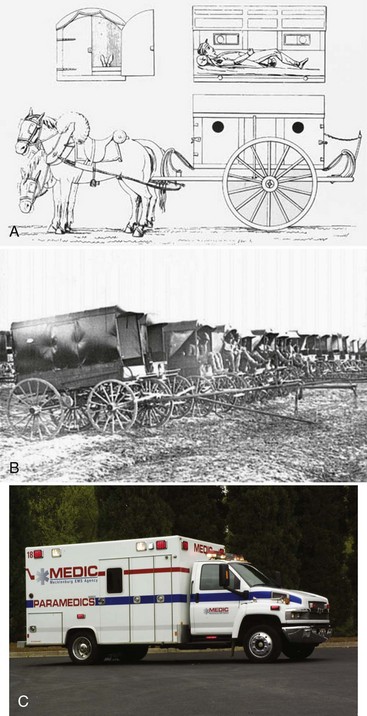
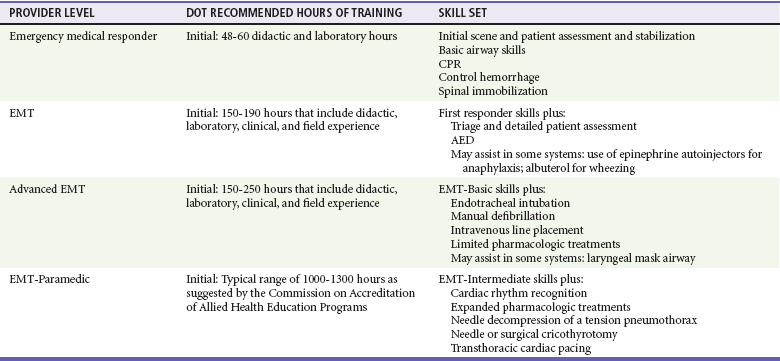
Chapter 190 Development of Emergency Medical Services Before the advent of civilian ambulance services, the sick and injured were transported by any means available, including passerby motorists, wagons, farm machinery, delivery carts, buses, and taxicabs. Figure 190-1 depicts the early Larrey ambulance used during the Napoleonic Wars, the Rucker wagon used during the American Civil War, and a modern ambulance used today. In 1865, the Commercial Hospital in Cincinnati established the first hospital-based ambulance service. Four years later, the first city service began at New York’s Bellevue Hospital.1 In 1965, the President’s Commission on Highway Safety recommended a National Accident Response Program to decrease death and injury from highway accidents.2 Results from a second national survey by the National Academy of Sciences–National Research Council were used to draft a white paper entitled Accidental Death and Disability: The Neglected Disease of Modern Society.3 Published in 1966, this document described the hazardous conditions of emergency care provision at all levels and outlined the necessary building blocks for future maturation of emergency medical services (EMS). These national efforts were the impetus for congressional legislation that directed the U.S. Department of Transportation (DOT)–National Highway Traffic Safety Administration (NHTSA) to develop a program for improving emergency medical care. During the mid-1960s, out-of-hospital cardiac care included field defibrillation programs in Belfast, Northern Ireland, and cardiac arrest research in several U.S. cities.4,5 In 1969, the first National Conference on EMS convened, resulting in the development of a curriculum, certification process, and national registry for the emergency medical technician–ambulance (EMT-A). By 1972, the U.S. Department of Labor recognized the EMT as an occupational specialty.6 Interested physicians and nurses later provided advanced educational courses and practical experiences for the EMTs, and thus began the paramedic providers.7,8 Additional programs prompted Congressional passage of the EMS Systems Act of 1973 (P.L. 93-154), which authorized funding that dramatically improved the development of comprehensive regional EMS delivery systems. Efforts to improve pediatric emergency care occurred in 1984 when Congress adopted the Emergency Medical Services for Children (EMS-C) initiative through the Health Services, Preventive Health Services, and Home Community Based Services Act of 1984 (P.L. 98-555).9 An Institute of Medicine (IOM) study, released in 1994, promoted the integration of EMS-C not just into existing EMS systems but into comprehensive systems of care provision, including injury prevention, primary and definitive care, and rehabilitation services.10 In 1996, the NHTSA published Emergency Medical Services Agenda for the Future, which broadly outlined the principles required for future EMS development.11 All components of an EMS system, both operational and clinical, were identified and discussed. This document has been used by many individuals and organizations as valuable reference material for planning, administration, and forecasting of the future of EMS delivery. More than 40 years since publishing the 1966 white paper, the IOM released a report on the status of emergency care entitled The Future of Emergency Care in United States Health System. The report focused on three separate yet related topics: (1) emergency care: at the breaking point, (2) emergency medical services at the crossroads, and (3) emergency care for children: growing pains.12–14 Multiple EMS system designs exist, all predicated on the type of community served. Whereas this is a local decision, all states incorporate an administrative office that governs or oversees the provision of EMS activities. Typically the role is not to direct any individual service but to assist in planning, licensing services, and establishing or enforcing the scope and standards for practice. Other functions may include training, examining, certifying, and recertifying providers; record keeping; data collection; and auditing or investigating programs. A description of systems for the 200 most populous cities in the United States is periodically published in the Journal of Emergency Medical Services.15 For simplicity, the following categorization of systems is used: private and public agencies; basic life support (BLS) and advanced life support (ALS) services; and single-tiered, multitiered, and first responder systems. BLS systems may be associated with poor survival rates from out-of-hospital cardiac arrest, especially those not incorporating AED technology.16 Alternatively, there is debate on the effectiveness of ALS for medical and traumatic emergencies.17 Despite this evidence, few urban communities across the United States operate solely at the BLS level. Many rural and some suburban EMS services rely on volunteers who may not wish to become advanced-level providers. Because these services may have low call volumes, it becomes more difficult for personnel to maintain advanced skills and a proficient knowledge base. Also, such communities may not have access to medical supervision or hospital sponsorship for ALS care.18 The number of EMT-Ps in any jurisdiction has come under scrutiny, in that cities with more paramedics per capita tend to have lower survival rates.19 Although this may seem implausible, one explanation might be that the number of patient encounters per paramedic decreases and the sharpness of skills degrades when that community is saturated with paramedics. The design of an EMS system is targeted toward providing quality patient care in the briefest time after unexpected injury or illness. A desirable and cost-effective design might include BLS nontransport first responders with short response times (average 2-4 minutes), having the capability of providing early defibrillation and airway support, coupled with ensuing ALS care and transport services.20 At the federal level, the NHTSA is responsible for development of the education standards and scope of practice for the different certification levels. The National EMS Education Agenda21 and the National EMS Scope of Practice Model22 now define the curriculum, education content, and core competencies for each level of provider. Individual state legislation is responsible for provider levels recognized, initial and continuing medical education requirements at each level, testing, and time intervals for course completion and recertification. The following sections outline the new suggested levels of provider and incorporated skills. Suggested hours of training are listed in Table 190-1. The four elements referred to as the chain of survival by the American Heart Association, which decrease mortality from out-of-hospital cardiac arrest, are early access to care, CPR, defibrillation, and advanced airway management and medications.23 Because early defibrillation may improve the odds of survival of out-of-hospital cardiac arrest, the use of an AED should be a mandatory procedure for the emergency medical responder.24 In 1995, the NHTSA released the revised EMT curriculum to include 46 lessons, each with cognitive, effective, and psychomotor objectives.25 Many states expanded the course to include more skills, such as AED use, epinephrine autoinjections, albuterol administration by hand-held nebulizer or metered-dose inhaler, and use of adjunctive airway devices such as the extraglottic airway. The initial training course for the EMT-P includes didactic, clinical, and field education. All course content focuses on technical and professional competencies. Additional modules are included that allow programs to incorporate an expanded scope of practice.26 With the expansion of EMS technology and management career options, many paramedic educational programs have advanced from 1-year certificate curriculums to 2-year associate or 4-year baccalaureate degrees. The National EMS Education Standards document recommends that all paramedic education programs be accredited in the future by the Commission on Accreditation of Allied Health Education Programs. To complement many of the educational issues addressed in the EMS Agenda for the Future document and at the request of the National Association of State EMS Officials (NASEMSO), the NHTSA along with the Health Resources and Services Administration under the Department of Health and Human Services published the Emergency Medical Services Education Agenda for the Future: A Systems Approach in 2000.27 This document sets forth the processes required to improve EMS education delivery similar to what is realized with other allied health care professions, provides a means of ensuring more instructor flexibility and EMS adaptation to community needs and resources, and moves toward standardization of all levels of certification across the United States. From this document, multiple activities have been completed and published, including the National EMS Core Content, a National EMS Scope of Practice Model of minimum competencies, and the 2009 National EMS Education Standards, which would ultimately replace the current National Standard Curricula for each level of provider. The NASEMSO has been collaborating with multiple EMS stakeholders and the federal partner organizations to assist states in implementing this agenda. The National Registry of Emergency Medical Technicians is in the process of revising their examination, with a new paramedic examination being finalized by January 2013. Future goals include the establishment of a national EMS certification program, consistent levels of provider that build off of each advancing level (emergency medical responder, emergency medical technician, advanced emergency medical technician, and paramedic), the requirement for educational programs to be nationally accredited, and the limitation of examinations only to those graduates who completed these accredited programs. Before the mid-1960s, few if any regulations governed system design, operations, and equipment. As EMS development progressed, guidelines for emergency vehicle specifications were adopted by the DOT and equipment lists were proposed. Today, collaborative efforts from multiple professional medical colleges and organizations continue to publish documents that recommend design, equipment, and medications for ambulances.28 During the 1980s, many believed that prehospital drug administration was unjustified and simply delayed hospital transport.29,30 Moreover, although there was a profound paucity of outcomes-based research into the use of various medications and practices in the prehospital environment, this has been improved in recent years.31 There is significant evidence for early defibrillation and certain advanced cardiac life support medications, which are carried by most ALS services.24,32 The wide variety of alternative medications is less uniform. This includes respiratory and anaphylaxis medications, preparations for altered mental status, analgesics, and antiemetics. Medications are traditionally administered in the field by the parenteral route, but the intranasal route is becoming popular for certain preparations. The beneficial aspects are that absorption is rapid with an onset of action similar to that of parenteral administration. Medications that are commonly administered intranasally are naloxone for narcotic overdose, midazolam for pediatric seizure, and fentanyl for pain control.33,34
Emergency Medical Services
Overview and Ground Transport
Perspective
Emergency Medical Service Systems
Basic Life Support and Advanced Life Support Service
Single-Tiered, Multitiered, and First Responder Systems
Levels of Provider and Scope of Practice
Emergency Medical Responder
Emergency Medical Technician
Emergency Medical Technician–Paramedic
Future
Material Resources
Medications
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Emergency Medical Services: Overview and Ground Transport
Only gold members can continue reading. Log In or Register to continue