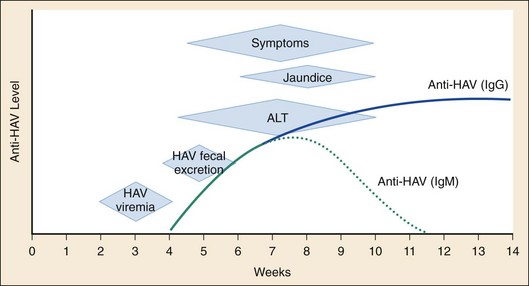
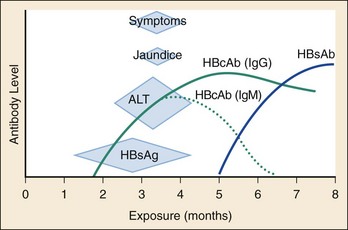
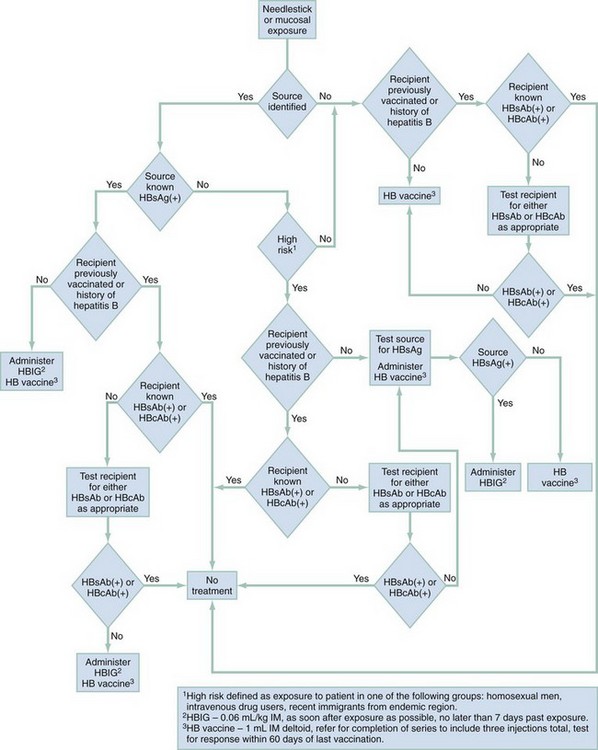
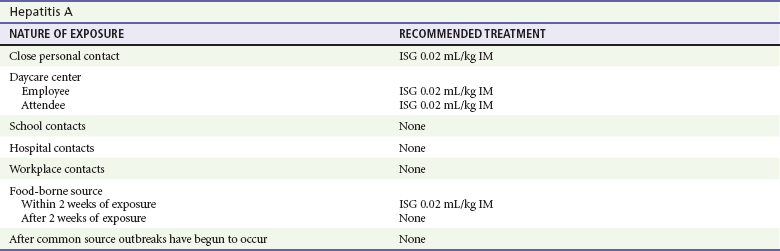
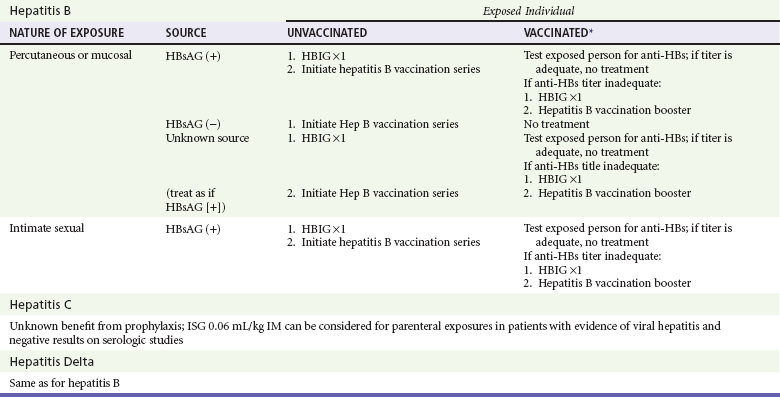
Chapter 90 Epidemiology: The number of cases of hepatitis A declined steadily from 12.0 cases per 100,000 population in 1995 to 1.0 case per 100,000 population in 2007.1,2 Western states have historically shown a higher incidence of hepatitis A, which in 1999 led to routine vaccinations of children from these areas. The greater decline in incidence of hepatitis A among children has resulted in a relative increase in the proportion of cases among adults.3 The number of reported cases of hepatitis B declined by more than 80% in the interval between 1990 and 2005, again with the greatest decline occurring among children younger than 15 years.3 The number of new cases of hepatitis C declined by approximately 80% during this period.2 The reduced rates of hepatitis A and B most likely reflect today’s broad use of effective vaccines.4 Since the late 1980s, the incidence of acute hepatitis C has declined as a consequence of improved blood product screening. A majority of cases occur among adults, with injection drug use recognized as the most common risk factor.3 Hepatitis A virus (HAV), the causative agent of hepatitis A, is an RNA enteroviral picornavirus. It is spread by the fecal-oral route either directly or through contaminated water or foodstuffs. Transmission by blood is a theoretic possibility but is exceedingly rare. HAV can occur sporadically but is notorious for its association with epidemics generally linked to common-source outbreaks. HAV infection is common worldwide; serologic evidence of previous infection exists in nearly 100% of the adult population in some regions. In the United States, close to one half of all urban-dwelling adults are seropositive for antibody for HAV.5 High rates of seropositivity in association with the relatively small number of reported episodes support the notion that many cases may be asymptomatic. Occult disease appears to be more common in children, and 70% of those infected may be asymptomatic.5 The incidence of hepatitis A infection varies among ethnic groups. In the United States, the incidence among different geographic areas and ethnic groups has changed notably since endemic areas have been targeted for routine vaccination of children. In 2005, recommendations on immunization were expanded to include routine vaccination of children in all 50 states.5 The declines have shifted the pattern of reported risk factors, showing an increasing proportion of cases among adults—specifically, men who have sex with men (MSM), illicit intravenous drug users (IVDUs), and non–injection drug users. The most common risk factor for hepatitis A in persons older than 15 years of age is travel outside of the United States.1,2,5 The typical incubation period for hepatitis A is 30 days, with a range of 15 to 45 days. Viremia is of relatively short duration and is most prominent before the onset of symptoms. Fecal shedding and maximum infectivity occur before the onset of symptomatic disease and generally have waned by the time jaundice appears (Fig. 90-1). HAV is not associated with a chronic carrier state. HBsAg has been detected in a variety of bodily secretions, including saliva, semen, stool, tears, urine, and vaginal secretions. Although the presence of HBsAg is not synonymous with infectivity, HBV DNA has been identified in several of these fluids and is likely to be infectious. The typical interval between exposure and onset of clinical illness is 60 to 90 days; however, serologic markers of infection generally appear within 1 to 3 weeks (Fig. 90-2). Approximately 10% of adults and 90% of infected neonates with immature immune systems will become asymptomatic chronic carriers of HBsAg.6 Health care workers who routinely come in contact with blood have a prevalence of HBsAg of 1 to 2%, and 15 to 30% show serologic evidence of previous infection. Among emergency physicians, seropositivity rates of 12% and 15% have been reported.7 The likelihood of becoming chronically infected with HBV varies inversely with the age at which infection occurs. HBV transmitted from HBsAg-positive mothers to their newborns results in HBV carriage in up to 90% of infants, whereas only 6 to 10% of acutely infected adults become carriers.6 In general, less than 5% of hepatitis B infections in healthy immunocompetent adults will progress to chronic hepatitis.8 Chronic hepatitis is most commonly defined as the presence of HBsAg in serum for longer than 6 months, serum HBV DNA greater than 20,000 IU/mL (105 copies/mL) (lower values are often seen in HBeAg-negative chronic hepatitis B), persistent or intermittent elevation in ALT/AST levels, and a liver biopsy showing chronic hepatitis with moderate or severe necroinflammation.9 What was historically referred to as non-A, non-B hepatitis is caused by at least two distinct RNA viruses: hepatitis C virus (HCV) and hepatitis E virus. Before the advent of widespread screening of the blood supply in 1992, hepatitis C was commonly transmitted through blood transfusions and organ transplants in the United States. With the screening of donor blood for surrogate markers (aminotransferases), antibody to hepatitis C, and nucleic acid amplification testing, the hepatitis C transmission risk from blood transfusion has been reduced to approximately 1 in 2 million blood units.10 The strongest risk factors for HCV infection are a history of intravenous drug use, having had 20 or more lifetime sex partners, and having undergone blood transfusions before 1992.11 Among patients infected with human immunodeficiency virus (HIV), the incidence of coinfection with hepatitis C is 15 to 30%. This rate approaches 50 to 90% in those who acquired HIV through intravenous drug use.12 Patients coinfected with HIV and HCV generally have a more aggressive course of both infections. In 40 to 57% of cases of hepatitis C, no source of infection is identified. The incubation period for hepatitis C is 30 to 90 days, with a mean of 50 days. Approximately 90% of HCV infections progress to chronic hepatitis. Long-term follow-up studies indicate that clinical liver disease develops in only 10 to 20% of those infected, during a period of approximately 20 years after transfusion.12 In the United States, it is estimated that 4.1 million persons are infected with HCV, and 3.2 million persons have chronic hepatitis C infection.12 Hepatitis E, which is associated with fecal-oral transmission, is encountered most often in Asia, Africa, and Russia. Hepatitis E has an incubation period of 15 to 60 days. Hepatitis delta virus (HDV) was discovered in 1977 in liver specimens from patients with chronic HBV infection. It is a defective RNA virus that can infect only patients who are actively producing HBsAg, which is required for its viral coating. In the United States the incidence of HDV antibody is 4 to 30% of patients with chronic HBV infection.13 As a consequence of the routine association with chronic HBV infection, it is likely that many cases of HDV infection are misdiagnosed as acute or reactivated hepatitis B. HDV infection is spread in a manner similar to that for hepatitis B, being most common among IVDUs, promiscuous homosexual men, and patients with hemophilia. Infection with HDV can occur either concomitantly with HBV (coinfection) or subsequent to earlier HBV infection (superinfection), because HDV cannot replicate in the absence of HBV. In cases of superinfection the presentation may range from acute self-limited disease to fulminant hepatitis or chronic infection. Severe or fulminant hepatitis is more often observed with HBV-HDV coinfection than with HBV monoinfection.13 Hepatitis G virus (HGV), also referred to as hepatitis GB virus type C, is the most recently identified virus associated with hepatitis. It is an RNA virus in the Flaviviridae family. Transmission of HGV seems to occur through blood transfusion and parenteral exposure to blood or blood products, and possibly during intimate sexual contact. The virus has been identified in patients with acute and chronic hepatitis. However, it generally is believed to be an “innocent bystander,” with disease manifestations attributable to coinfection with another hepatitis virus.14 Principles of Disease: The pathophysiology of viral hepatitis is not completely understood. In the most common varieties of hepatitis, liver injury appears to be related to the development of the immunologic response to infection rather than to the