CHAPTER 23 ENDPOINTS OF RESUSCITATION
The optimal endpoint of resuscitation has been debated since the early 20th century when Cannon espoused his controversial viewpoints concerning limited volume resuscitation, and it continues to be a topic of tremendous discussion and study. The ideal endpoint should be readily obtainable and easily interpretable. The goal is to provide adequate oxygen delivery (DO2) and therefore tissue perfusion without producing the complications of over-resuscitation. This is accomplished primarily by increasing cardiac output via increases in preload (volume loading) or vasoactive drugs. Multiple diagnostic measurements have been used to determine both optimal cardiac performance and adequate tissue perfusion. While no single value can be used exclusively, various measurements do allow uniformity in comparing adequacy of resuscitation. The values provide the ability over time to determine whether a patient is being properly resuscitated. These can be categorized into hemodynamic parameters, metabolic parameters, and regional perfusion endpoints.
HEMODYNAMIC PARAMETERS
Vital Signs and Clinical Endpoints
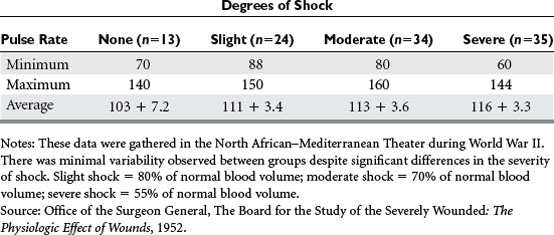
Shock has been defined in a multitude of ways, but can best be described as a lack of adequate tissue perfusion, and thereby an impairment of oxygen delivery and removal of waste products. The six basic advanced trauma life support (ATLS) physiologic parameters that have been used to identify shock are heart rate, respiratory rate, blood pressure, urine output, level of consciousness, and pulse pressure. Urine output and level of consciousness are direct measurements of tissue perfusion, and are defined by the classes of shock. Renal blood flow correlates with arterial pressure, but can be subject to significant autoregulation during periods of hypoperfusion. Level of consciousness is less reliable when influenced by intoxication, central nervous system injury, and medication. Heart rate and respiratory rate can be notoriously misleading (Table 1). Anxiety, pain, and stress secondary to the emotional impact of trauma can falsely elevate these physiologic parameters. This can confuse the picture and mask the underlying severity of shock. The diagnosis of shock is best made by observing the body’s main compensatory mechanism: redistribution of blood flow.
Invasive Monitoring
Many have attempted to define the oxygen consumption/delivery endpoint itself, but with no clear results. The Fick equation states that DO2 and VO2 are functions of cardiac performance (CI), hemoglobin (Hb), and arterial and venous oxygen saturations (SaO2 and SvO2, respectively):
Unfortunately, DO2 and VO2 are both derived from cardiac output, and the stable plateau described in Figure 1 is virtually impossible to obtain. Goal-directed therapy, aimed at ensuring CI greater than 4.5 l/min/m2, DO2 index greater than 600 ml/min/m2, and VO2 index greater than 170 ml/min/m2, has been advocated by Shoemaker and others, showing reduced morbidity and mortality in critically ill patients. However, Gattinoni in a multicenter randomized controlled trial, and Heyland in a meta-analysis, have shown that no such benefit exists. Furthermore, a prospective, randomized controlled trial by Velmahos comparing conventional versus supranormal endpoints demonstrated that despite all efforts, only 70% of patients were able to reach these endpoints. They concluded that regardless of the resuscitation strategy, the ability of the patient to achieve “optimal hemodynamic values” significantly affected outcome. Looking at O2 delivery alone, McKinley et al. found that there was no difference in outcome between groups resuscitated to an O2 delivery goal of 600 ml/min/m2 versus 500 ml/min/m2.
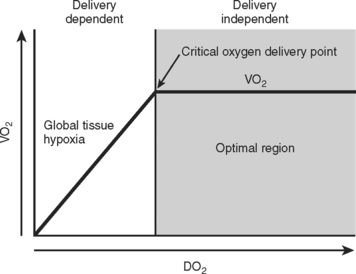
Figure 1 Relationship between oxygen delivery (DO2) and oxygen extraction (VO2).
(From Bilkovski RN, et al: Targeted resuscitation strategies after injury. Curr Opin Crit Care 10:529–538, 2004, with permission.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree