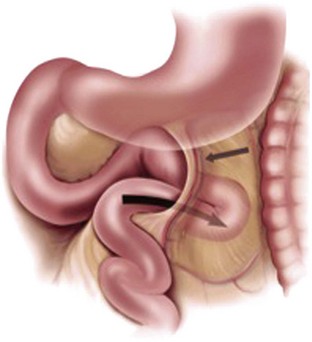
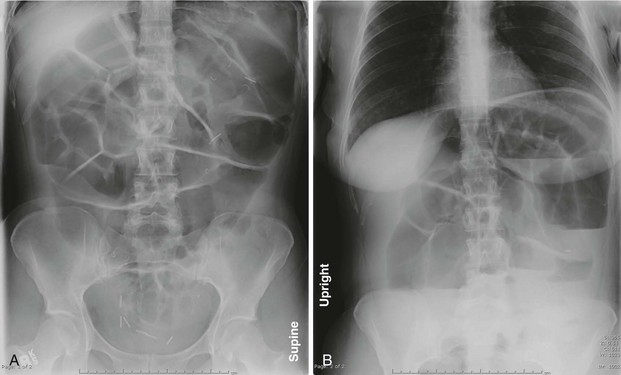
Chapter 92 The signs and symptoms of small bowel obstruction (SBO), as well as the potentially life-threatening nature of the condition, have been recognized since ancient times. The Egyptian Ebers Papyrus, which is thought to date to as early as 3400 BC, contains an ominous passage detailing what some modern researchers have suggested may describe a small intestinal volvulus. It states, “if thou examinest one who suffers…with colicky pains, and whose belly is stiff through it, and has pain in his cardia…nor is there any way it can come out, then it shall rot in his belly…it grows into a twist in the bowel.”1 Over the centuries numerous therapeutic treatments have been used to treat SBO, including the administration of metallic mercury, opium, enemas, inflation of the bowels with air, electrical stimulation, percutaneous puncture of the bowel, horseback riding, leeches, and even “suspending the patient in an upside-down position over an attendant’s shoulder,” as suggested by Sir Astley Cooper in 1804 to assist in the reduction of a hernia, and by Jonathan Hutchinson in 1878 to treat intussusception.2 By the close of the 19th century, proximal intestinal decompression via gastric suctioning was found to quickly reduce the symptoms of intestinal obstruction. Although the management of SBO has remained challenging, over the last century advancements in imaging as well as operative techniques have greatly improved the prognosis for patients with this condition and have decreased the mortality rate from nearly 60% in 1900 to less than 8% today.3,4 Intestinal obstruction is a relatively common problem encountered in the emergency department (ED), accounting for an estimated 15% of all emergency admissions for abdominal pain.5 This translates to over 300,000 patients per year in the United States, at an estimated yearly cost of over 1.3 billion dollars for the treatment of SBOs caused by adhesions alone.6 Despite the high frequency with which SBO is encountered, the ideal management remains controversial. There are several different types of SBO with a vast array of causes ranging from the common to the truly unusual. The term mechanical obstruction implies the presence of a physical barrier to the movement of the intestinal contents. Obstructions of this type can be further subclassified according to the cause of the obstruction relative to the intestinal wall (Box 92-1). Lesions external to the intestinal tract can cause obstruction via compression from outside the gut. This is most commonly a result of postoperative adhesions, but hernias and intraperitoneal neoplasms are other causes. Lesions intrinsic to the intestinal wall itself can cause mechanical obstruction; such lesions include primary intestinal neoplasms, localized infection (i. e., intestinal wall TB), and trauma-related conditions (i. e., a hematoma of the intestinal wall). Lesions within the intestinal lumen itself can lead to obstruction. Bezoars, ingested foreign bodies, and gallstone ileus are all examples of the cause of this type of obstruction.7 Another important distinction of SBO is whether the obstruction is a simple or closed-loop obstruction. A simple obstruction occurs at a single point. On the other hand, in a closed-loop type obstruction the intestine is obstructed at two locations, which creates a segment of bowel with both proximal and distal blood flow compromised. This can occur when a twist develops in the mesentery or, in the case of an internal hernia, when a loop of bowel becomes entrapped in a defect in the mesentery (Fig. 92-1). If not promptly recognized and relieved, a closed loop obstruction can quickly lead to intestinal infarction and necrosis, which, in most studies, has been shown to double the mortality rate.8 In contrast to a mechanical obstruction, a neurogenic or functional obstruction occurs as a result of disruption of the normal coordinated peristaltic activity of the gastrointestinal tract in the absence of a physical blockage within the intestinal lumen. This is also commonly referred to as an adynamic ileus. The causes of adynamic ileus are listed in Box 92-2. Most often it occurs in patients who have undergone abdominal surgery and is transient in nature. In fact, some degree of functional obstruction is considered normal after surgery and is thought to result from multiple factors, including an inflammatory response to intestinal manipulation, the effects of analgesics, and the release of hormones and several neurotransmitters.9 In addition to surgery, a number of metabolic abnormalities and medical conditions can lead to the development of a functional SBO, including infection, medications, and metabolic abnormalities. Finally, the term pseudo-obstruction refers to a poorly understood and complex syndrome in which the signs and symptoms of a mechanical obstruction, including the appearance of dilated bowel on radiography, are present in the absence of a mechanical lesion. This is thought to involve disruption of the intestinal “pacemaker activity” controlled by a specialized group of cells found in the gastrointestinal tract called the interstitial cells of Cajal (ICCs). These cells regulate the contractility of the intestinal smooth muscle and are under the influence of the enteric nervous and autonomic systems. Because of this, pathology at any one of these sites can lead to pseudo-obstruction. Pseudo-obstruction can arise from many causes, including degenerative neuropathies, autoimmune and paraneoplastic disease, and hereditary conditions.10 Unlike in adynamic ileus, the symptoms of pseudo-obstruction are often chronic and respond poorly to treatment. In the developed world the most common cause of SBO is postoperative adhesions, which account for approximately 60% of cases. These adhesions develop as a result of a process involving the interaction among numerous types of cells, cytokines, and coagulation factors caused by damage to peritoneal surfaces.11,12 It has been estimated that 93 to 100% of patients who undergo transperitoneal surgery will develop postoperative adhesions.13 Of these, up to 25% will develop SBO, with those undergoing intestinal or pelvic surgeries at greater risk.14 Over the last several years, numerous physical bioabsorbable barriers and pharmacologic agents have been evaluated as potentially useful in decreasing the formation of postoperative adhesions.15 The second most common cause of SBO is tumors, which are responsible for roughly 20% of cases. This includes both malignancies, such as adenocarcinomas, carcinoid tumors, lymphomas, and sarcomas, and benign conditions, including adenomas, leiomyomas, and lipomas.16 In addition to these primary gastrointestinal tumors, gynecologic cancers, especially ovarian cancer, are a very common cause of SBO.17 There are also numerous case reports of metastatic disease leading to SBO, including metastatic breast, skin, and testicular cancers.18 Although rare in the general population, internal hernias (Fig. 92-1) are a recognized complication of bariatric surgery, especially when a Roux-en-Y type procedure has been performed. In this group, internal hernias have been described in up to 5% of patients and usually develop at the mesocolic window.19 Another rare type of hernia is the obturator hernia. This hernia develops into the obturator foramen and is especially common in elderly women who have recently lost a significant amount of weight. The female pelvis is wider and the obturator canal is more oblique in women than in men. This, in combination with a loss of preperitoneal fat in elder, often emaciated patients, predisposes to the development of an obturator hernia. Because an external mass is absent, the diagnosis can be especially challenging, which explains why it carries the highest mortality of any abdominal hernia, at nearly 70% when incarcerated.20 Gallstone ileus is another rare but important cause of mechanical SBO (Fig. 92-2). It is responsible for 1 to 4% of all cases of mechanical obstruction and is most frequently seen in elder patients with significant underlying medical problems.21 The pathogenesis involves the entry of a gallstone into the intestinal tract through a biliary-enteric fistula. This results from the localized inflammation of cholecystitis, and in the majority of cases entry occurs via a cholecystoduodenal fistula, although cholecystocolonic and cholecystogastric fistulae can also be involved. After entering the intestinal lumen, the gallstone migrates distally. As a stone moves through the intestinal lumen, it often increases in size as bowel content sedimentation attaches. Eventually, the gallstone becomes lodged, most often in the ileum, which is the narrowest segment of the small bowel, and the patient then develops symptoms of obstruction. Figure 92-2 Gallstone ileus of the small intestine at laparotomy. (Photograph courtesy J.C. Campbell, Plymouth, England. www.surgical-tutor.org.uk Accessed February 15, 2011.) Small bowel volvulus occurs infrequently in this country but is a potentially catastrophic cause of SBO. This condition results from the abnormal twisting of a loop of small bowel around the axis of its own mesentery. This accounts for only 3.5 to 6.2% of SBO in the Western world. However, it is much more common in Africa, India, and the Middle East, where it is responsible for up to 20% of cases of SBO.22 Primary small bowel volvulus occurs in an otherwise normal abdominal cavity; secondary small bowel volvulus occurs when a congenital or acquired abnormality leads to the development of the volvulus, as in the case of intestinal malrotation or as a result of postoperative adhesions.23 Although primary small bowel volvulus is poorly understood, there are several proposed factors that may predispose to its development. Diet is thought to play a role in some cases. One study found a tenfold increase in the incidence of small bowel volvulus among Muslims in Afghanistan during the festival of Ramadan.24 During this period observers abstain from food or drink from dawn to sunset and then consume large quantities of food and liquid. The researchers proposed that eating a large amount of food bulk after prolonged fasting causes the proximal jejunum to descend into the pelvis, displacing empty small bowel loops upward and initiating malrotation. Alterations in gut motility and increased small bowel length have also been suggested as possible predisposing factors. Secondary causes of small bowel volvulus include intestinal malrotation caused by the arrest of normal rotation of the embryonic gut or as a result of postoperative adhesions. In the case of malrotation, more than 50% of affected children present for evaluation before 1 month of age with small bowel volvulus.25 Because a small bowel volvulus is a classic closed-loop obstruction, prompt recognition and surgical treatment are imperative, as the risk of strangulation is high. Intussusception describes the invagination or “telescoping” of a part of the small intestine into itself. This results in the development of venous and lymphatic congestion with consequent intestinal edema, which can lead to intestinal ischemia and perforation. Intussusception occurs in patients of all ages but is most frequently seen in children younger than 2 years. It is the most common cause of intestinal obstruction in infants 6 to 36 months of age.26 In children the cause is most often idiopathic, but several studies have shown an association with adenovirus infection. It has been postulated that enteric adenovirus infection may trigger stimulation of the lymphatic tissue in the intestinal tract, which may create a “lead point” for the intestine to be “dragged” into itself by the normal peristaltic activity of the intestines.27 In contrast to the idiopathic nature of intussusception in children, a mechanical cause is found in more than 90% of adult cases. Tumors, either benign or malignant, are discovered as the initiating cause in more than 65% of adult cases. Several reports have also described adult intussusception in association with acquired immunodeficiency syndrome (AIDS).28 These patients are at an increased risk of lymphoma or unusual infections, such as atypical mycobacterial infections, as the cause of the development of intussusception. As with all patients in the ED, the physical examination should start with a careful evaluation of the patient’s hemodynamic status, degree of distress, and general condition. Thus patients requiring resuscitation can be quickly identified, and the appropriate interventions, including aggressive intravenous fluids, can be initiated early. Inspection of the patient should include a careful search for abdominal distention and hernias and should include a genital examination. Although bowel sounds in SBO are frequently described as high pitched and “tinkling” in nature, studies have shown that they are also frequently decreased or absent in SBO. One study showed that physicians listening to recordings of bowel sounds were able to correctly identify SBO in only 42% of affected patients.29 There are numerous serious complications associated with SBO. Persistent vomiting can lead to significant hypovolemia, metabolic alkalosis, and shock. If strangulation occurs, necrosis of the bowel can lead to perforation and leakage of contaminated bowel contents into the peritoneal space. This can cause peritonitis, intra-abdominal abscess formation, and sepsis. As one would expect, complications are more common in older patients and in those with comorbidities.30 There are also several potential complications related to surgical intervention for SBO, including wound infection and short bowel syndrome. Unfortunately, in addition to these adverse events, the rate of recurrence of SBO is quite high. For patients treated nonoperatively the rate is 40%, and in those treated operatively, 27%.31 For patients with SBO secondary to adhesions, the relative risk of recurrence increases with the number of prior episodes of obstruction. For those with four or more episodes of adhesional SBO, the recurrence rate is more than 80%.32 Although laboratory tests are not helpful in diagnosing the presence of SBO, they can be very useful in assessing the degree of dehydration and metabolic disruption resulting from the obstruction. Several studies have evaluated the use of various biomarkers to identify strangulation complicating SBO. These have included lactate and creatinine phosphokinase (CPK), and some studies have evaluated the use of intestinal fatty acid binding protein (I-FABP), which is released by necrotic enterocytes, to attempt to identify strangulation.33 Unfortunately, these may be normal until very late in the process of intestinal strangulation and have proven to be overall unreliable. Several imaging modalities are applicable in the diagnosis and evaluation of SBO. Plain radiographic findings are estimated to be diagnostic in approximately 50 to 60% of cases of SBO, equivocal in 20 to 30%, and normal, nonspecific, or misleading in 10 to 20%. The cause of the obstruction can rarely be elicited from plain radiographs. In addition, there is occasionally a discrepancy between terms used by emergency physicians and radiologists to describe abdominal plain film results. For example, many emergency physicians use the term “nonspecific bowel gas pattern” to mean normal. However, one survey showed that 65% of radiologists use that same term to describe normal bowel gas findings, 22% use it to mean that they cannot tell if the findings are normal or abnormal, and 13% use it to indicate an abnormal study, but one in which they cannot determine if the findings represent mechanical obstruction or adynamic ileus.34 Abdominal plain film radiographs should include both supine and upright or decubitus studies. An upright chest radiograph may also be obtained to evaluate for subdiaphragmatic free air resulting from a bowel perforation. Characteristic plain radiographic findings of SBO include distended loops of bowel, normally greater than 3 cm in diameter, seen centrally in the radiograph (Fig. 92-3). In addition, unlike the haustra of the large intestine, which do not cross the full diameter of the bowel, the valvulae conniventes (or plicae circulares) of the small bowel cross the entire lumen of the small intestine. Noting these structures crossing the lumen of distended bowel on plain radiographs helps to differentiate SBO from large bowel obstruction. In general, the greater the number of distended loops, the more distal the obstruction. No gas should be seen in the large bowel, unless the films are obtained early in the course of the obstruction, or in the presence of a partial SBO.
Disorders of the Small Intestine
Small Bowel Obstruction
Principles of Disease

Clinical Features
Physical Examination
Complications
Diagnostic Strategies
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Disorders of the Small Intestine
Only gold members can continue reading. Log In or Register to continue