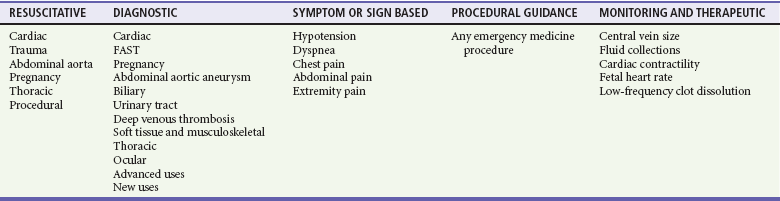
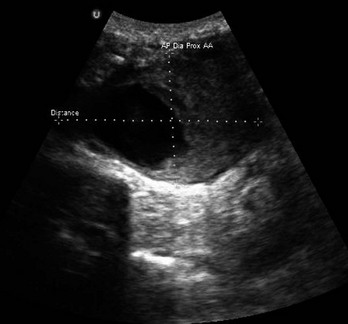
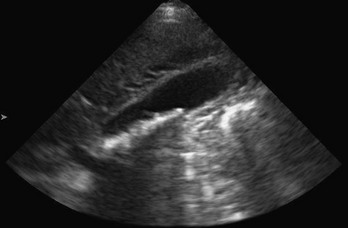
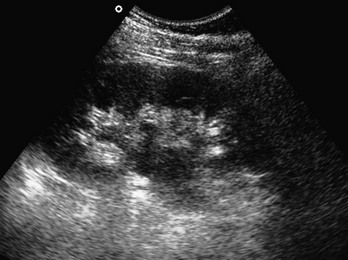
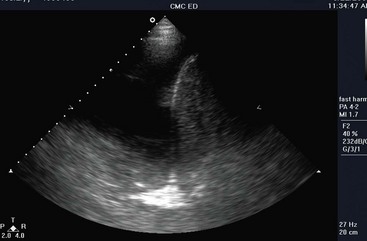
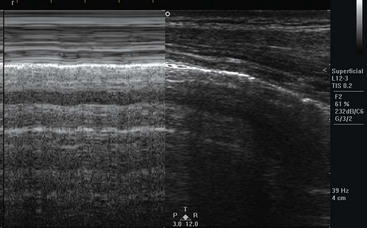
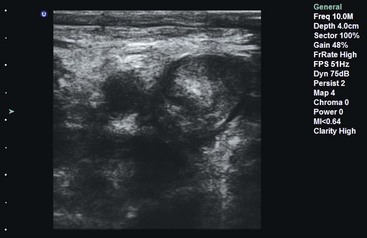
Chapter 196 Emergency ultrasound (US) is the simultaneous performance and interpretation of a focused sonographic examination at the bedside of the patient for the diagnosis, resuscitation, monitoring, guidance, and treatment of emergency medical conditions.1,2 Emergency US is an emergency clinician–performed study.1,3 Although the operator is typically an emergency physician, he or she may be an emergency physician assistant, nurse practitioner, or trained emergency nurse or paramedic—all under the supervision of a trained, credentialed emergency physician.4–6 Emergency physicians who have advanced training in US imaging are also known as emergency sonologists.6 Emergency US is typically performed in the emergency department (ED) but may also be performed in other areas of the hospital, emergency stand-alone centers, out-of-hospital mobile transport (such as ambulances and helicopters), disaster scenes, military engagements, international rescue work, and remote settings (such as space, sea, or land centers with limited or no medical access).7–13 With emergency US, the physician or clinician (1) performs, (2) simultaneously interprets the examination, and (3) integrates the results in the clinical scenario.1,5 This is unlike other specialties, in which a trained technologist performs the examination and a physician interprets or “reads” the images.5,14 Emergency US examinations are focused examinations of an area of the body, organ system, or physiologic pattern or goal-directed investigations of an emergency symptom or sign. Not all pathologic processes will be detected by such examinations, usually because of the interference of acoustic entities that reduce transmission and reflection of sound and the lack of an appropriate window to the tissue of choice. Other limitations include experience, skill, and confidence of the performing physician.15 The main risk management issue associated with emergency US is not using the modality when it is available and appropriate.16 A half-century of scientific work in many countries produced the initial medical uses of US in the 1950s by physicians interested in its advantages over traditional imaging, including noninvasiveness, lack of ionizing radiation, and superior resolution.14 In the 1980s emergency physicians started to use US as a way of ruling out emergent “silent” diagnoses, such as ectopic pregnancy, intraperitoneal hemorrhage, hemopericardium, cholelithiasis, renal colic, and aortic aneurysm. A model curriculum was created by the Society for Academic Emergency Medicine (SAEM) that initiated formal guidance for emergency US programs.17,18 Because of resistance from traditional imaging specialties, such as radiology and cardiology, the American Medical Association House of Delegates, led by the American College of Emergency Physicians (ACEP), passed a resolution that hospital credentialing committees follow specialty-specific guidelines for US-based credentialing.19 Specialty-specific guidelines, created in 2001 and updated in 2008 by the ACEP and endorsed by the SAEM in 2010, specify emergency US scope of practice, primary applications, training pathways, number of procedures required for training before credentialing, quality assurance and documentation guidance, and training course outlines.1 Today, more than 95% of emergency medicine residencies teach US, and approximately 30 to 60% of community hospitals have instituted bedside US performed by emergency physicians.20,21 Since 2008, emergency US has been recognized by outside organizations, including the American Institute of Ultrasound in Medicine, with implementation of the focused assessment with sonography for trauma (FAST) examination, and the American Society of Echocardiography, with application of focused cardiac US (FOCUS) for shock, effusion, chest pain, and cardiac arrest.22,23 Several other organizations have recognized emergency or point-of-care US, including the World Interactive Network Focused on Critical Ultrasound internationally and the Society of Medical Ultrasound in Medical Education for medical education. US programs typically require some investment in education and hardware, but reimbursement for both professional and hospital fees is adequate to meet return on investment within years, depending on number and types of US, payer mix, and documentation.24 More EDs have recently invested in digital-based archiving and storage systems. The more traditional solution is the picture archiving and communication system. A new, more comprehensive solution seems to be the web-based US management systems, which provide archiving, documentation, quality assurance, and credential solutions to the emergency medicine and point-of-care market. Emergency US is one of the competency assessments required of emergency medicine residents by the Residency Review Committee for Emergency Medicine, with defined requirements as set by national organizations.25–27 For emergency physicians in practice, initial training often takes place through nationally defined hands-on continuing medical education courses followed by a period of proctoring or supervision.1,28 Credentialing at the hospital level is based on specialty-specific national guidelines. Recent educational advances, such as simulation, task trainers, and web-based training, enhance US training.29–32 US is not defined as advanced imaging by the Centers for Medicare and Medicaid Services or the 2008 Medicare Improvements for Patients and Providers Act.33 Medical student emergency US education has also been defined by national organizations and may be incorporated in more extensive undergraduate US programs.1 US fellowships have become the most prevalent postgraduate emergency medicine fellowship.34 See the website of the American College of Emergency Physicians (http://www.acep.org/Clinical–Practice-Management/Ultrasound/; accessed April 12, 2013) for helpful references for program development and education. By definition, US is sound with frequencies higher than 20,000 Hz. US is kinetic energy, a longitudinal, mechanical, and directional wave, so all users of this technology should observe the ALARA (as low as reasonably achievable) principle by performing procedures only when they are needed and limiting the time of sonographic investigation.35 Other US terms and artifacts commonly used are listed in Box 196-1. US biosafety, including use of the ALARA principle, appropriate Doppler technology, and appropriate microbiologic disinfection of the probe, has been reinforced by recent articles.36 The ALARA principle suggests that the least amount of energy be used to produce satisfactory imaging. Doppler modes should be minimized over sensitive tissue, including early gestation, germinal tissue, and mucosal or neural tissue. The sonographer should be familiar with the thermal index (TI), which should be kept below 2.0, and the mechanical index (MI), which should be kept below 1.9. Surface probes should be cleaned at the bedside with mechanical removal of the gels and debris and then disinfected with an appropriate spray or wipe. Endocavitary probes will need more prolonged and substantial cleaning. Safety also includes the use of appropriate barriers over transducers, including condoms, gloves, or commercial barriers over endocavitary probes and sterile transducer covers for sterile procedures.37 For nonsterile procedures, barriers can include translucent sterile transdermal barriers. In 1994 the SAEM categorized US applications broadly into abdominal, cardiac, obstetric-gynecologic, and special applications.17 In 2001 the ACEP developed guidelines that categorized applications more specifically to include trauma, pregnancy, abdominal aortic aneurysm, cardiac (for pericardial effusion and cardiac activity), biliary, renal, and procedural guidance.38 In 2008 the ACEP added deep venous thrombosis (DVT), thoracic studies for pneumothorax and pleural effusion, soft tissue and musculoskeletal studies, and ocular examination as core appplications.1 Advanced applications at that time included testicular, adnexal, bowel, advanced echocardiography, transesophageal echocardiography, transcranial Doppler, and contrast studies. Therapeutic applications of transcranial Doppler are being studied by emergency physicians.39 Grouping of these US applications into categories of resuscitative, diagnostic, symptom or sign based, procedural guidance, and monitoring and therapeutic helps describe the relationship between the uses of US in emergency medicine (Table 196-1). The most common uses of emergency US in decreasing order are trauma, cardiac (cardiac arrest and pericardial effusion), abdominal aortic aneurysm, pelvic, biliary, procedural, renal, and DVT.21 Among recent emergency medicine residency graduates, US use was high (98%), with those in academic centers reporting highest use. US guidance can assist many percutaneous procedures, such as vascular access, torso cavities evacuation (e.g., thoracentesis, paracentesis, and pericardiocentesis), arthrocentesis, lumbar puncture, abscess drainage, nerve blocks, and others.3 Emergency US is used in clinical pathways or algorithms to identify or to exclude emergency medical conditions rapidly.40,41 The trauma US examination is also called the focused assessment with sonography for trauma (FAST) examination.1,22,42 The trauma examination originally focused on the peritoneal space, as an evaluation for hemoperitoneum, with use of the right flank, left flank, and pelvic windows for detection of dependent peritoneal fluid and pleural effusion.43 Newer versions include the EFAST (extended FAST) for the evaluation of potential pneumothorax and FASTER for evaluation of the extremities.40,44–46 The FAST examination is based on the premise that a treating physician can sample known sonographic windows within minutes to evaluate the peritoneal, pericardial, and pleural spaces for fluid and abnormal fluid and air. Within the peritoneum, fluid circulates throughout the abdomen and pelvis and settles in dependent spaces.47,48 The volume of fluid required for a positive US study depends on the site of injury and site of sonographic detection, but 250 mL or more is generally visible, and nearly 600 mL of fluid is necessary to cause a positive flank stripe when fluid is infused from the pelvis.49 Pericardial fluid is contained within the parietal and visceral pericardium. Once a certain volume is reached, the pressure in the pericardial space increases exponentially, causing pericardial tamponade.50 In general, 50 mL is required to cause hemodynamic compromise in a patient without prior pericardial inflammation. However, tears in the pericardium that communicate with the pleural space or even the peritoneum can cause false-negative examination findings. Pleural fluid can be detected by US, but this depends on the position of the body.51 Pneumothorax detection is based on the absence of the normal sonographic sliding of the visceral and parietal pleurae, although there are other signs (see thoracic section). The torso trauma US examination (often called the EFAST) can detect pathologic free intraperitoneal fluid (typically hemoperitoneum, uroperitoneum, bile, or ascites), hemopericardium, hemothorax, or pneumothorax.45,46 Typically, fluid in the peritoneum, pericardium, and pleural cavity is anechoic, but it can have echogenicity with clotting, depending on the age of the clot or bowel contents. Compared with other fluid-filled structures in the abdomen and pelvis, peritoneal free fluid generally has sharp edges and an irregular shape, whereas most visceral or vascular structures have intrinsically smooth oval contours and less abrupt edge detail. The FAST technique uses a low- to middle-frequency probe (2-5 MHz) to evaluate dependent peritoneal spaces, pleural spaces, and the pericardium. Within the peritoneum, dependent spaces include the following, grouped by tissue window: the right flank, which evaluates the hepatorenal space (also called Morison’s pouch; Fig. 196-1), the right subphrenic space, and the right costophrenic angle; the left flank, which evaluates the perisplenic space between the diaphragm and spleen, the splenorenal space, the perirenal space, and the left subphrenic space; and the suprapubic view, which is performed by placement of the transducer superior to the pubic bone with a full bladder to visualize the pouch of Douglas in women and the retrovesical space in men. Extra views include the paracolic gutters inferior from the flank views and medial from the iliac spine to visualize free fluid surrounding the bowel.52 For pleural fluid, the superiorly angled flank views allow visualization of the costophrenic angles. The evaluation for pneumothorax uses either a low-frequency probe at a shallow depth or, more typically, a high-frequency probe for better resolution, placed at the anterior chest in the second intercostal space for anterior pneumothorax and at the axilla for large pneumothoraces and pleural effusion. Diaphragm injuries have been described with dislocation of typical organ patterns.53 The sensitivity of the FAST examination ranges from 60 to 99%, and its specificity ranges from 80 to 99%.54–57 The large range of sensitivity is related to the comparative “gold standard” used for each study, with clinical endpoints suggesting higher accuracy. The FAST does not capture every peritoneal injury, although the need for intervention in undetected injuries has not been studied.58 Randomized, controlled trials show lower morbidity, time to operating room, and charges for patients with US use during resuscitation, and a positive US study increases the odds ratio for laparotomy.59,60 Patients with traumatic pericardial effusions are taken to the operating room sooner and have lower mortality rates with US.44 However, the mediastinal injuries more common in blunt trauma have not been assessed without transesophageal echocardiography.50,61 US can diagnose pneumothorax with excellent sensitivity and specificity compared with plain chest radiography and variable accuracy compared with computed tomography scanning.62,63 There are certain populations of patients in whom FAST evaluation has limited benefit. With penetrating chest injuries, the FAST examination seems to be efficacious for both pericardial and nearby peritoneal injuries; but in patients with purely anterior penetrating trauma to the abdomen, the sensitivity of trauma US is poor because bowel injuries can occur without significant hemoperitoneum.58,59,64–66 The accuracy of the FAST examination may be lower in children than in adults, and many pediatric injuries can be observed or treated nonoperatively with angiography.67 In obstetric patients, the few observational studies that have been performed have shown reasonable sensitivity and specificity, although abruption and fetal viability may necessitate an earlier operative course.68 With pelvic fractures, the sensitivity ranges from 20 to 80%.69–72 More important, the detection of free fluid in an unstable patient with a pelvic fracture may be due to uroperitoneum from bladder injury rather than hemoperitoneum from vascular injury, clouding the decision for laparotomy versus pelvic embolization.64 In addition, retroperitoneal injuries to the genitourinary tract are not assessed with four-quadrant FAST examination. Pelvic US by emergency physicians was initiated to address one of the epidemics of the modern era—ectopic pregnancy.73–77 Typically, pelvic US is used to confirm intrauterine pregnancy, which indirectly excludes ectopic pregnancy in most patients.78,79 A recent meta-analysis revealed a pooled sensitivity of 99.3% to rule out ectopic pregnancy when an intrauterine pregnancy was detected. Another use during pregnancy is the detection of fetal viability, incomplete abortion, ectopic pregnancy, and molar pregnancy. Pelvic US is used in nonpregnancy states to detect tubo-ovarian abscesses, masses, and hemoperitoneum in the hemodynamically unstable patient.80 Indications for sonographic evaluation of the first-trimester pregnant patient include symptoms or signs that suggest an ectopic pregnancy, molar pregnancy, or fetal demise and dating of the pregnancy. Intrauterine pregnancy is confirmed with a gestational sac with a yolk sac or fetal pole within the fundus of the uterus (Fig. 196-2).78 An embryonic or fetal demise has US findings of a fetal pole measuring more than 5 mm without fetal heart rate or a gestational sac of more than 20 mm in diameter without a fetal pole. A molar pregnancy appears as an echogenic, cystic uterus with disorganized echoes and is associated with high β-human chorionic gonadotropin concentrations without the sonographic finding of intrauterine pregnancy. Findings of an ectopic pregnancy include a chorionic ring or gestational sac with evidence of a yolk sac or fetal pole outside the uterus or in an abnormal location in the uterus, such as the cornu or cervix.73 Excluding the groups of intrauterine pregnancy, embryonic demise, molar pregnancy, and ectopic pregnancy, there is a class called indeterminate, which may account for 20% of pregnant patients presenting to the ED in the first and early second trimesters. Heterotopic pregnancies can occur at a rate of 1/5000 and be detected by the same techniques and definitions.81 Emergency physician–performed pelvic US has reduced the morbidity of ectopic pregnancy by shortening the time to diagnosis and operating room treatment and has resulted in greater initial detection of abnormal pregnancy, reduced ED patient throughput times, and increased patient satisfaction with care.74,76,82–85 The detection of live intrauterine pregnancy predicts a rate of 91% continuation past 20 weeks, except for those with vaginal bleeding, who drop to a rate of 86%.86 Further continuation of the pregnancy to term occurs in 77% of patients.87 Emergency physicians can date pregnancies accurately by pelvic US with typical fetal biometry.88 Emergency physicians are adept at identification of ectopic pregnancies by both transabdominal and endovaginal techniques.85,89–93 In addition, molar pregnancies and some malformation, such as conjoint twins, have been described.94,95 The gynecologic differential diagnosis of significant free fluid in a pregnant woman, in addition to ectopic pregnancy, should include uterine rupture and ruptured corpus luteum pregnancy.96 Pelvic US in nonpregnancy states has shown good accuracy for tubo-ovarian abscess and improved decision-making for female patients with right lower abdominal pain.97,98 The use of cardiac US by emergency physicians is presentation and symptom specific and focused in nature. Indications include cardiac arrest, possible pericardial effusion, trauma, chest pain, hypotension, and procedural guidance.1,3,23,99 Cardiac US is often included in algorithms and protocols for certain symptoms or signs, such as dyspnea or hypotension. Cardiac US is performed through the transthoracic and transabdominal windows with use of small curvilinear or phased array transducers. Typical views include the subcostal four-chamber and long-axis views, parasternal long-axis view, parasternal short-axis view, and apical four-chamber view. Although most emergency physicians are comfortable with the subcostal view from the FAST examination, the parasternal long-axis view is a good alternative and good window for left ventricular assessment.100,101 In addition, the apical four-chamber view provides excellent comparison of the right and left ventricles in terms of size and function. The long-axis subcostal view shows some of the right side of the heart but highlights the IVC, including size and respiratory variation. Cardiac US performed by emergency physicians shows good accuracy in detection of pericardial effusion (Fig. 196-3), assessment of left ventricular function, and evaluation of patients with undifferentiated shock. In addition, aspects of cardiac US are being used for the assessment of intravascular volume status and cardiac output and in the evaluation of dyspnea. In cardiac arrest, US can detect ventricular motion in both asystole and pulseless electrical activity (PEA).102,103 In asystole, two studies have shown poor prognosis in the absence of sonographic ventricular activity.84 Cardiac US can detect pseudoasystole by revealing ventricular fibrillation or coordinated cardiac contractions without a palpable pulse.85,104 Use of cardiac US in PEA and near-PEA states can be diagnostic for pericardial effusion.82 Cardiac US can detect ventricular capture when the patient is paced, transcutaneously or by a transvenous pacer. US can also identify pneumothorax, another treatable cause of cardiac arrest.103 Cardiac US is feasible during pulse checks and prehospital life support, as advanced cardiac life support guidelines suggest minimizing non–cardiopulmonary resuscitation intervals.105–108 Emergency cardiac US is diagnostic for both medical and traumatic pericardial effusions.109,110 In patients with dyspnea, pericardial effusion is detected with excellent accuracy.111 In trauma, use of cardiac US reduces time to operative intervention and reduces mortality in patients with penetrating cardiac injury.50 Detection of effusions in blunt trauma has also been described. Patients with cardiac US performed by emergency physicians for pericardial effusion have significantly reduced hospital length of stay and charges.112 Cardiac US is used for detection of pericardial effusions, chamber enlargement, and global activity in chest pain syndromes.113 In chest pain, US has been studied for the evaluation of pericardial tamponade, pulmonary embolus, cardiogenic shock, aortic dissection, pneumothorax, and bony chest wall fracture.114–116 US protocols have been developed to evaluate undifferentiated hypotension.41,117–119 Cardiac US windows with the addition of abdominal views can assess for effusion, global ventricular activity, ventricular chamber size, IVC size and respiratory change, peritoneal fluid, and abdominal aortic aneurysm to narrow the differential diagnosis. Sepsis is the most common diagnosis for patients with hyperdynamic ventricular activity.120 Central pressures can be estimated by examination of the IVC size and collapsibility.121,122 Studies show that this technique has good accuracy in assessment of blood loss, hypovolemia, and congestive heart failure.123,124 Correlation studies have shown moderate agreement between central venous pressure and IVC measurements, with actual cardiac qualitative assessment as good as or better than the IVC measurements.125–129 The internal jugular vein measurement may correlate with central venous pressure,130 and esophageal Doppler examination may also correlate with hemodynamic measurements.131 Emergency physicians use abdominal US to detect abdominal aortic aneurysm, another silent disease in patients with flank, abdominal, or back pain, and to evaluate unexplained hypotension in the older patient.132,133 The use of US to detect aortic dissection and occlusion is described as well.134–136 The technique involves imaging of the aorta from the subxiphoid space to the umbilicus to evaluate for dilation above a diameter of 3 cm (Fig. 196-4). For the detection of infrarenal aneurysms, the technique should visualize the aorta from the diaphragm to the aortic bifurcation. Fusiform aneurysms are more common, but detection of saccular aneurysms requires both the transverse and longitudinal planes.137 If an aneurysm is found, a peritoneal view of Morison’s pouch is performed to detect intraperitoneal fluid. Proximal iliac arteries may be followed if it is technically feasible or time allows. Emergency physician use of US for abdominal aortic aneurysm detection has shown good accuracy compared with other imaging modalities and laparotomy.133,138–140 It also has management implications in older patients with lower back pain, in whom the elimination of the presence of abdominal aortic aneurysm can lead to other management decisions. Screening for abdominal aortic aneurysm in the ED with US has been shown to be effective.141,142 Endovascular repair versus the more traditional open repair has become more popular.143,144 The detection of leaks (often called endoleaks) from the stent would require Doppler imaging and may require further imaging with computed tomography or magnetic resonance imaging.144 Aortic dissection may be detected by a combination of abdominal and cardiac scanning.136 A linear echogenic flap, anywhere across the lumen of the aorta, is suggestive of dissection, sometimes with the detection of different flows on either side of the flap by color Doppler scanning. The cardiac US examination can show unexplained pericardial effusion; a dilated aortic root; aortic insufficiency; and a linear echogenic flap seen in the ascending aorta, aortic arch (through a suprasternal notch), or descending aorta. Aortic occlusion is another condition that may be detected by US.145 Echogenic thrombus may fill the aorta and disrupt perfusion below the diaphragm with resulting pain, pallor, numbness, and reduction or absence of distal pulses. Clear identification of the borders and lack of Doppler flow in the abdominal aorta are characteristic of the syndrome. Biliary US to detect gallstones and associated cholecystitis was one of the early applications of US in emergency medicine.146–148 The sonographic technique involves a modified biplanar approach to the right upper quadrant. A complete evaluation includes visualization of the common bile duct. The diagnosis of cholelithiasis is made after identification of echogenic foci within the gallbladder lumen with shadowing (Fig. 196-5). Other image patterns include stones that will not shadow, sludge, and the wall echo sign of a gallbladder full of gallstones. Signs of cholecystitis include a dilated gallbladder, increased gallbladder wall thickness, sonographic Murphy’s sign, and pericholecystic fluid. A nonmobile stone in the gallbladder neck is highly suggestive of eventual cholecystitis.149 A common bile duct larger than 6 mm in people younger than 60 years and smaller than 10 mm in elders may indicate choledocholithiasis. Biliary US is fast and accurate, with a sensitivity of 87 to 94% and a specificity of 82 to 96% in detection of gallstones, comparable to radiology ultrasonography.150–153 Biliary US has replaced nuclear medicine testing.148,154 Renal US includes biplanar views of the kidneys with emphasis on dilation of the calyceal system and pelvis of the respective kidney (Fig. 196-6). In addition, visualization of the bladder can diagnose secondary hydronephrosis from an obstructed bladder stone and may demonstrate nonobstructive bladder jets through the use of Doppler US. The windows for the two kidneys are similar to those of the trauma flank series, with the exception that the patient may be rolled on the opposite side so that the transducer may be placed more posteriorly on the back if necessary. The bladder view is performed suprapubically, and calculations of volume may be made with on-machine calculators or by formulas. Renal US has a sensitivity of 83% and a specificity of 92% in detection of hydronephrosis (see Fig. 196-6).155,156 Genitourinary tract obstruction protocols have great sensitivity in elimination of renal obstruction from a differential diagnosis.157 Bladder US is useful for detection of a full bladder and the presence of a Foley catheter and for guidance during suprapubic aspiration or Foley placement.119–124,158–160 The swollen extremity often requires sonographic imaging to assess for DVT. Emergency physicians commonly use compression US to rule out DVT.125–128,161–165 The two-level compression technique involves visualization of the compressibility of the common femoral and popliteal veins. The three-level technique adds the junction of the superficial femoral and deep femoral veins (Fig. 196-7). Use of upper extremity veins is less common because Doppler US is needed for the subclavian vein, which is not compressible under the clavicle.166 Figure 196-7 Deep venous thrombosis with layering clot in popliteal vein seen on compression ultrasound examination. The accuracy of this technique ranges from 70 to 99%, depending on operator experience.164,167–169 Hospital charges and time in the ED are reduced for patients who have bedside venous US performed to rule out DVT.170–172 Bernardi also investigated a whole-leg strategy versus a 2-point strategy in combination with a D-dimer test, which required 1-week follow-up with an abnormal level.173 Both strategies were equivalent in detection of symptomatic DVT at 3-month follow-up. Depending on the skill of the sonographer, patient characteristics, and availability of follow-up, ED US may guide lower extremity DVT institutional protocols. Thoracic applications include the detection of pleural effusion, pneumothorax, pneumonia, and interstitial edema.174,175 The technique of thoracic US uses a low-frequency probe to survey for pleural effusions and a high-frequency probe to detect pleural lines and related artifacts. Pleural fluid appears as an anechoic collection above the diaphragm (Fig. 196-8). In addition, a collapsed lung may be visualized as an echogenic floating structure. Normally, the parietal and visceral pleural lines slide against each other, and lack of sliding is the finding most consistent with pneumothorax (on M-mode, called the seashore sign). Additional findings of pneumothorax include the presence of horizontal artifacts called A-lines (on M-mode, called the stratosphere sign) and the absence of B-lines (vertical white lines from reverberation of air with fluid) at the parietal-visceral pleural line (Fig. 196-9).176–179 Confounding factors include adhesions of the pleura, chronic obstructive pulmonary disease, prior pneumothorax, and mainstem bronchus intubation. A lung point sign is the edge of the pneumothorax where the lung is still adherent to the parietal pleura, and part of the image shows no sliding until the lung moves into the interspace with respirations.177 The accuracy of US for detection of pneumothorax (sensitivity 100%, specificity 98%) is better than that of plain chest radiography in the acute setting, but there may be reduced accuracy after 24 hours.180 Severe pneumonia is visualized as echogenic “liver-like” echogenicity as the lung accumulates fluid with consolidation.181 Peripneumonic collections are common and may indicate inflammation. The dynamic air bronchogram, hyperechoic areas within bronchi that move with respiration, usually within “heparinized” lung, has been described as another sign of alveolar consolidation.182 Pulmonary edema is indicated by the presence of comet tails (B-lines), which are reverberation artifacts that reflect from the parietal pleural interface into the lung. Normally found in dependent areas of the lung, the widespread distribution of these artifacts in an apical lung may indicate increased lung congestion.183–185 Dynamic tracheal US for the confirmation of endotracheal intubation has relatively good sensitivity and specificity.186–188 The dynamic movement of the endotracheal tube creates a flutter through the recognized shadow of the airway, but static US seems to lack accuracy.189,190 This technique may have a role in patients in cardiac arrest or with equivocal end-tidal carbon dioxide levels, and confirmation is significantly faster than with chest radiography in children.190
Emergency Ultrasound
Perspective and Definitions
History
Training, Credentialing, and Accreditation
Applied Ultrasound Physics and Instrumentation
Equipment and Safety
Applications and Categorization
Trauma Ultrasound
Pelvic Ultrasound
Cardiac Ultrasound
Abdominal Vascular Ultrasound
Biliary Ultrasound
Urinary Tract Ultrasound
Deep Venous Thrombosis Ultrasound
Thoracic and Tracheal Ultrasound
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree