Anemia is due to loss of red blood cells (RBCs) by hemorrhage, increased destruction of RBCs, or impaired production of RBCs.
![]() Bleeding disorders from congenital or acquired abnormalities in the hemostatic system can result in excessive hemorrhage, excessive clot formation, or both.
Bleeding disorders from congenital or acquired abnormalities in the hemostatic system can result in excessive hemorrhage, excessive clot formation, or both.
CLINICAL FEATURES
![]() The rate of the development of the anemia, the extent of the anemia, and the ability of the cardiovascular system to compensate for the decreased oxygen-carrying capacity determine the severity of the patient’s symptoms and clinical presentation.
The rate of the development of the anemia, the extent of the anemia, and the ability of the cardiovascular system to compensate for the decreased oxygen-carrying capacity determine the severity of the patient’s symptoms and clinical presentation.
![]() Patients may complain of palpitations, dizziness, postural faintness, easy fatigability, exertional intolerance, and tinnitus.
Patients may complain of palpitations, dizziness, postural faintness, easy fatigability, exertional intolerance, and tinnitus.
![]() On physical examination, patients may have pale conjunctiva, skin, and nail beds.
On physical examination, patients may have pale conjunctiva, skin, and nail beds.
![]() Tachycardia, hyperdynamic precordium, and systolic murmurs may be present. Tachypnea at rest and hypotension are late signs.
Tachycardia, hyperdynamic precordium, and systolic murmurs may be present. Tachypnea at rest and hypotension are late signs.
![]() Use of ethanol, prescription drugs, and recreational drugs may alter the patient’s ability to compensate for the anemia.
Use of ethanol, prescription drugs, and recreational drugs may alter the patient’s ability to compensate for the anemia.
![]() Risk factors for underlying bleeding disorders include a family history of bleeding disorder, history of liver disease, and use of aspirin, nonsteroidal anti-inflammatory drugs, ethanol, warfarin, or certain antibiotics.
Risk factors for underlying bleeding disorders include a family history of bleeding disorder, history of liver disease, and use of aspirin, nonsteroidal anti-inflammatory drugs, ethanol, warfarin, or certain antibiotics.
![]() Signs of platelet disorders include mucocutaneous bleeding (including petechiae, ecchymoses, purpura, and epistaxis), gastrointestinal or genitourinary bleeding, or heavy menstrual bleeding.
Signs of platelet disorders include mucocutaneous bleeding (including petechiae, ecchymoses, purpura, and epistaxis), gastrointestinal or genitourinary bleeding, or heavy menstrual bleeding.
![]() Signs of coagulation factor deficiencies include delayed bleeding, hemarthrosis, or bleeding into potential spaces (eg, retroperitoneum). Patients with combined abnormalities of platelets and coagulation factors, such as disseminated intravascular coagulation, present with both mucocutaneous and deep space bleeding.
Signs of coagulation factor deficiencies include delayed bleeding, hemarthrosis, or bleeding into potential spaces (eg, retroperitoneum). Patients with combined abnormalities of platelets and coagulation factors, such as disseminated intravascular coagulation, present with both mucocutaneous and deep space bleeding.
DIAGNOSIS AND DIFFERENTIAL
![]() Decreased RBC count, hemoglobin, and hematocrit are diagnostic of anemia. Hemoccult examination, complete blood cell count, reticulocyte count, review of RBC indices, and examination of peripheral blood smear are necessary for the initial evaluation of the patient with anemia (Table 135-1).
Decreased RBC count, hemoglobin, and hematocrit are diagnostic of anemia. Hemoccult examination, complete blood cell count, reticulocyte count, review of RBC indices, and examination of peripheral blood smear are necessary for the initial evaluation of the patient with anemia (Table 135-1).
