119 Disorders of Early Pregnancy
• Spontaneous abortion (before 12 weeks) will progress to completion with few complications, and incomplete or missed abortion (without shock, fever, or significant bleeding) can be managed expectantly.
• Rh0 immune globulin is effective for up to 12 weeks; no repeated dose is required if bleeding recurs in that time.
• Ectopic pregnancy is responsible for the greatest morbidity and mortality in early pregnancy; ruptured ectopic pregnancy remains responsible for 10% of pregnancy-related deaths.
• Women with a previous ectopic pregnancy have a 15% recurrence rate.
• Serum human chorionic gonadotropin (HCG) levels can vary by as much as 15% between laboratories, and an HCG level should be ordered when suspicion is high despite a negative urine HCG.
• Gestational trophoblastic disease (up to 75% of malignant cases) may develop after a nonmolar pregnancy (spontaneous and elective abortion, ectopic pregnancy, and term gestation); these patients have prolonged bleeding after delivery or miscarriage, with subsequent HCG levels that fail to return to undetectable values.
Spontaneous Abortion
Epidemiology
Spontaneous abortion, also known as miscarriage, occurs when a pregnancy ends before the fetus has reached viability. Viability correlates to a fetus larger than 500 g—or approximately the size at 20 to 22 weeks of gestation. Miscarriage is common and occurs in 25% to 30% of all pregnancies. Eighty percent of miscarriages occur before the 12th week of gestation, and up to 25% occur in pregnancies that are not even recognized clinically; in such cases human chorionic gonadotropin (HCG) can be detected in urine but the patient has no missed menses.1
Pathophysiology
The etiology of miscarriage can be classified as either intrinsic or extrinsic to the embryo. Intrinsic factors include genetic abnormalities and congenital conditions. Most cases of spontaneous abortion are due to genetic factors, either anembryonic gestations or chromosomal abnormalities. The majority of these defects arise de novo during fertilization and are not inherited. Genetic factors tend to lead to miscarriage early because of abnormal growth and development.2 In contrast, later miscarriage is more often a result of extrinsic factors.
Presenting Signs and Symptoms
Spontaneous abortion is classified as threatened, inevitable, incomplete, complete, missed, or septic. Table 119.1 lists characteristics of these categories. Symptoms of spontaneous abortion include vaginal bleeding, suprapubic cramping or pain, and passage of tissue. Bleeding can vary from minor spotting to severe hemorrhage.
Table 119.1 Classification of Spontaneous Abortion
| CATEGORY | DEFINITION, CLINICAL CHARACTERISTICS | ULTRASONOGRAPHIC FINDINGS |
|---|---|---|
| Threatened | Bleeding and/or cramping with no passage of tissue, closed os, uterine size appropriate for dates, pregnancy viable | Intrauterine pregnancy (IUP), fetal heart tones (if age appropriate) |
| Inevitable | Open os without passage of products, pregnancy nonviable | IUP or products in the cervical canal |
| Incomplete | Partial passage of products; open os, uterus not well contracted; variable bleeding; pregnancy nonviable | Persistent gestational tissue in the uterus |
| Complete | Products of pregnancy completely passed, closed os, minimal bleeding, uterus well contracted | Empty uterus |
| Missed | Intrauterine demise with no spontaneous passage of products, closed os | Absent fetal cardiac activity or anembryonic gestation, absent heart tones with a crown rump length > 5 mm, absent fetal pole with >18-mm mean sac diameter |
| Septic | Infection complicating any of the previously described categories | Persistent products of conception or hemorrhage within the uterine cavity |
Differential Diagnosis and Medical Decision Making
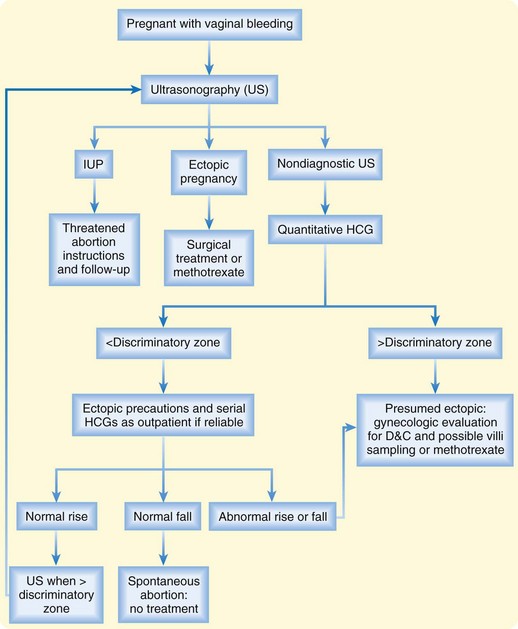
Laboratory studies include a complete blood count, quantitative HCG, and blood type with Rh status. With significant bleeding or other medical disease, coagulation parameters and typing and crossmatching for blood products should be ordered. Ultrasonography is essential for a full diagnosis and for guiding further management (Fig. 119.1). Even if it appears that the patient has passed the embryo, she should undergo ultrasound imaging to evaluate for any retained products.
Treatment
Many patients with spontaneous abortion often need little or no intervention following accurate diagnosis and exclusion of other pathology. Expectant management is the only option for threatened abortion; education and ensuring adequate follow-up care are essential. The presence of fetal heart tones in women with symptoms of threatened abortion is reassuring; less than 5% of women younger than 36 years will miscarry, but this risk rises to 29% in those older than 40.3
Incomplete or missed abortions can be managed expectantly as long as shock, fever, or significant ongoing bleeding are absent. The time course for completion of a spontaneous abortion is highly variable, and patients will need education and routine gynecologic care to plan for dilation and curettage if tissue does not pass spontaneously or if the bleeding becomes heavy. Patients should attempt to collect the products of conception for examination and should undergo subsequent ultrasonography to assess whether all products of conception have passed. Studies have proved the safety of this practice.4 Approximately 90% of patients with incomplete and 76% of those with missed abortions require no surgical treatment when managed expectantly for 4 weeks. Complications occur in 1%, less than in those managed medically.5
Prostaglandins such as misoprostol can effectively induce abortion for pregnancy failure of longer than 12 weeks and may help control bleeding in patients with inevitable or incomplete abortions. The dose of misoprostol is 800 mcg administered vaginally or rectally, but this drug should be given only after consultation with a gynecologist. One large study showed an 84% success rate.6 Misoprostol induces spontaneous abortion, so any possibility of a desired viable pregnancy must be excluded.
Surgical management includes dilation and curettage or dilation and evacuation. Indications are listed in Box 119.1. Risks associated with surgical management are small and include uterine perforation, infection, adhesions, and anesthetic complications.
Rh0 Immune Globulin
Rh0 IG is effective for up to 12 weeks after administration, so patients with recurrent bleeding who already received immunization within that time frame do not need a repeated dose. If significant hemorrhage occurs later in pregnancy, especially in the setting of trauma, additional doses are necessary. Ideally, Rh0 IG is administered within 72 hours of the event leading to fetal-maternal hemorrhage (Box 119.2).
Next Steps in Care and Follow-Up
![]() Patient Teaching Tips
Patient Teaching Tips
Spontaneous Abortion
Miscarriage affects up to one third of pregnancies. Most patients will subsequently have normal pregnancies.
Reassure the patient that in most cases genetic factors are responsible—not patient behavior.
In threatened abortion with a detectable fetal heartbeat, 95% of cases will progress to normal pregnancy.
Women with recurrent miscarriage should receive fertility and genetic evaluation.
Menses will usually resume in about 6 weeks.
Advise 2 weeks of pelvic rest and suggest waiting 2 to 3 months before trying to get pregnant again (although no studies have confirmed either recommendation).
Ectopic Pregnancy
Epidemiology
Ectopic pregnancy, in which the developing embryo implants outside the uterine cavity, is responsible for the greatest morbidity and mortality in early pregnancy. The incidence of ectopic pregnancy in the United States has increased over the past 30 years, and it now accounts for 2% of all pregnancies.7 This increase has been attributed to rising rates of pelvic inflammatory disease, as well as the advent of assisted reproductive technologies.
Pathophysiology
Risk factors for ectopic pregnancy are outlined in Box 119.3. Tubal pathology, the most significant risk factor, leads to abnormal transport and implantation of the embryo. The majority of cases arise in women with a history of pelvic inflammatory disease, and women with a previous ectopic pregnancy have a 15% recurrence rate. However, up to 50% of patients with an ectopic pregnancy have no identifiable risk factor.8
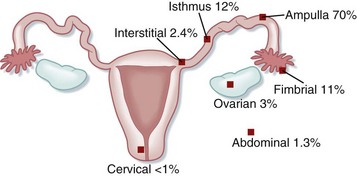
The most common location for ectopic implantation is the fallopian tube, which accounts for 95% of all ectopic pregnancies. The growing blastocyst leads to tubal distention and bleeding into the peritoneal cavity. If the pregnancy continues and is undetected, it can lead to rupture of the tube with subsequent hemorrhage. Less commonly, ectopic pregnancies implant on the ovary, abdominal viscera, or cervix. In these cases, significant hemorrhage or perforation of abdominal structures may occur. See Figure 119.2 for sites of ectopic implantation.