Traumatic wounds are common reasons for visits to emergency departments.
PATHOPHYSIOLOGY
![]() The mechanism of injury will help identify risk of foreign body, contamination, and wound complication.
The mechanism of injury will help identify risk of foreign body, contamination, and wound complication.
![]() A foreign body sensation increases the likelihood of a retained foreign object.
A foreign body sensation increases the likelihood of a retained foreign object.
![]() Predictive factors for infection include: location, depth, configuration, contamination, and patient age.
Predictive factors for infection include: location, depth, configuration, contamination, and patient age.
![]() Blunt forces compress the skin against underling bone, while sharp objects produce shear forces resulting in skin damage.
Blunt forces compress the skin against underling bone, while sharp objects produce shear forces resulting in skin damage.
![]() Crush injuries are more likely to cause wound infection due to greater tissue damage.
Crush injuries are more likely to cause wound infection due to greater tissue damage.
![]() Low-energy impact injuries may result in hematoma formation. These require aspiration or incision and drainage if they fail to resorb spontaneously.
Low-energy impact injuries may result in hematoma formation. These require aspiration or incision and drainage if they fail to resorb spontaneously.
CLINICAL FEATURES
![]() Document important medical conditions such as diabetes, renal disease, immunosuppression, malnutrition, and connective tissue disorders that impact wound healing.
Document important medical conditions such as diabetes, renal disease, immunosuppression, malnutrition, and connective tissue disorders that impact wound healing.
![]() Most states have regulations requiring reporting of injuries that result from intentional acts.
Most states have regulations requiring reporting of injuries that result from intentional acts.
![]() Bacterial growth increases from time of injury to wound closure.
Bacterial growth increases from time of injury to wound closure.
![]() Consider time from injury to presentation, wound etiology, anatomic location, degree of contamination, host risk factors, and the importance of cosmetic appearance in assessing the decision to close wounds.
Consider time from injury to presentation, wound etiology, anatomic location, degree of contamination, host risk factors, and the importance of cosmetic appearance in assessing the decision to close wounds.
![]() Wounds at high risk for infection should be considered for delayed primary closure after 4 days.
Wounds at high risk for infection should be considered for delayed primary closure after 4 days.
DIAGNOSIS AND DIFFERENTIAL
![]() A complete examination, including neurovascular assessment, should be documented prior to analgesia or anesthesia.
A complete examination, including neurovascular assessment, should be documented prior to analgesia or anesthesia.
![]() A thorough visual inspection to the full depth and length of the wound and palpation will minimize missed foreign bodies, tendon and nerve injuries; such missed injuries are a common cause of litigation.
A thorough visual inspection to the full depth and length of the wound and palpation will minimize missed foreign bodies, tendon and nerve injuries; such missed injuries are a common cause of litigation.
![]() Consider injecting a wound that extends over a joint to determine the integrity of the joint space.
Consider injecting a wound that extends over a joint to determine the integrity of the joint space.
![]() Consider radiographs to detect foreign bodies. Ultrasound may be used for non-radiopaque foreign bodies (Fig. 11-1).
Consider radiographs to detect foreign bodies. Ultrasound may be used for non-radiopaque foreign bodies (Fig. 11-1).
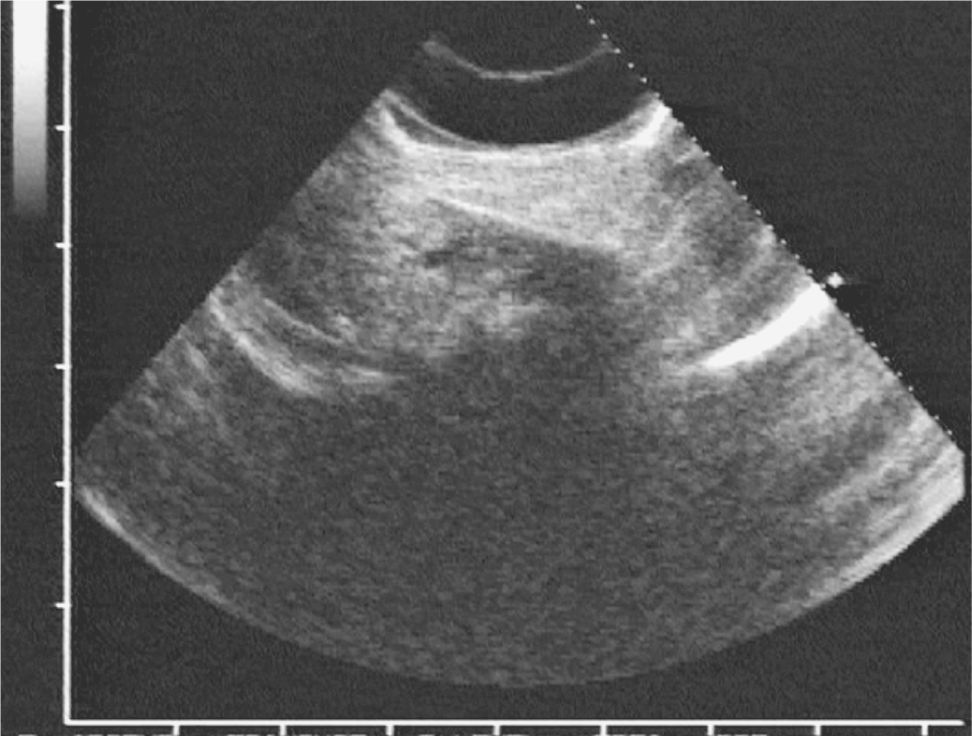
FIG. 11-1. Long-axis sonogram of a wooden foreign body in a patient’s foot. The wood fragment is a hyperechoic linear structure that slants to the right; a prominent posterior acoustic shadow is seen beneath the wood fragment. (Reproduced with permission from Dewitz A, Frazee BW. Soft tissue. In: Ma OJ, Mateer JR, Blaivas M. eds. Emergency Ultrasound, 2nd ed. Figure 16–50. Copyright © 2008 by the McGraw-Hill Companies, Inc. All rights reserved.)
EMERGENCY DEPARTMENT CARE AND DISPOSITION
![]() Wound preparation is the most important step for adequate evaluation of the wound, prevention of infection, and optimal cosmetic outcome.
Wound preparation is the most important step for adequate evaluation of the wound, prevention of infection, and optimal cosmetic outcome.
![]() Universal precautions and aseptic technique may improve efficiency and cost savings. Full sterile procedures are not required.
Universal precautions and aseptic technique may improve efficiency and cost savings. Full sterile procedures are not required.
![]() Pain control with consideration of local or regional anesthesia should be provided before any wound manipulation.
Pain control with consideration of local or regional anesthesia should be provided before any wound manipulation.
![]() Perform a careful neurovascular examination prior to anesthesia. Two-point discrimination (<6 mm) for digital nerves.
Perform a careful neurovascular examination prior to anesthesia. Two-point discrimination (<6 mm) for digital nerves.
HEMOSTASIS
![]() Direct pressure is the preferred method to control bleeding to facilitate adequate wound evaluation.
Direct pressure is the preferred method to control bleeding to facilitate adequate wound evaluation.
![]() Epinephrine-containing local anesthetics can be used in distal anatomy such as finger, nose, and ear except in patients with underlying small vessel disease.
Epinephrine-containing local anesthetics can be used in distal anatomy such as finger, nose, and ear except in patients with underlying small vessel disease.
![]() Other measures for control of bleeding include ligation of small vessels, electrocautery, absorbable gelatin foam (Gelfoam), oxidized cellulose (Oxycel), or collagen sponge (Actifoam).
Other measures for control of bleeding include ligation of small vessels, electrocautery, absorbable gelatin foam (Gelfoam), oxidized cellulose (Oxycel), or collagen sponge (Actifoam).
IRRIGATION AND CLEANING
![]() Use skin disinfectants only on the wound edges and outward, as these substances may impair host defenses and promote bacterial growth in the wound.
Use skin disinfectants only on the wound edges and outward, as these substances may impair host defenses and promote bacterial growth in the wound.
![]() Wound irrigation reduces infection. Normal saline has lowest toxicity, but tap water is safe and effective.
Wound irrigation reduces infection. Normal saline has lowest toxicity, but tap water is safe and effective.
![]() Low pressure irrigation (0.5 psi-slow gentle wash) for uncontaminated wounds.
Low pressure irrigation (0.5 psi-slow gentle wash) for uncontaminated wounds.
![]() High pressure irrigation (>7 psi-18 g catheter) for contaminated wounds.
High pressure irrigation (>7 psi-18 g catheter) for contaminated wounds.
![]() Use 60 mL per centimeter of wound length, with a minimum of 200 mL.
Use 60 mL per centimeter of wound length, with a minimum of 200 mL.
![]() Soaking wounds is not effective in cleaning contaminated wounds and may increase wound bacterial counts.
Soaking wounds is not effective in cleaning contaminated wounds and may increase wound bacterial counts.
DEBRIDEMENT AND HAIR REMOVAL
![]() Debridement of devitalized tissue by elliptical incision removes foreign matter and bacteria, resulting in a decreased infection risk. It also creates a clean wound edge, facilitating repair.
Debridement of devitalized tissue by elliptical incision removes foreign matter and bacteria, resulting in a decreased infection risk. It also creates a clean wound edge, facilitating repair.
![]() Clip hair if necessary rather than shaving the skin, as shaving is associated with an increased infection rate. Do not remove hair from eyebrows due to the potential for abnormal or lack of regeneration.
Clip hair if necessary rather than shaving the skin, as shaving is associated with an increased infection rate. Do not remove hair from eyebrows due to the potential for abnormal or lack of regeneration.
ANTIBIOTICS
![]() Although there is no clear evidence that antibiotic prophylaxis prevents wound infection in most ED patients, there may be a role in selected high-risk wounds and populations.
Although there is no clear evidence that antibiotic prophylaxis prevents wound infection in most ED patients, there may be a role in selected high-risk wounds and populations.
![]() If used, antibiotic prophylaxis should be: (1) initiated before tissue manipulation, (2) effective against predicted pathogens, and (3) administered by routes that quickly achieve adequate blood levels.
If used, antibiotic prophylaxis should be: (1) initiated before tissue manipulation, (2) effective against predicted pathogens, and (3) administered by routes that quickly achieve adequate blood levels.
![]() For non-bite infections use a first-generation cepha-losporin; cephalexin 25–50 milligrams/kg/day PO qid in children; 500 milligrams PO four times daily in adults. For β-lactam allergic patients use clindamycin 8 to 25 milligrams/kg/day three times daily in children or 150 to 450 four times daily for adults.
For non-bite infections use a first-generation cepha-losporin; cephalexin 25–50 milligrams/kg/day PO qid in children; 500 milligrams PO four times daily in adults. For β-lactam allergic patients use clindamycin 8 to 25 milligrams/kg/day three times daily in children or 150 to 450 four times daily for adults.
![]() Patients with bites should be treated with amoxi-cillin-clavulanate, 875 milligrams PO twice daily (25–50 milligrams/kg/day twice daily for children) to cover Pasteurella, Eikenella, or Capnocytophaga.
Patients with bites should be treated with amoxi-cillin-clavulanate, 875 milligrams PO twice daily (25–50 milligrams/kg/day twice daily for children) to cover Pasteurella, Eikenella, or Capnocytophaga.
![]() Wounds contaminated by fresh water and plantar puncture wounds of the foot require coverage for Pseudomonas, such as ciprofloxacin 500 PO twice daily in adults.
Wounds contaminated by fresh water and plantar puncture wounds of the foot require coverage for Pseudomonas, such as ciprofloxacin 500 PO twice daily in adults.
![]() Prophylactic antibiotics should be given for 3 to 5 days.
Prophylactic antibiotics should be given for 3 to 5 days.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