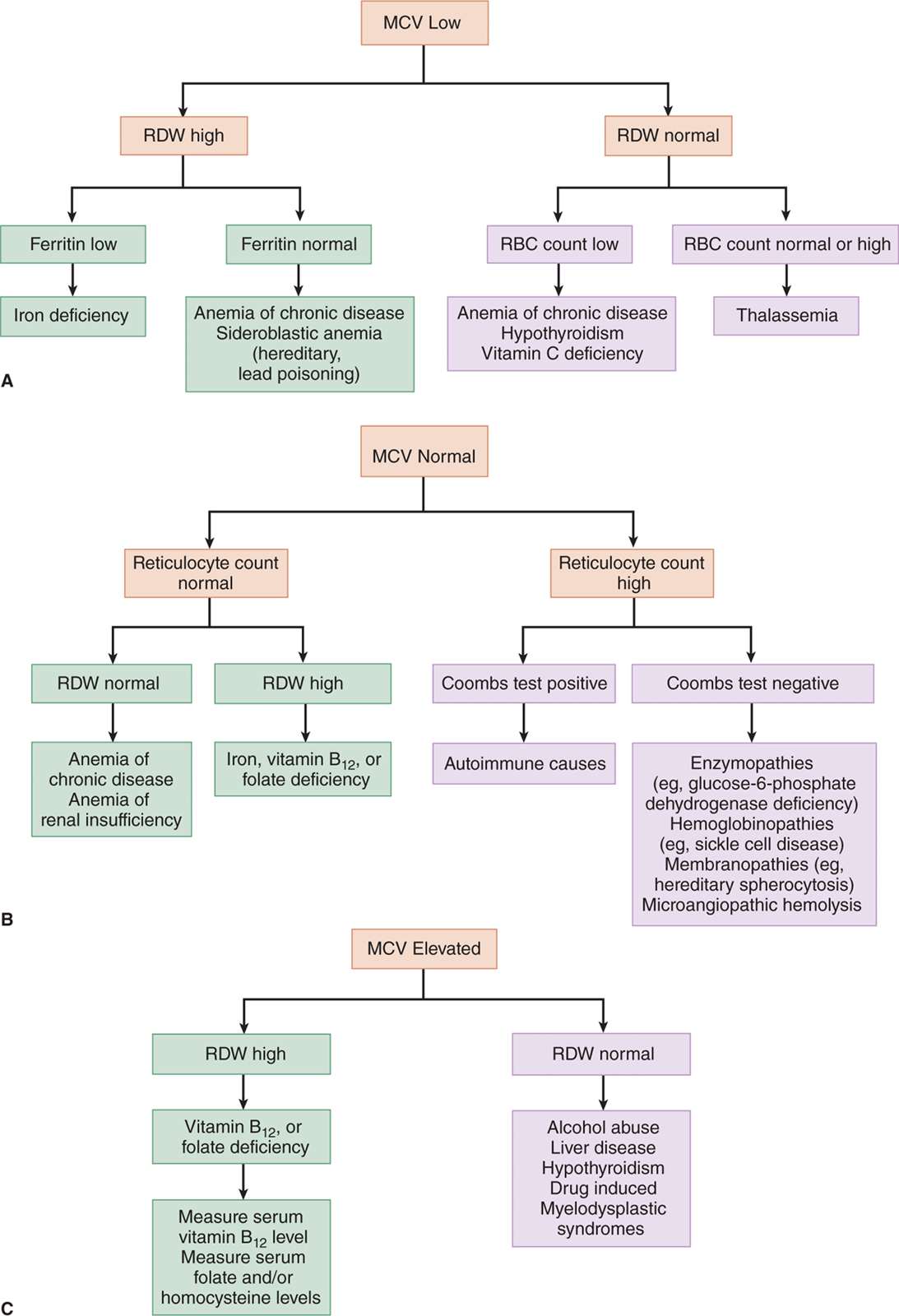
![]() The mean cellular volume and reticulocyte count can assist in classifying the anemia and can aid in differential diagnosis (Fig. 135-1).
The mean cellular volume and reticulocyte count can assist in classifying the anemia and can aid in differential diagnosis (Fig. 135-1).
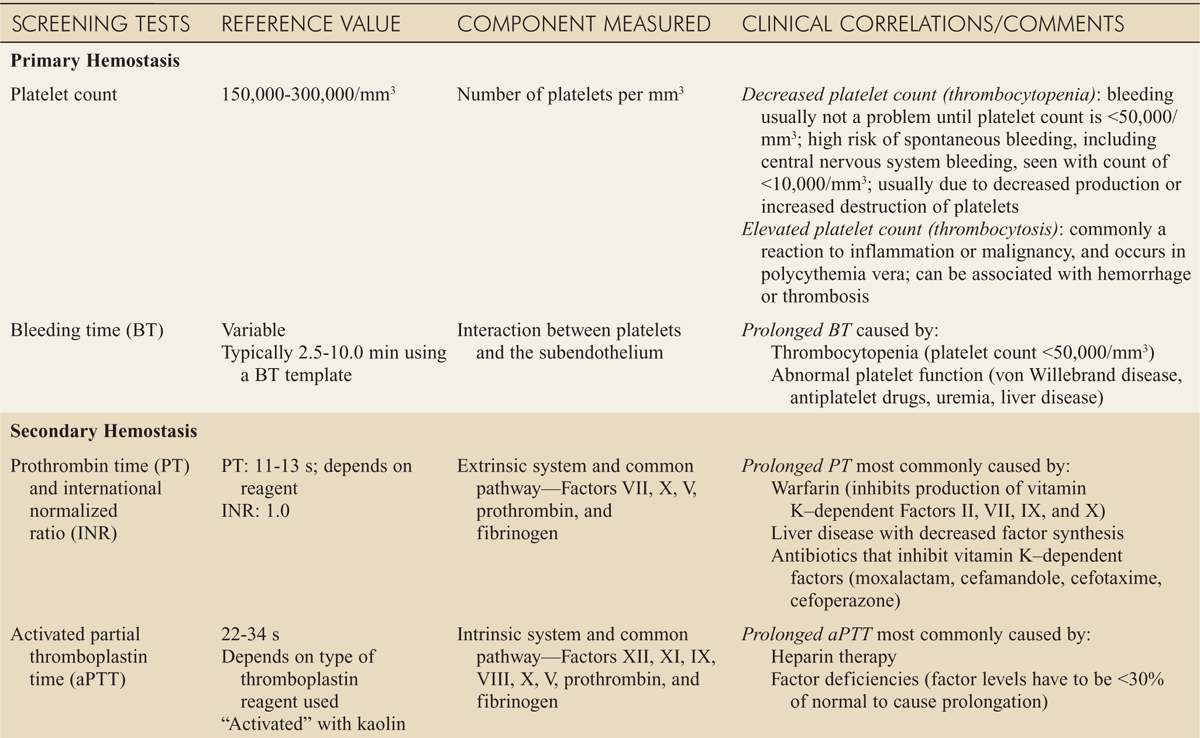
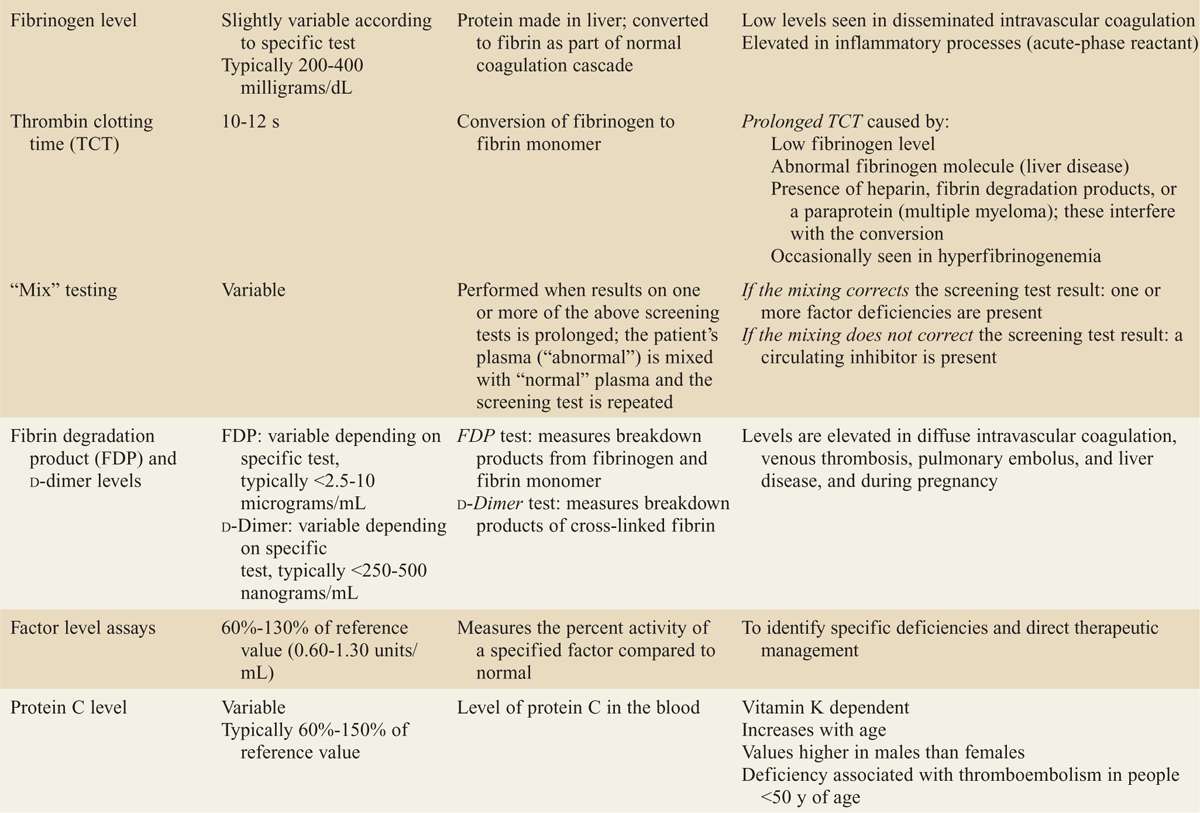
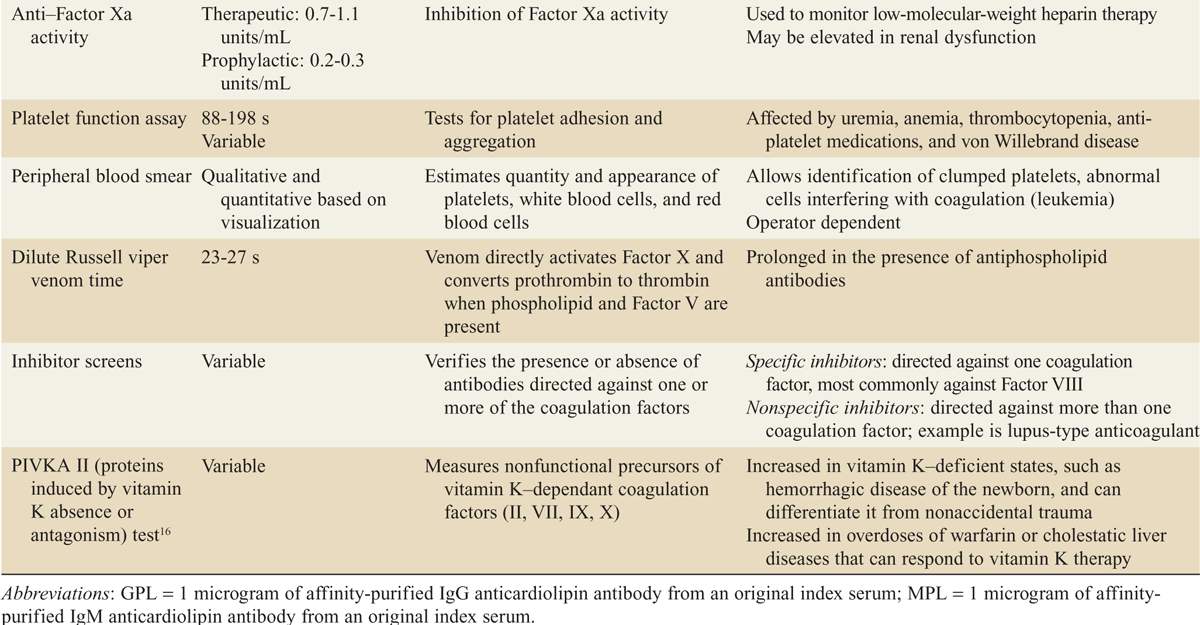
![]() Complete blood cell count, platelet count, prothrombin time, and partial thromboplastin time are necessary for the initial evaluation of the patient with a suspected bleeding disorder (Table 135-2).
Complete blood cell count, platelet count, prothrombin time, and partial thromboplastin time are necessary for the initial evaluation of the patient with a suspected bleeding disorder (Table 135-2).
EMERGENCY DEPARTMENT CARE AND DISPOSITION
![]() Emergent priorities remain airway, breathing, and circulation. Hemorrhage should be controlled with direct pressure.
Emergent priorities remain airway, breathing, and circulation. Hemorrhage should be controlled with direct pressure.
![]() Type- and cross-matched blood should be ordered if blood transfusion is anticipated. Packed RBCs should be transfused in symptomatic patients and those who are hemodynamically unstable
Type- and cross-matched blood should be ordered if blood transfusion is anticipated. Packed RBCs should be transfused in symptomatic patients and those who are hemodynamically unstable
![]() Patients with anemia and ongoing blood loss should with be admitted to the hospital for further evaluation and treatment.
Patients with anemia and ongoing blood loss should with be admitted to the hospital for further evaluation and treatment.
![]() Patients with chronic anemia or newly diagnosed anemia with unclear etiology require admission if they are hemodynamically unstable, hypoxic, or acidotic, or demonstrate cardiac ischemia
Patients with chronic anemia or newly diagnosed anemia with unclear etiology require admission if they are hemodynamically unstable, hypoxic, or acidotic, or demonstrate cardiac ischemia
![]() Hematology consultation is warranted in patients with suspected bleeding disorders and anemia of unclear. etiology.
Hematology consultation is warranted in patients with suspected bleeding disorders and anemia of unclear. etiology.
TABLE 135-1 Laboratory Tests in the Evaluation of Anemia
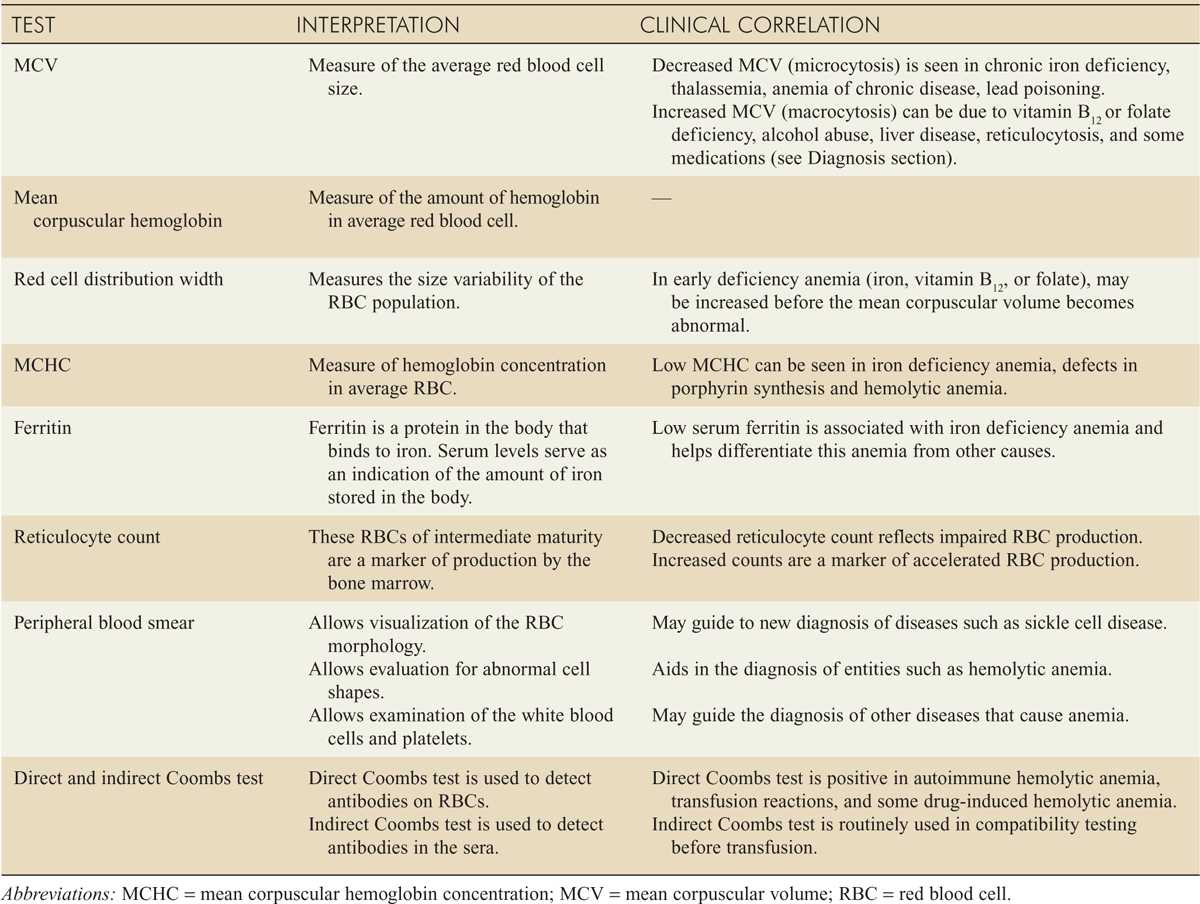
FIG. 135-1. A. Evaluation of microcytic anemia. MCV = mean corpuscular volume; RBC = red blood cell; RDW = red cell distribution width. B. Evaluation of normocytic anemia. MCV = mean corpuscular volume; RDW = red cell distribution width. C. Evaluation of macrocytic anemia. MCV = mean corpuscular volume; RDW = red cell distribution width.
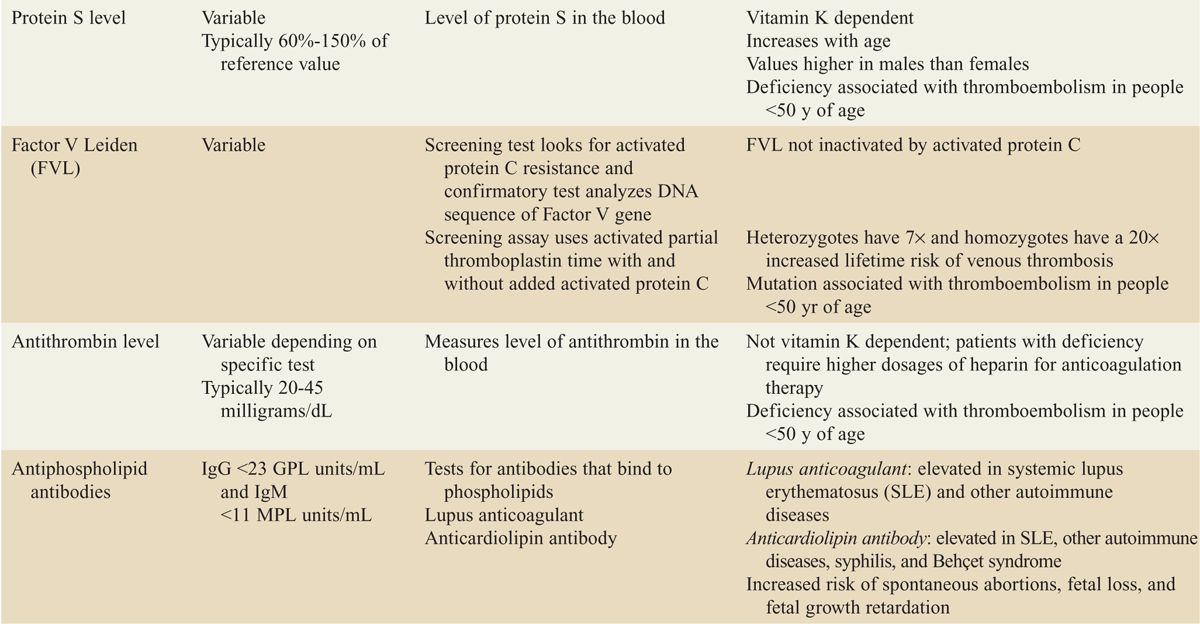
TABLE 135-2 Initial Tests of Hemostasis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree