Endocrine Function
An understanding of the pathophysiology of endocrine function is important in the management of anesthesia for patients with disorders of the hormone-producing glands (Schwartz JJ, Akhtar S, Rosenbaum SH. Endocrine function. In: Barash PG, Cullen BF, Stoelting RK, Cahalan MK, Ortega R, Stock MC, eds. Clinical Anesthesia. Philadelphia: Lippincott Williams & Wilkins; 2013:1326–1355).
I. Thyroid Gland
Thyroid Metabolism and Function. Thyroxine (T4) and triiodothyronine (T3) are the major regulators of cellular metabolic activity. The thyroid gland is solely responsible for the daily secretion of T4 (80–100 μg/day; elimination half-time, 6–7 days). About 80% of T3 is produced by extrathyroidal deiodination of T4 (elimination half-time, 24–30 hours). Thyroid hormone synthesis occurs in four stages (Fig. 46-1). Most of the excess effects of thyroid hormones (hyperadrenergic state) are mediated by T3 (Table 46-1).
Tests of Thyroid Function (Table 46-2)
Hyperthyroidism
Treatment and Anesthetic Considerations (Table 46-3)
A combination of propranolol (effective in attenuating the manifestations of excessive sympathetic nervous system activity, as evidenced by a heart rate <90 beats/min) and potassium iodide (inhibits hormone release) is effective in rendering patients “euthyroid” before anesthesia and surgery. Esmolol may be administered as a continuous intravenous (IV) infusion to maintain the heart rate below 90 beats/min.
The goal of intraoperative management is achievement of a depth of anesthesia (often with isoflurane or desflurane) that prevents an exaggerated sympathetic nervous system response to surgical stimulation. Drugs that activate the sympathetic nervous system (ketamine) or increase the heart rate (pancuronium) are not likely to be recommended.
If a regional anesthetic is selected, epinephrine should not be added to the local anesthetic solution.
Anesthesia for thyroid surgery (subtotal thyroidectomy) is an alternative to prolonged medical therapy. Complications associated with surgery occur more frequently when preoperative preparation is inadequate (Tables 46-4 and 46-5).
It is useful to evaluate vocal cord function in the early postoperative period by asking patients to say the letter “e.”
Unexpected difficult intubation is increased in the presence of goiter. Inhalation induction or awake fiberoptic intubation should be considered if there is evidence of significant airway obstruction or tracheal deviation or narrowing.
Postoperative airway obstruction caused by hematoma or tracheomalacia may require urgent reintubation of the trachea.
Operating on an acutely hyperthyroid patient may provoke thyroid storm.
Hypothyroidism
Hypothyroidism is a relatively common disease (0.5%–0.8% of the adult population) that results from inadequate circulating levels of T4, T3, or both (Table 46-6).
Treatment and Anesthetic Considerations
No evidence supports postponement of elective surgery (including coronary artery bypass graft surgery) in the presence of mild to moderate hypothyroidism.
No evidence supports the choice of a specific anesthetic technique or selection of drugs for hypothyroid patients, although opioids and volatile anesthetics are often considered to have increased depressant effects in these patients. There appears to be little, if any, decrease in anesthetic requirements as reflected by the minimum alveolar concentration.
Meticulous attention must be paid to maintaining body temperature.
Myxedema coma is a medical emergency that requires aggressive therapy (Table 46-7).
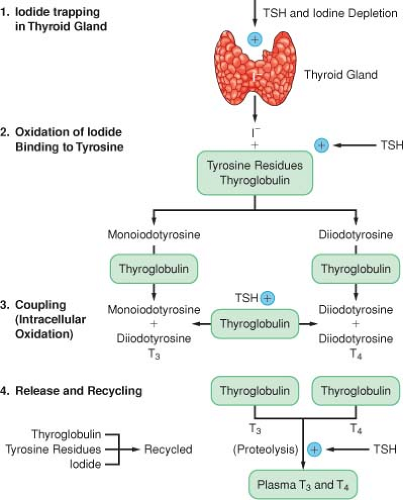 Figure 46-1. Schematic depiction of the four stages of synthesis and release of thyroid hormone. T3 = triiodothyronine; T4 = thyroxine; TSH = thyroid-stimulating hormone. |
Table 46-1 Effects of Triiodothyronine on Receptor Concentrations | |
|---|---|
|
Table 46-2 Tests of Thyroid Function | ||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Table 46-3 Preparation of Hyperthyroid Patients | ||
|---|---|---|
|
Table 46-4 Possible Complications of Thyroid Surgery | ||
|---|---|---|
|
Table 46-5 Management of Thyroid Storm | ||
|---|---|---|
|
Table 46-6 Manifestations of Hypothyroidism | ||
|---|---|---|
|
II. Parathyroid Glands
Calcium Physiology. Parathyroid hormone secretion is regulated by the serum ionized calcium concentration (negative feedback mechanism) to maintain calcium levels in a normal range (8.8–10.4 mg/dL).
Hyperparathyroidism
Hypercalcemia is responsible for a broad spectrum of signs and symptoms (nephrolithiasis, confusion).
Treatment and Anesthetic Considerations. Preoperative IV administration of normal saline and furosemide may lower serum calcium concentrations. There is no evidence that a specific anesthetic drug or technique is preferred. A cautious approach to the use of muscle relaxants is suggested by the unpredictable effect of hypercalcemia at the neuromuscular junction. Careful positioning of osteopenic patients during surgery is necessary to minimize the likelihood of pathologic bone fractures.
Anesthesia for Parathyroid Surgery. General anesthesia is most commonly selected. Minimally invasive parathyroidectomy is superior to conventional bilateral cervical exploration and can usually be performed using a bilateral cervical plexus block.
Hypoparathyroidism. Clinical features are manifestations of hypocalcemia, and treatment is with calcium gluconate (10–20 mL of 10% solution IV) (Table 46-8).
Table 46-7 Management of Myxedema Coma | ||
|---|---|---|
|
III. Adrenal Cortex
The biologic effects of adrenal cortex dysfunction reflect cortisol or aldosterone excess or deficiency (Table 46-9).
Glucocorticoid Excess (Cushing Syndrome) (Table 46-10)
The diagnosis of hyperadrenocorticism is established by failure of the exogenous administration of dexamethasone to suppress endogenous cortisol secretion.
Anesthetic Management (Table 46-11). Etomidate has been used for temporizing medical treatment of severe Cushing’s disease because of its inhibition of steroid synthesis.
Mineralocorticoid excess should be considered in nonedematous hypertensive patients who have persistent hypokalemia and are not receiving potassium-wasting diuretics.
Adrenal Insufficiency (Addison Disease)
Clinically, primary adrenal insufficiency is usually not apparent until at least 90% of the adrenal cortex has been destroyed.
The clinical presentation almost always includes hypotension. (A high degree of suspicion should be maintained for patients who demonstrate cardiovascular instability without a defined cause.)
Treatment and Anesthetic Considerations. Immediate therapy consists of electrolyte resuscitation (glucose in
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