cytopathologic effect of the virus. HDV appears to be an exception, having significant direct cytotoxic potential. Clinical Features: The clinical presentation of viral hepatitis is highly variable. A significant number of cases, possibly a majority, are asymptomatic. The protean nature of symptoms and the common occurrence of anicteric disease can result in misdiagnosis. The most common symptoms and signs are malaise, fever, and anorexia, followed by nausea, vomiting, abdominal discomfort, and diarrhea. The first symptom leading to physician consultation typically is jaundice. A small number of patients with hepatitis B may experience a prodromal illness characterized by arthralgia or arthritis and dermatitis. The joint involvement typically is polyarticular; the small joints of the hands and the wrists are most commonly affected. Joint fluid usually is noninflammatory, but cell counts for aspirated fluid can be as high as 90,000/mm3. The characteristic dermatitis is urticarial but may be macular, papular, or petechial. Diagnostic Strategies: Laboratory tests are critically important in diagnosing hepatitis and determining the specific cause. The most useful tests are measurements of the hepatic aminotransferases and bilirubin. Typically, hepatitis is associated with elevations (tenfold to 100-fold) of serum aspartate aminotransferase (AST) and alanine aminotransferase (ALT), with ALT generally elevated in excess of AST. Bilirubin may be moderately increased (5-10 mg/dL) and occasionally is markedly elevated (15-25 mg/dL). Hyperbilirubinemia typically emerges several days to a week or more after the onset of clinical symptoms. Both direct and indirect bilirubin levels are elevated in close to equal proportions. Alkaline phosphatase and lactate dehydrogenase may be elevated but rarely are more than two to three times normal. Prothrombin time (PT) or international normalized ratio (INR) is useful in assessing the degree of hepatic synthetic dysfunction. Elevation of the PT or INR may be the first clue to a complicated course. The white blood cell (WBC) count generally is not useful in the diagnosis because values range from low overall counts with a lymphocytic predominance to marked polymorphonuclear leukocytosis. Although determination of the precise cause of hepatitis can rarely be achieved in the ED, this evaluation should be initiated as soon as possible. Identification of the causative agent has significant impact on prognosis and public health issues. In this regard, it is important to be able to interpret the significance of certain serologic tests (Table 90-1). Table 90-1 Serologic Markers in Hepatitis The temporal relationships among infection, clinical symptoms, and serologic responses for the two most common causes of viral hepatitis—HAV and HBV—are delineated in Figures 90-1 and 90-2. Differential Considerations: The protean nature of the symptoms and signs associated with viral hepatitis makes the differential diagnosis of this disorder quite broad in scope. Beyond a variety of nonhepatic viral illnesses, all of the infectious, chemical, and immunologic causes of hepatic inflammation in addition to biliary tract disease must be considered. A viral cause often is suggested by a history of exposure and a suggestive medical history, but serologic tests are required for confirmation. Alcoholic hepatitis usually is associated with a history of chronic or excessive alcohol consumption, less marked elevation of hepatic transaminases, and AST levels elevated above those of ALT. Extrahepatic obstruction, cholecystitis, and cholelithiasis are excluded by their lack of association with significant elevation of aminotransferases; however, abdominal ultrasound imaging may be required to eliminate these other diseases. Management: Treatment of viral hepatitis is primarily symptomatic. It often is necessary to correct fluid and electrolyte imbalances secondary to poor oral intake or excessive diarrhea or vomiting. Antiemetics may allow resumption of adequate oral intake, thereby avoiding the need for hospital admission. In the anorexic or nauseated patient, fluid intake should be encouraged, with avoidance of solids until they are palatable. Medications requiring primarily hepatic metabolism generally do not need to be discontinued nor the dosage modified unless there is significant hepatic dysfunction. Nonessential drugs with hepatotoxic potential should be avoided. Alcohol consumption should be completely discontinued until signs of liver injury have disappeared. Although various active interventions (e.g., corticosteroid administration) have been suggested, no reliable data suggest that such therapies offer clear benefit; they may even be harmful. Complications of acute hepatitis are most commonly related to fluid or electrolyte imbalance as a result of inadequate oral intake or refractory emesis. Severe vomiting can result in upper gastrointestinal (GI) bleeding from an esophageal tear. The most severe complication of acute disease is the development of liver failure, heralded by the emergence of hepatic encephalopathy. Most patients with viral hepatitis have self-limited disease, with symptomatic and histologic resolution in 2 to 4 weeks. Chronic disease will develop in approximately 10% of patients with hepatitis B and in as many as 50 to 84% of those with hepatitis C.15 Clinical liver disease develops in only 10 to 20% of chronically infected patients within approximately 20 years after becoming infected. Many of these patients will eventually die of cirrhosis secondary to their disease.15 Disposition: Hospital admission is rarely required for management of viral hepatitis and generally is reserved for the patient with significant fluid and electrolyte imbalance or refractory vomiting. Patients with less severe illness may require hospitalization for concomitant medical problems or if suitable living arrangements are not available. Altered sensorium, prolongation of the PT beyond 5 seconds, or increase in the INR above 1.5 may suggest fulminant disease or an increased likelihood of a complicated course, necessitating hospitalization for observation. The emergence of fulminant disease should lead to consideration of transfer to a facility that can offer liver transplantation. Treatment with interferon alfa-2b has resulted in a 35 to 45% remission rate after a 4-month course of treatment in selected patients with active immune responses in the symptomatic stage 2 period of hepatitis B infection. Early treatment of acute hepatitis C infection with interferon alfa-2b alone prevents the development of chronic HCV infection in most patients.15 Hepatitis C treatment recommendations suggest that duration of treatment with interferon and ribavirin should be based on the HCV genotype and pretreatment viral load. Polyethylene glycol added to interferon alfa (peginterferon alfa) extends the half-life and duration of the therapeutic activity of the interferon. Corresponding clinical benefits include both a higher rate of response than with conventional daily interferon monotherapy and feasibility of once-weekly administration. Referral to a hepatic disease specialist is recommended. Viral hepatitis is a reportable disease requiring notification of the local health department. Immunoprophylaxis should be provided to the patient’s family members and close personal contacts. Although the nature of prophylaxis depends on the specific viral cause, it is wise to offer gamma globulin to household contacts immediately unless they are known to have been previously immunized, pending serologic determination. Table 90-2 outlines the guidelines for immunoprophylaxis. Patients with HAV infection who process or handle food must not return to work while potentially infectious. Although infectivity is greatly diminished by the time jaundice emerges, it is best to delay return to work until after jaundice has cleared. Table 90-2 Postexposure Hepatitis Prophylaxis *The HB vaccine recombinant dose comes in three formulations (pediatrics, adults, and those on hemodialysis). The adult formulation (without preservative) comes in a concentration of 10 µg/mL. The dose is 1 mL for adults. Each 1-mL dose contains 10 µg of hepatitis B surface antigen. Adapted from Protection against viral hepatitis. Recommendations of the Immunization Practices Advisory Committee (ACIP). MMWR Recomm Rep 39(RR-2):1, 1990 and Guidelines for the management of occupational exposures to HBV, HVC and HIV: recommendations for postexposure prophylaxis. MMWR Recomm Rep 50(RR-11):1-42, 2001. Effective preexposure and postexposure prophylaxis for HBV has been available for more than two decades. The rates of seropositivity for HBV infection among health care workers have historically been high compared with those in the general population. Health care workers in an ED are at increased risk because of frequent contact with blood and interaction with high-risk patients. Historically, the seropositivity rate among ED nurses is 30%, and among ED physicians it is 12 to 15%.11 The 1-year risk of infection among unimmunized emergency physicians is approximately 0.25%, with a 30-year risk approaching 7.5%. During a 30-year career, the risk of death from hepatitis B is estimated at 1 in 540.16 Markers for hepatitis C were identified in 18% of patients in an inner-city ED; the potential associated health risk to staff is unknown. All ED personnel involved in patient care or custodial work should be vaccinated for HBV before or soon after starting employment. The vaccine is highly effective and associated with minimal acute or delayed toxicity. A complete three-injection series of vaccine produces protective antibody in approximately 95% of persons.17 Optimal immunologic response is obtained with deltoid injection. Hepatitis B immune globulin (HBIG) is recommended for immediate passive immunization of persons not previously immunized who have been exposed to potentially infective material. HBIG alone diminishes the risk of HBV infection by 75%.17 Unvaccinated, exposed people should receive HBIG 0.06 mL/kg intramuscularly (IM) in addition to the HBV vaccine. Concerns related to the potential risk of HIV infection from gamma globulin preparations are unfounded. Figure 90-3 outlines an approach for managing health care workers exposed to blood or other potentially infectious secretions. A safe and effective vaccine for HAV is available; however, health care workers are not currently on the list of those recommended for routine immunization. The risk of seroconversion after percutaneous exposure from an HCV-positive source is approximately 1.8%. Despite the theoretic risk of blood-borne HCV exposure among health care workers, the prevalence of HCV infection in this group is approximately the same as in the general population. No effective vaccine for HCV is available, and despite evidence to suggest effectiveness of interferon in acute hepatitis C, there is no accepted preexposure or postexposure prophylaxis regimen.18 Universal precautions—the use of gloves, masks, protective eyewear, and gowns—constitute the first and best means of defense for persons who work in proximity to potentially infective bodily fluids. Perspective: In the United States, an estimated 15 to 20 million people are chronic alcoholics. Alcohol and its metabolites are toxic to most organ systems and contribute to disease or death from many different causes. The liver is the most common site of injury from chronic ethanol ingestion. Alcoholic liver disease is the third leading preventable cause of death in the United States. Alcohol-associated mortality is disproportionately high among young people, resulting in approximately 30 years of life lost because of alcohol-associated death.19 Principles of Disease: Alcohol is largely eliminated by metabolic degradation in the liver. Approximately 2 to 15% of alcohol is excreted unchanged in the urine or expired air.20 The precise pathogenesis of alcoholic liver disease is unknown and probably is multifactorial. Coexistent malnutrition, accumulation of toxic metabolites (e.g., acetaldehyde), excessive production of nicotinamide adenine dinucleotide (NADH), induction of microsomal enzymes as a result of the metabolism of alcohol, and alteration of immune function all may play a role.20 Clinical Features: Alcoholic hepatitis is a potentially severe form of alcohol-induced liver disease. Most cases probably are subclinical, but the spectrum of presentation can range from nausea, vomiting, and abdominal pain to acute liver failure. Physical findings include tachycardia, fever, and supine or orthostatic hypotension. Abdominal tenderness usually can be elicited, especially in the right upper quadrant. Coexistent fatty infiltration may produce palpable hepatomegaly; cirrhosis from chronic disease may result in a small, nonpalpable liver. The characteristic physical signs of cirrhosis (gynecomastia, spider angiomata, muscle wasting, ascites, and palmar erythema) may be present. Jaundice can be noted in patients with a bilirubin level of at least 2.5 mg/dL. Diagnostic Strategies: Laboratory tests reveal moderate elevations of AST and ALT. Values in excess of 10 times normal are unusual, even in severe cases associated with eventual liver failure. Compared with viral hepatitis, a relative predominance of AST to ALT is expected. Bilirubin is commonly elevated. The WBC count often is high, with a polymorphonuclear leukocytosis in the range of 10,000 to 20,000/mm3. The PT and the INR provide a rough assessment of hepatic dysfunction. An acutely prolonged PT or elevated INR in a patient not suspected to have chronic cirrhotic disease suggests a complicated course. Electrolyte or acid-base disturbances may develop as a consequence of excessive vomiting or alcoholic ketoacidosis. Differential Considerations: The differential diagnosis of alcoholic hepatitis is quite broad in scope and includes a variety of other alcohol-related GI maladies (e.g., gastritis, pancreatitis). Patients often have several ethanol-induced diseases simultaneously. Initially, all of the potential etiologic disorders must be considered; however, the clinical history and aminotransferase profile should facilitate accurate diagnosis. Mild aminotransferase elevation and marked bilirubin elevation are consistent with alcoholic hepatitis; ultrasonography will differentiate this from common duct obstruction. Serum should be sent for testing for anti-HAV IgM and hepatitis B core antibody (HBcAb) IgM, but results usually are not available to establish these diagnoses in the ED. Management: Management of alcoholic hepatitis is principally supportive. Fluid and electrolyte imbalance must be corrected, usually requiring parenteral fluid replacement; antiemetics may mitigate the need for intravenous treatment. Alcohol may suppress gluconeogenesis, thereby causing hypoglycemia. Blood glucose should be measured and supplemented as indicated. Many alcoholics are malnourished, and if thiamine deficiency is suspected, thiamine should be given at a dose of 100 mg intravenously (IV) before glucose administration to avoid induction of acute Wernicke’s encephalopathy. Ethanol-induced magnesium wasting may not be apparent on serum magnesium measurement, and replacement should be given empirically unless the patient has a contraindication such as renal failure or known hypermagnesemia. Magnesium can be given as the sulfate salt in a dose of 1 g IV or IM or as an oxide, chloride salt, or amino acid conjugate for oral replacement therapy at a daily dose of 200 to 1000 mg. The overall nutritional status of the patient should be addressed with the administration of a high-calorie, vitamin-supplemented diet. Protein content may require restriction if evidence of cirrhosis and incipient encephalopathy exists. Coexisting gastritis should be treated with histamine H2 antagonists, proton pump inhibitors, or antacids. The patient should be evaluated for GI bleeding and treated appropriately. Corticosteroids, propylthiouracil, insulin-glucagon infusions, pentoxifylline, and anti–tumor necrosis factor alpha (TNF-α) therapy have been investigated for treatment of alcoholic hepatitis and look promising in severe cases, but none of these agents have gained acceptance as part of routine management.20,21 Disposition: Disposition is determined by the patient’s clinical state: the degree of fluid and electrolyte abnormality, the ability to retain oral intake, any coexistent illnesses or complications, and the patient’s socioeconomic circumstances. Admission to the hospital generally is not required. All patients should be advised to abstain from further alcohol ingestion and should be provided referral for detoxification or alcohol dependency treatment. Principles of Disease: Cirrhosis is a generic term for an end stage of chronic liver disease characterized by destruction of hepatocytes and replacement of normal hepatic architecture with fibrotic tissue and regenerative nodules. Laennec’s cirrhosis is a diffuse process that involves the entire lobule and most often is related to chronic alcohol ingestion. From 10 to 20% of chronic alcoholics develop this type of cirrhosis. Amount and duration of alcohol ingestion, heredity, and underlying nutritional status all seem to play some role in the development of this disorder. Postnecrotic cirrhosis usually is nonhomogeneous, characterized by regions of fibrosis and hepatocyte loss alternating with normal areas. It most often is a consequence of chronic hepatitis of various causes: infectious (viral, bacterial, fungal), drug induced, or metabolic. Biliary cirrhosis is much less common and is a consequence of chronic extrahepatic biliary obstruction or a primary disorder of autoimmune-mediated intrahepatic duct inflammation and scarring. Nonalcoholic fatty liver disease has become an increasingly recognized cause of cryptogenic cirrhosis. This still poorly understood disease, with features similar to those of Laennec’s cirrhosis, is more common in obese patients and those with type 2 diabetes mellitus.22 Clinical Features: The clinical manifestations of cirrhosis are related to loss of hepatocytes, leading to metabolic and synthetic dysfunction, or to fibrosis and altered hepatic architecture, resulting in impaired portal vein blood flow and portal hypertension. Typically the patient with cirrhosis complains of chronic fatigue and poor appetite. With the exception of those with biliary cirrhosis, many patients with cirrhosis can be asymptomatic until some dramatic complication develops, such as GI bleeding, ascites, or hepatic encephalopathy. Patients with biliary cirrhosis generally complain of pruritus or exhibit obvious jaundice before end-stage cirrhosis or complications develop. Primary biliary cirrhosis may be associated with other immune-mediated disorders; these patients may have signs and symptoms characteristic of scleroderma or the CREST syndrome (i.e., calcinosis cutis, Raynaud’s phenomenon, esophageal motility disorder, sclerodactyly, and telangiectasia). Diagnostic Strategies: Laboratory tests are not specific. Aminotransferase levels are rarely more than minimally elevated. Bilirubin may be increased but usually not until cirrhosis is far advanced. Elevation of alkaline phosphatase out of proportion to other liver enzymes is suggestive of biliary cirrhosis. Coagulation studies commonly show abnormalities, and the serum albumin level is low as a result of impaired hepatic synthetic function. Mild to moderate anemia and thrombocytopenia often are present in Laennec’s cirrhosis. Elevated blood urea nitrogen (BUN) or creatinine suggests dehydration or hepatorenal syndrome. Management: Treatment of cirrhosis in the ED is limited. Fluid and electrolyte imbalances should be corrected, and vitamin and nutritional supplements should be provided. Most patients can be discharged with referral to a general internist for further evaluation and treatment. Ascites associated with respiratory compromise or significant discomfort can be treated with paracentesis and removal of 2 L of fluid or more. Removal of very large quantities of ascitic fluid can result in body fluid and electrolyte abnormalities and hemodynamic instability. If SBP is a consideration, diagnostic paracentesis should be done.
Disorders of the Liver and Biliary Tract
Hepatic Disorders
Hepatitis
Viral Hepatitis
SEROLOGIC MARKER
ABBREVIATION
INTERPRETATION
Antibody to HAV
Anti-HAV
A combination of IgG and IgM antibody defining infection with HAV, acute or past
IgM antibody to HAV
Anti-HAV IgM
Antibody to HAV, indicating acute infection
Hepatitis B surface antigen
HBsAg
Surface antigen associated with acute or chronic HBV infection
Hepatitis B e antigen
HBeAg
Antigen associated with active infection, acute or chronic, and indicative of high infectivity
Antibody to B surface antigen
HBsAb
Antibody indicative of acute or past infection or immunization
Antibody to B core antigen
HBcAb
A combination of IgG and IgM antibody defining infection with HBV, acute or past
IgM antibody to B core antigen
HBcAb-IgM
Antibody to B core antigen, indicating acute infection with HBV
Antibody to B e antigen
HBeAb
Antibody to e antigen, possibly representing resolving HBV infection and decreased infectivity
Antibody to HDV
Anti-HDV
Antibody defining infection with HDV; HBsAg should be present
Antibody to HCV
Anti-HCV
A new antibody that defines infection with HCV, acute or past
Special Considerations
Alcohol-Related Liver Disease
Cirrhosis
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree