarly, the white card test was either predictive of extubation outcome [4] or not [7]. Conversely, all studies that objectively measured cough strength by PCEF found a significant association with extubation outcome [6–8, 11]: a low PCEF before extubation increases the risk of extubation failure by five- to sevenfold. The cut-off value of PCEF differed depending on the device used.
7.3 Impact on the Decision to Extubate
As stated by the International Consensus Conference 2007 on weaning from mechanical ventilation [2], it is recommended that patients who successfully pass a spontaneous breathing trial should not be extubated if the amount of respiratory secretions is excessive; the need to suction the patient every 2 h or less seems here a reliable criteria.
Concerning the evaluation of cough strength by the measurement of PCEF, the positive predictive value of the test was low in all studies. For example, in a study using an electronic flowmeter, the risk of extubation failure was 3.5 % for the patients with a PCEF > 35 l/min and 24 % for those who did not cough on demand or with a low PCEF < 35 l/min (RR = 6.9, 95 % CI 2–24, p = 0.002) [8]. Therefore, a low PCEF does not preclude extubation but selects patients who are “at risk” and need specific management after extubation.
7.4 Management after Extubation
Noninvasive ventilation (NIV) has been proposed as a prophylactic measure after extubation for patients who are at high risk for reintubation. Three studies showed a beneficial effect, with one study showing a reduction of reintubation rate [12] and the others a reduction in the rate of respiratory failure post-extubation, which was the primary end-point [13, 14]. In the study by Nava et al. [12], a weak cough before extubation was one of the criteria for enrollment. In a before-after study, our group evaluated the impact on extubation outcome of identifying weak cough at extubation by the measure of PCEF and assisting these patients with NIV [15]. Two cohorts of patients were compared: a historical cohort of 141 patients in 2005–2006, where the physician was blinded to the value of PCEF (blinded cohort) and no prophylactic NIV was applied, and an open cohort of 151 patients in 2012–2013, where prophylactic NIV was applied to the patients with PCEF < 35 l/min or inability to cough on demand. Extubation failure was defined by the need of reintubation within 48 h following extubation. The rate of extubation failure was significantly reduced: 11/55 (20 %) in the blinded cohort versus 3/51 (6 %) for the open cohort (p = 0.043), without increasing the total duration of ventilator assistance. This result suggests that NIV could be useful when applied systematically after extubation to patients with a weak cough before extubation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




