223 Evaluating Pediatric Critical Care Practices
 A Historical Perspective on Quality
A Historical Perspective on Quality
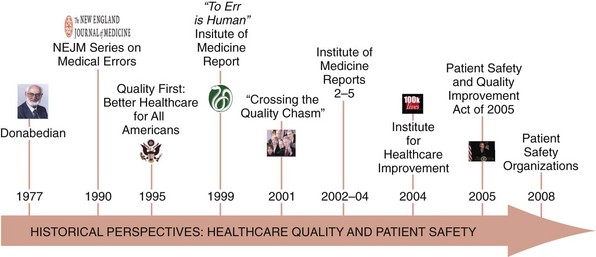
Quality in health care has received increased focus over the last 30 years, beginning with Donabedian’s influence demonstrating that the fundamental concepts of structure, process, and outcome were as important to health care as they were to other industries (Figure 223-1).1 Since then, focused efforts to advance the concept of quality in health care have been performed. In the early 1990s, a series of articles in the New England Journal of Medicine quantified adverse events and helped disentangle the elements of patient harm and its relationship to risk management.2–4 A few years later, President Clinton, through executive order, chartered a commission to investigate healthcare quality more broadly.5
Despite these and a variety of other prominent efforts, discussion regarding quality in health care remained relatively stagnant until the Institute of Medicine’s (IOM’s) series of reports.6–9 The first IOM report, “To Err is Human,” provided a wakeup call for the healthcare industry to consider how patients may be harmed.6 This was followed by “Crossing the Quality Chasm,” which defined six “Aims for Improvement.”7 These aims included safety, effectiveness, equity, timeliness, patient centeredness, and efficiency and helped establish a framework through which clinical services, including those delivered to the critically ill child, could be evaluated.10
The Institute for Healthcare Improvement (IHI), among other groups, became instrumental in providing clinicians with tools to help them focus on improvement work by defining and measuring what was to be improved and by when.11 Efforts aimed at improving reporting and learning from adverse occurrences were noticed when President Bush signed the Patient Safety and Quality Improvement Act, which would become operationalized in part through patient safety organizations.12 More recently, with healthcare reform taking shape, other considerable advances including medical homes, accountable care organizations, and pay for performance are likely to take on additional significance and set the tone for healthcare quality for years to come. This will create important opportunities and challenges for advancing care for critically ill children.10
 Systems of Care
Systems of Care
Traditional engineering approaches focus on how systems work rather than on understanding the ways in which they fail or the effects of failure.13 There are several aspects of system design and maintenance that can affect the likelihood of failure. This is a fundamental distinction to how quality is viewed in health care.13 First, clinicians often approach quality improvement from the perspective of risk rather than the perspective of reliability. Mortality and morbidity conferences, peer review meetings, and root-cause analysis all tend to focus on what went wrong in retrospect and the elements of failure rather than on the system’s reliability.13 Second, pediatric critical care clinicians function in complex systems of care yet have little training or experience in how to design and organize those complex systems to ensure that the needs of the critically ill child are met.13 Routinely, providers will repetitively use “workarounds” rather than redesigning processes to be safer and more efficient. Finally, in contrast to the engineering approach, clinicians are very interested in the effects of system failure, which in clinical parlance are the outcomes of care. Whereas outcomes are important, several recent efforts in health care have also demonstrated the importance of managing the processes of care.14 The best examples of these efforts in pediatric critical care are evidence-based clinical guidelines, checklists, and “bundles” of care, which represent tactical opportunities to specify how care should be delivered to arrive at the desired outcomes.
 Designing for Evaluation
Designing for Evaluation
Program Elements
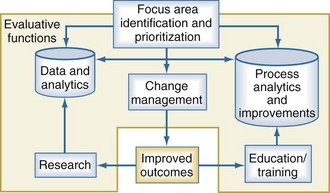
The ability to evaluate clinical services, including pediatric critical care services, depends upon how well the evaluation program is built and implemented. When considering complex systems, it is often helpful to begin by identifying the focus areas for evaluation and improvement and prioritizing those based on the desired impact. Quality improvement and evaluation rely upon three critical and interdependent functions: data and analytics, process improvement techniques, and change management principles (Figure 223-2). Each one of these functions is important in their own right, but none of these is sufficient individually to accomplish successful improvement. The use of data is fundamental for improving quality. Data should be objective, easy to measure, accurate, and establish a baseline of performance upon which improvement efforts can be compared when the evaluation is completed. The analytic component is equally important. Effective programs will move past mere descriptions of data and use important analytic techniques to support their inferences. Clinical processes are the interactions between providers and their patients and providers with one another. A variety of techniques can help with the description of clinical processes, including workflow analysis, flow charting, and time motion studies. These important data elements can then be compared and analyzed using value-stream mapping to eliminate waste and streamline the process, making the care more efficient. More recent efforts evaluating teamwork principles and their impact on outcomes are beginning to emerge.15,16 Change management is fundamental to every improvement process. In addition to managing the changes in process, managing the transition from a current state to some future state requires attention to relationships, commitment, and communication for the team and its members.
Sustaining Improvements
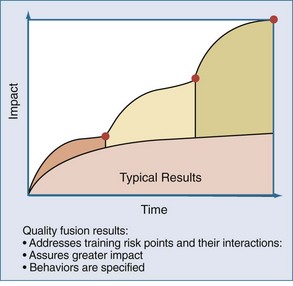
In contrast, when systems are designed around specified behaviors, and the risk points that allow workarounds and adaptive behaviors to emerge are identified, higher levels of performance can be achieved. This approach involves the fusion of different team members’ perspectives over time. For example, when considering the evaluation of results of a recent project to improve bloodstream infections, the PICU team invited members of the operating room suite and hematology-oncology service to participate in the meetings. The input of these “internal consultants” provided the PICU team with an opportunity to learn and apply useful practices from other clinical contexts with relevance to their patient. The use of this so-called quality fusion approach (Figure 223-3) provides the PICU with a greater impact on the initiative under study and provides important sustainability when attention is diverted to the next improvement project.
 Evaluation Domains at the Unit Level
Evaluation Domains at the Unit Level
Safety
Since the IOM’s report on medical errors and patient safety highlighted the problem of iatrogenic injury in hospitalized inpatients, numerous stakeholders have begun to focus on reducing medical errors as a means of improving patient safety and reducing the harm associated with the delivery of health care.7 Adverse patient occurrences are inevitable in the high-risk environment of the PICU, but interventions aimed at reducing these adverse events can be designed once one understands the types of errors and the circumstances that contribute to them.
Error Classification
Different classification schemes for medical errors have been developed. Brennan and colleagues classified adverse events in medical practice as operative and nonoperative.7 McClead and Menke, in their classification system for neonatal ICUs, included both the investigation of complications associated with new or unproven technologies and the study of human error, which is relevant to the understanding of a just culture where providers are held accountable for risky behaviors in the care process.17–18 The identification of critical incidents provides opportunities to make system improvements. Finally, the IOM categorized medical errors based on their diagnosis, treatment, prevention, communication, and equipment failures.6 These categories are relevant for the evaluation of pediatric critical care services.
Diagnostic Errors
The autopsy has been used as a technique to enhance quality assurance programs in medical care. Diagnostic errors uncovered at autopsy that result in the primary cause of death or affected patient outcome are important to consider.19 In three single-institution studies of critically ill adults, autopsies revealed diagnoses that would have changed antemortem management and affected outcome in 10% to 27% of cases.20–22 In children, the rate of missed diagnoses that affected outcome was estimated at 7% in one study.23 In the PICU, one study identified major diagnostic errors that would have affected outcome in 5% of patients; in an additional 25% of cases, there were missed diagnoses that were not believed to be clinically meaningful.24 Importantly, iatrogenic injury was a major subset of these missed diagnoses, occurring 17% of the time.24 Thus, autopsy remains an important tool for identifying diagnostic errors and deaths related to iatrogenic injury in the PICU. It also provides an opportunity to enhance provider education and training related to diagnostic dilemmas.
Treatment Errors
Medication Errors
Medication administration occurs frequently in the treatment of critically ill children and provides considerably more opportunities for medication errors and adverse drug events (ADEs). Among hospitalized children, ADEs are common, and the PICU is an important setting for their occurrence.25–26 Specific medication classes are prone to errors, including sedatives, vasoactive infusions, and parenteral nutrition. One useful and cost-effective strategy to improve medication safety in the PICU is to have a unit-based pharmacist who can intervene to adjust dosages, provide drug information, contribute to management decisions, and monitor complications of medication therapy. This has become an increasingly important opportunity to be able to provide high-quality critical care services to children.27
Nosocomial Infection
Acquired infections are important contributors to morbidity, mortality, and cost in the PICU.14,28–32 Recent efforts have expanded our knowledge of the incidence, prevalence, risk factors, costs, and methods of improving bloodstream infections in the PICU.14 The importance of these efforts is the ability to demonstrate how care can be improved when providers use data to drive system changes.
Risk factors for nosocomial infection in the PICU include severity of illness, postoperative status, and device use.31–34 Specific investigations into the types of nosocomial infection (e.g., urinary tract, pneumonia), specific organisms (e.g., influenza, respiratory syncytial virus, methicillin-resistant Staphylococcus aureus), specific PICU patient populations (e.g., cardiac surgery, burns), and specific procedures (e.g., mechanical ventilation, extracorporeal membrane oxygenation) have been performed. These studies provide insight for the development of directed strategies to reduce nosocomial infection rates and their associated morbidity and mortality in PICUs. These strategies include more stringent infection control policies, reduction of colonization with resistant organisms, and scheduled rotation of prescribed antibiotics.35–37 Perhaps the most important opportunity to reduce infections is the removal of unnecessary devices including urinary catheters, central venous and arterial catheters, and ventilators as soon as they are not longer needed for the child’s care.14,31,32
Procedures
Interventional procedures are an important component of pediatric critical care practice. They provide the intensivist with the means to address a child’s failing organ systems, but they are also associated with risk. Procedural risks are associated with both the insertion and maintenance of these devices. For example, tracheal intubation is associated with potential complications from laryngoscopy, failed intubation attempts, esophageal intubation, damage to the teeth, and hypoxemia.38–39 In addition, the risks from unintended extubation for the child with respiratory failure are significant. PICUs can address their rates of adverse occurrences related to both the performance and maintenance of commonly performed invasive procedures like central venous access, mechanical ventilation, arterial cannulation, and intracranial pressure monitoring. Collaborative efforts that share best-practice methods of inserting and maintaining these devices can demonstrably improve the complications associated with these procedures.14
Preventive Errors
In the ICU, considerable evidence has been accumulated regarding prophylaxis for gastrointestinal stress ulcers, deep venous thrombosis, pressure ulcers, and other adverse events.40–41 Efforts have also been made to address prophylactic care more broadly. For example, the Prophylactic Intravenous Use of Milrinone After Cardiac Operation in Pediatrics (PRIMACORP) study was initiated to determine whether the prophylactic postoperative use of milrinone in pediatric cardiac surgery patients improves the outcome associated with low cardiac output syndrome.42
Other Errors
The PICU environment may itself be an independent contributor to patient safety. Two characteristics contribute to the likelihood of errors in the PICU. The first is complexity, or the degree to which system components are specialized and interdependent. Complex systems are more prone to errors. The second characteristic is coupling. Tightly coupled systems have no buffer, and sequences are fixed, whereas loosely coupled systems can tolerate delays or variations in sequencing. Communication errors, equipment failures, system failures, and more recently, problems with teamwork are all associated with complex and tightly coupled systems and can contribute to an unsafe environment in these settings.6 Equipment failures are an obvious and often unavoidable problem related to patient safety. However, communication failures, system failures, and teamwork problems can enhance the likelihood of errors and prevent an appropriate mitigating response when they occur.15–16
Effectiveness
Evidence-based practice incorporates the best research evidence with clinical expertise and patient values to achieve the best outcomes for patients.7 The clinical practice of critical care medicine is highly variable among practitioners and institutions. Efforts to reduce variability in care are provided by the implementation of practice guidelines and the use of clinical algorithms and checklists.43–44
Private, governmental, and subspecialty organizations have developed numerous guidelines to reduce unnecessary variability in care. The American Academy of Pediatrics and the Society for Critical Care Medicine have developed guidelines and policy statements to help improve the care of critically ill children.45–46 Guidelines can be heterogeneous with respect to their creation. At one extreme, results from randomized controlled trials are incorporated into the care guidelines; at the other extreme, the consensus of a group of practitioners is all that is required. This is important, because the success of any practice guideline is dependent on its ability to influence physician decision making.
Efficiency
Economics demands that healthcare resources be delivered in a cost-effective and efficient manner while not jeopardizing quality.47 The achievement of specific outcome goals is a measure of an ICU’s quality. Costs vary with outcome measures. Mortality rates, efficiency rates, lengths of stay, rates of nosocomial infection and readmission, and the presence of a teaching program all impact expenses and reimbursement. Quality at a given level of cost determines the value of a commodity. In this case, the commodity is ICU care.48
The value of an individual ICU is increased by its ability to achieve selected measures of outcome while keeping costs to a minimum. This is concordant with the concept of efficiency as an aim in the IOM’s current model of healthcare quality.7 Intensive care services are a commodity, and those units providing quality care at a reasonable cost, as judged by efficiency and a similar patient mix, will be most appealing. Less efficient ICUs will have to optimize efficiency or have cost-containment strategies imposed on them.48
From a microeconomic perspective, patients who are sicker require more services in the ICU, stay longer, are more likely to die, and cost more to be treated.49–50 This is not new information. However, to balance the issues of cost and quality, ICUs should identify same-strata best-practices ICUs with similar cost drivers (e.g., severity of illness) and operate under a philosophy of “targeted benchmarking” to achieve comparability up to a specified level.51 To accomplish this, clinical scoring systems are frequently used to control for case-mix variables (physiology, diagnoses, etc.) and thus allow for standardized comparisons. Length of stay has become a standard in benchmarking ICU performance and quality, and reducing length of stay is one method of reducing cost, although as a variable itself, length of stay is subject to differences in measurement.52–53 The standardized length-of-stay ratio is that of observed-to-predicted length of stay and is an indicator of resource use adjusted for severity.54 The standardized length-of-stay ratio can be used to compare a particular unit’s performance over time, but it can also be used to determine whether a particular ICU’s resource use is above or below that of similar ICUs.54
Another method of assessing the efficiency of resource use in the ICU is to evaluate unique ICU therapies55–61—that is, those that are best delivered in the ICU, such as mechanical ventilation and vasoactive infusions. Individual ICUs and physicians differ in their monitoring strategies, so monitoring technologies should not be classified as unique therapies.57 The benefits of this approach are that it allows physicians to determine the proportion of low-risk monitor-only patients61 and compare the number of high-risk critical care patients requiring unique ICU therapies. Excess bed capacity leads to a higher ratio of monitored patients to high-risk patients and reduces the efficiency of the ICU.61 Opportunities to evaluate admission and discharge criteria, as well as throughput issues resulting from the inability to transfer ICU patients because of a high hospital occupancy rate, may serve to improve an individual ICU’s efficiency.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree