Chapter 28 Disorders of Cardiac Rhythm
Cardiac rhythm disturbances (arrhythmias) are common in intensive care settings, where they may represent the primary disease process or occur as a complication of management (Table 28-1).1,2 It is important to note that arrhythmias that might otherwise be well tolerated hemodynamically may be immediately life-threatening to the critically ill child. In addition, certain treatment strategies may be available in the critical care unit that normally might not be considered, particularly for serious but transient arrhythmias. Therefore response to arrhythmias in this setting should emphasize prompt restoration of hemodynamic stability concurrent with identification of the arrhythmia mechanism and predisposing factors. This chapter emphasizes the most common clinical scenarios and treatment approaches encountered in the intensive care setting while providing a broader overview of the array of arrhythmia mechanisms and their associated presentations in pediatric patients.
Table 28–1 Classification of Arrhythmias by Type and Basis
| Arrhythmia | Primary | Secondary |
|---|---|---|
| Ventricular premature beats and supraventricular premature beats | +++ | +++ |
| Sinus bradycardia, sick sinus syndrome | ++ | ++ |
| Incomplete AV block | ||
| Mobitz I | ++ | +++ |
| Mobitz II | ++ | |
| Congenital third-degree AV block | +++ | ++ |
| Acquired third-degree AV Block | ++ | |
| Paroxysmal SVT (AV reentrant tachycardia, AV nodal reentrant tachycardia) | +++ | |
| Ectopic atrial tachycardia | ++ | |
| Atrial flutter and intraatrial reentry | ++ | +++ |
| Atrial fibrillation | + | +++ |
| Chaotic atrial tachycardia | ++ | |
| Junctional ectopic tachycardia | + | +++ |
| Monomorphic ventricular tachycardia | ++ | ++ |
| Torsades des pointes | + | + |
| Ventricular fibrillation | + | ++ |
| Bidirectional ventricular tachycardia | ++ | + |
AV, Atrioventricular; SVT, supraventricular tachycardia; +++, typical; ++, occasional; +, rare.
Classification of Arrhythmias
Bradycardias
Sinus Bradycardia and Sinus Pauses
Sinus bradycardia may result from high vagal tone, hypothermia, acidosis, increased intracranial pressure, drug toxicities, or direct surgical trauma to the sinoatrial (SA) node. In otherwise well patients, intermittent sinus bradycardia or prolonged sinus pauses may be caused by intense vagal episodes, such as those occurring during neurocardiogenic syncope. Whereas vagal stimulation may produce profound bradycardia, pauses, or even asystole lasting for several seconds, transient bradycardia should not be construed as an absolute indication for pacing. However, in the hemodynamically tenuous patient, persistent or recurring bradycardias, whether attributed to sinus node exit block (periodic loss of sinus impulse) or sinus arrest, often warrant intervention with vagolytic, sympathomimetic, or pacing therapies. It is important to recognize that blocked premature atrial depolarizations (where premature P waves may be obscured in the preceding T wave) may also mimic sinus pauses or even sinus bradycardia when occurring in a bigeminal pattern. In cardiac patients, sinus node dysfunction may be the result of surgical injury or heterotaxy syndromes. Primary sinus node dysfunction in childhood is rare but has been described.3
Conduction Abnormalities
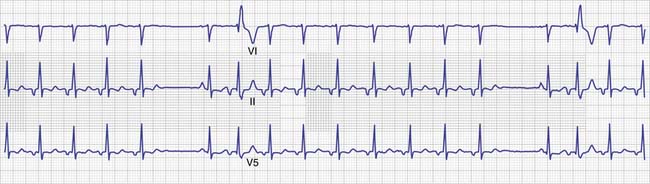
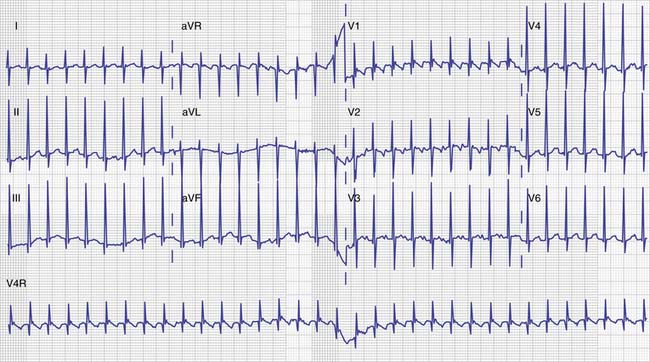
Complete or third-degree AV block represents complete loss of AV conduction, usually with a junctional or idioventricular escape rhythm that is regular but may be quite slow. Periodic shortening of the RR interval may be the only clue to distinguish complete AV block from high-grade second-degree block with intermittent conduction (Figure 28-1) or from a junctional rhythm with slower atrial rate and intermittent AV conduction.
Escape Rhythms
In the presence of sinus bradycardia or AV block, escape rhythms typically emerge from AV nodal or Purkinje cells. These rhythms are slower than the appropriate sinus rate but may become accelerated with enhanced adrenergic tone and compete with the underlying sinus rhythm. It is important to distinguish these accelerated subsidiary rhythms from both pathologic tachycardias and escape rhythms resulting from AV block. Only rarely does an accelerated junctional or ventricular rhythm result in significant symptoms in a healthy child.4 However, in the critically ill patient, the resultant loss of AV synchrony may warrant atrial pacing at a slightly faster rate if cardiac output is compromised.
Tachycardias
Classification by Mechanism
Most abnormal tachycardias encountered clinically are caused by abnormal impulse propagation in the form of reentry. This may represent reentry using an accessory AV connection (AV reentry), the AV node and its adjacent tissues (AV nodal reentry), atrial myocardium (intraatrial reentry including atrial flutter and fibrillation), or ventricular myocardium (most ventricular tachycardias). Automatic tachycardias represent abnormal impulse formation arising from either ectopic foci or usual subsidiary pacemaker tissues (atrial, junctional, or ventricular) but at a significantly accelerated rate. These tachycardias may be due to an abnormally accelerated rate of depolarization of normally automatic tissues or to diseased atrial or ventricular myocardium with a propensity to abnormal spontaneous depolarization. Triggered tachycardias are thought to arise from abnormal secondary depolarizations (afterdepolarizations) following normal myocardial depolarizations, which may propagate to adjacent tissues. These tachycardias probably are important in several specific situations such as cardiac glycoside toxicity (delayed afterdepolarizations) and drug-induced long QT syndromes (early afterdepolarizations), and they also are important in many hereditary arrhythmias syndromes. Triggered activity is often dependent on the underlying heart rate, a feature that may sometimes be exploited therapeutically.
Supraventricular Tachycardias
“Supraventricular tachycardia” (SVT), “paroxysmal atrial tachycardia,” and “paroxysmal supraventricular tachycardia” (PSVT) are descriptive but nonspecific terms commonly used interchangeably to describe tachycardias with a regular rate (usually in excess of 200 to 220 beats/min), normal QRS morphology, and P waves that either are not discernible or follow the QRS complex. This phenotype represents the most common form of SVT seen in otherwise healthy neonates and children and usually can be attributed to AV nodal reentry or AV reentry using an accessory connection (see next section). However, these typical ECG features can be produced by a more diverse array of tachycardia mechanisms.5 Furthermore, intermittent AV block or QRS prolongation may be observed in certain types of “SVT,” such that the ECG distinction of “SVT” from other atrial arrhythmias becomes obscured. Likewise, some tachycardias of supraventricular origin are associated with a widened QRS, either because of rate-related bundle branch block or anomalous antegrade conduction through an accessory connection. Therefore it is most useful to include among SVTs all tachycardias originating from the atrium, the AV node, or both, regardless of whether the ventricles participate primarily (i.e., AV reentry) or merely as a secondary consequence of AV conduction. This broad and inclusive definition appropriately allows inclusion of nonreciprocating mechanisms that need to be included in the differential diagnosis of “SVT,” such as intraatrial reentry.
Atrioventricular Reciprocating Tachycardias
AV reciprocating tachycardias use one or more accessory AV connections to allow a reentrant circuit to develop involving both atrial and ventricular tissues. By definition, they display a fixed 1:1 AV relationship. Orthodromic reciprocating tachycardia (ORT) is the most common AV reentrant tachycardia and, in otherwise normal infants, also is the most common mechanism of SVT.5,6 In ORT, antegrade conduction is over the AV node, whereas retrograde conduction to the atria occurs via an accessory AV connection. QRS morphology and duration usually are normal, with retrograde P waves often evident following each QRS complex. If the accessory connection conducts antegradely during sinus rhythm, ventricular preexcitation occurs prior to conduction over the AV node (Wolff-Parkinson-White [WPW] syndrome). The fusion of preexcited ventricular depolarization with the normal depolarization of the AV node and His-Purkinje system produces the characteristic short PR interval and Δ wave of WPW syndrome. Many patients experiencing ORT have normal QRS morphology during sinus rhythm. In these individuals the accessory pathway may only conduct retrogradely and is thus clinically evident only during tachycardia or during ventricular pacing.
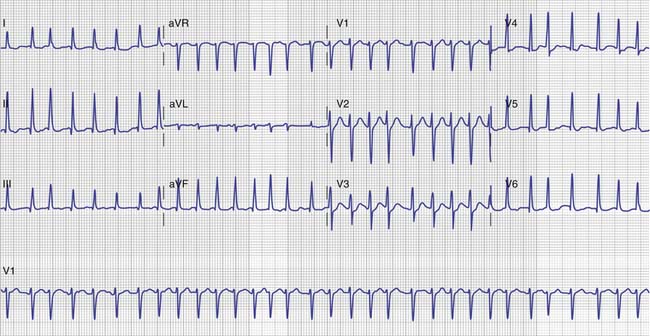
Permanent junctional reciprocating tachycardia (PJRT) is a variant of ORT with retrograde conduction over a slowly conducting accessory AV connection that possesses decremental (“AV nodelike”) conduction.7 The relative conduction and refractory properties of the accessory connection and the AV node are such that the PR interval is short or normal and tachycardia is incessant. In a single-lead rhythm strip, PJRT may mimic sinus tachycardia, although a 12-lead ECG reveals atypical P wave morphology with P-wave inversion in the inferior leads. This tachycardia typically displays repeated spontaneous termination and prompt reinitiation, resulting in incessant tachycardia until it is adequately treated (Figure 28-2).
Atrioventricular Nodal Reentrant Tachycardia
AV nodal reentrant tachycardia (AVNRT) is the most common cause of SVT in older children and young adults without WPW syndrome or structural heart disease. It is seen less commonly in infants.5,6 Occasionally it is precipitated for the first time by a serious illness or by other secondary factors associated with arrhythmias in the intensive care unit (ICU). This tachycardia can be attributed to so-called “dual AV nodal physiology.” Conceptually, one functional “limb” of the AV node typically displays slow conduction and a short refractory period, whereas the other limb typically displays more rapid conduction but a longer refractory period. The differential conduction between the two “limbs” of the AV node (slow and fast pathways) provides the functional substrate for reentry. In actuality, these “limbs” represent differential conduction properties of the fibers inputting the AV node from upper and lower approaches of the atrial septum, representing so-called “fast” and “slow” inputs.
Classically, two electrocardiographically distinct forms of AVNRT may occur. In the “typical” form of AV node reentry, antegrade conduction during tachycardia is over the slow AV node inputs, and the P waves often are obscured by the preceding QRS complex. In the “atypical” form of AV node reentry, antegrade conduction is via the fast inputs of the AV node and retrograde conduction is over the slow limb. This conduction results in a long RP and short PR with an inverted P wave. The typical form of AVNRT can be difficult to distinguish from ORT in which P waves also are often obscured. The atypical form of AVNRT may be indistinguishable from PJRT (see previous section), except that the tachycardia is paroxysmal rather than incessant. Like PJRT, atypical AVNRT must be carefully distinguished from other tachycardias with a normal PR interval, including sinus tachycardia, intraatrial reentry, or ectopic atrial tachycardias (see next section). Other atypical forms of AV nodal reentry using “intermediate” pathways can occur but are uncommon in children. Other variations of AVNRT can be characterized during the course of formal intracardiac electrophysiologic study.
Primary Atrial Tachycardias
Primary atrial tachycardias represent a diverse group of tachycardias originating solely from atrial tissue. They include tachycardias with discrete P waves (ectopic atrial tachycardia, intraatrial reentry), sawtooth flutter waves (atrial flutter), or disorganized atrial activity (atrial fibrillation, chaotic atrial tachycardia).8 The ECG appearance alone may not adequately distinguish the underlying mechanism.
Atrial fibrillation, a very common arrhythmia among the elderly, is far less common in pediatric patients. It may occur as the result of atrial myocarditis,9 as a result of an underlying reentrant SVT,10 or sometimes as the result of central venous catheters (Figure 28-3). In patients with WPW syndrome, rapid conduction over the accessory pathway may be life-threatening. When atrial fibrillation is seen, the underlying basis should be sought, because the long-term implications and treatment measures are much different than in adult patients.
Ectopic atrial tachycardia is an automatic arrhythmia that typically presents as an incessant and chronically elevated atrial rhythm that may be mistaken for sinus tachycardia, depending on the site of the automatic focus. First-degree AV block may be seen as a result of the inappropriate rate. Patients often experience no overt palpitations but rather present with ventricular dysfunction and sometimes frank congestive heart failure. In such cases, careful scrutiny of the P wave morphology and evaluation of any abrupt changes in rate (as the result of transitions between sinus and the tachycardia) are necessary to establish the diagnosis. Adenosine may inhibit the automatic focus, making this diagnosis especially difficult.
Chaotic atrial tachycardia is an uncommon arrhythmia that is usually observed in infants and toddlers, often in association with a viral respiratory illness.11 The hallmark features are a rapid and irregular atrial rate, often exceeding 300 bpm, and presence of multiple P-wave morphologies. The resulting ventricular response is irregularly irregular, simulating atrial flutter. However, this rhythm is probably the result of multiple triggered foci within the atria, and thus acute termination measures (i.e., DC cardioversion, adenosine, or pacing) are of little benefit. Usually this arrhythmia resolves within weeks or months of presentation.
Junctional Ectopic Tachycardia
Junctional ectopic tachycardia (JET) probably arises from an abnormal automatic focus or a protected microreentrant circuit in the region of the AV node or proximal His bundle. Antegrade conduction usually is over the normal His-Purkinje system with a narrow QRS. Retrograde (VA) block or complete VA dissociation with a slower atrial rate aids in the recognition of this mechanism. Variants include a congenital form, the more common postsurgical form, and paroxysmal JET described primarily in adults.12,13 As in primary atrial tachycardias, atrial depolarization may be obscure, and direct atrial recordings aid the diagnosis. Occasionally JET is associated with 1:1 VA conduction, in which case additional pacing or pharmacologic maneuvers are necessary to distinguish it from other mechanisms of SVT.
Ventricular Tachycardias
Although often regarded as a homogeneous group of arrhythmias, ventricular tachycardias actually constitute diverse rhythms, representing each of the underlying tachycardia mechanisms (reentry, automaticity, and triggered activity) with important therapeutic implications.14 Likewise, although they are sometimes lethal, they may range in complexity and severity from benign accelerated ventricular rhythm to rapid polymorphic ventricular tachycardia and ventricular fibrillation. Both the clinical setting and the QRS morphology during ventricular tachycardia may provide important clues to the mechanism and pathogenesis, anatomic origin or tachycardia focus (see incessant ventricular tachycardias), and treatment strategies, as discussed later.
Approach to Diagnosis
Surface Electrocardiogram
The surface ECG remains the cornerstone of arrhythmia diagnosis. Certainly in patients with known cardiac abnormalities, and arguably in all patients admitted to the ICU, a baseline ECG should be obtained at admission. This ECG may provide a valuable baseline for later comparison in the event of an arrhythmia. Because these arrhythmias occur in a monitored environment, a strip should be available to assess the rate, regularity, QRS morphology and duration, and AV relationship (Table 28-2), which should provide an initial differential diagnosis (Figure 28-4). Ideally, multiple leads should be inspected. For sustained tachycardias, a full 12-lead ECG should be obtained whenever possible because diagnostic details, such as QRS aberrancy, atrial rate, and P-wave morphology, or hidden features, such as “flutter waves,” may be evident only in selected leads (Figure 28-5). Most contemporary monitoring systems now have automatic arrhythmia detection and storage capabilities, allowing discrimination between a gradual versus abrupt change in rhythm or rate. Such distinctions may be key in discriminating between sinus and nonsinus tachycardias in the critical patient. Familiarity with the capabilities and limitations of the specific system available is therefore essential.
Table 28–2 Electrocardiographic Patterns
| Pattern | Description |
|---|---|
| AV BLOCK | |
| Mobitz I | Shortened PR of first conducted beat after block |
| Mobitz II | No change in PR before/after block |
| Periods of high-grade block | |
| Third-degree | Fixed, rather than variable, RR interval |
| SUPRAVENTRICULAR TACHYCARDIAS | |
| AV reentrant supraventricular tachycardia | P waves obscured or buried in ST segment |
| AV nodal reentrant supraventricular tachycardia | P waves obscured by terminal QRS |
| ”Pseudo” R′ in lead V1 during tachycardia, not sinus | |
| Junctional ectopic tachycardia | Narrow QRS tachycardia, VA dissociation |
| RR periodically shortened because of sinus capture complexes∗ | |
| Atrial ectopic tachycardia | Monotonous rate, inappropriately fast |
| Abnormal P-wave morphology (may be subtle) | |
| Intraatrial reentrant tachycardia | Inappropriately fast rate, discrete P waves, variable AV conduction in postoperative patient with congenital heart disease |
| Atrial flutter | Variable RR interval |
| Rapid, sawtooth flutter waves (>280 beats/min) | |
| Atrial fibrillation | Irregular ventricular rate |
| Coarse baseline with no discernible P waves | |
| Chaotic atrial tachycardia | Three or more P-wave morphologies, irregular atrial rate, variable AV conduction (periods or atrial flutter or fibrillation common) |
| VENTRICULAR TACHYCARDIAS | |
| Monomorphic | Wide QRS for age, different from baseline |
| Slurred upstroke of QRS | |
| Variable VA conduction† | |
| Sinus capture complexes† | |
| Idiopathic types | Left bundle branch block, inferior axis (right ventricular outflow tract origin) |
| Right bundle branch block, left superior axis (left ventricular septal origin) | |
| Bidirectional | Alternating QRS axis (beat-to-beat) |
| Torsades des pointes | Initiation with “short-long-short” sequence |
| QT-interval prolongation prior to onset | |
| “Twisting” of QRS axis |
AV, Atrioventricular; VA, ventriculoatrial.
∗ Junctional ectopic tachycardia may be associated with third-degree AV block.
† Helpful when seen; absent if 1:1 VA relationship.
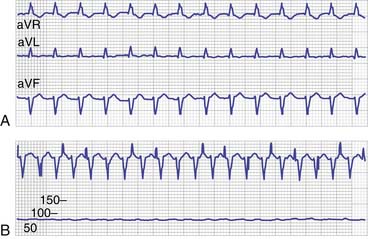
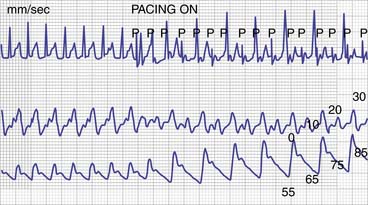
For bradycardias, the surface ECG usually is sufficient to characterize the arrhythmia and differentiate between an abnormality in sinus nodal function and AV block, based on the ratio of atrial-to-ventricular rate. The diagnosis of tachycardias may not be feasible from the surface ECG alone. Nevertheless, a combination of surface ECG and simple diagnostic maneuvers, sometimes coupled with direct recording of atrial activation, should allow accurate determination of most tachycardias. As with bradycardias, the surface ECG should be inspected for the ventricular rate and regularity, QRS duration and morphology, and atrial-to-ventricular relationship. Too often the apparent atrial-to-ventricular relationship is not clearly reflected on the surface ECG, and direct atrial recording, either with temporary atrial pacing wires or an esophageal ECG, is necessary to facilitate the diagnosis (Figure 28-6).
Bradycardias
In the absence of AV block, bradycardias are characterized by the origin of the initiating impulse as sinus, atrial, junctional, or ventricular. It is important to distinguish junctional or ventricular bradycardia from sinus bradycardia with an underlying junctional or ventricular escape, respectively. Terms such as “nodal rhythm” and “dissociated” are imprecise and demand further characterization. When the atrial rate exceeds the ventricular rate, second-degree or third-degree AV block is present. In complete AV block, the resultant escape rhythm usually is regular; in second-degree AV block, the ventricular intervals vary (see Figure 28-1). Occasionally, sinus node disease and complete AV block coexist, so it is important in the setting of a slow atrial rate to note “sinus capture” complexes when appropriately timed P waves conduct to the ventricle. When atrial pacing is feasible (as in patients with recent cardiac surgery), temporary atrial pacing can be used to demonstrate normal AV conduction, and the maximum rate at which 1:1 conduction can be maintained can be easily determined and followed serially.
Extrasystoles
Isolated premature QRS complexes with prolonged QRS duration may represent either ventricular extrasystoles or aberrantly conducted atrial extrasystoles. Distinguishing the two may be difficult from a single rhythm strip. Premature P waves often may be obscured in a particular lead, or the ventricular extrasystole morphology may appear similar to the sinus QRS in one lead (but totally dissimilar in another). The ECG features favoring ventricular extrasystoles over aberrantly conducted atrial extrasystoles include (1) wide QRS morphology, (2) a full compensatory pause, (3) presence of fusion beats, and (4) absence of a discernible premature P wave. In the setting of ventricular preexcitation, variable fusion can occur as a result of exaggerated preexcitation with premature atrial depolarizations. As noted earlier, ventricular extrasystoles usually are followed by a full compensatory pause because the sinus node is not reset by the ventricular depolarization. However, an atrial extrasystole may sometimes fail to reset the sinus node (because of entrance block) or a ventricular extrasystole may occasionally reset the sinus node because of retrograde (VA) conduction. The simultaneous occurrence of both narrow QRS and wide QRS extrasystoles usually favors normally and aberrantly conducted atrial extrasystoles, particularly when the QRS width varies with the degree of prematurity (excluding fusion complexes).
Tachycardias with Normal QRS
By definition, all tachycardias with normal QRS represent either sinus tachycardia or a form of SVT. It should be noted that the terms supraventricular tachycardia, paroxysmal supraventricular tachycardia, and paroxysmal atrial tachycardia often are used in reference to tachycardias with normal QRS, a regular rate in excess of 200 bpm, and no readily discernible P waves. In otherwise healthy infants, children, and adolescents, these features usually result from either AV reentrant tachycardia or AVNRT (Figure 28-7). Further distinction between these two mechanisms has little impact on acute management. However, in the ICU setting, primary atrial tachycardias (including sinus tachycardia) and junctional tachycardias also must be considered (particularly following cardiac surgery). Abnormal P-wave morphology (determined by 12-lead ECG), PR interval greater than 50% of the RR interval, or completely obscured P waves favor a nonsinus mechanism. Finally, the QRS duration may appear normal by adult standards but be significantly prolonged for age.
In young patients, intraatrial reentry, atrial flutter, and atrial fibrillation usually are seen following surgical treatment for congenital heart defects involving the atrium (atrial septal defects, atrial repair of transposition of the great arteries, or the Fontan operation).15 The sawtooth pattern typical of atrial flutter may be absent in these patients, and the term intraatrial reentrant tachycardia (IART) may be more appropriate when discrete P waves are present. Because the atrial rate often is relatively slow in comparison with “typical” atrial flutter, a high index of suspicion is required. In some cases, the atrial rate is slow enough that consistent 1:1 conduction (with discrete P waves) further obscures the diagnosis by simulating sinus tachycardia. Similarly, with 2:1 conduction, alternate P waves may be obscured by the T wave, giving the impression of sinus rhythm.
Distinguishing sinus tachycardia from various types of SVT may be difficult. The appropriateness and variation of the rate (or lack thereof) may be particularly helpful in differentiating sinus from nonsinus tachycardias. Observing the heart rate response to interventions such as volume expansion, analgesia, antipyretic agents, and catecholamine infusions often is helpful. Depending on the pattern of atrial activation, P waves may even simulate a normal sinus P-wave morphology during primary atrial tachycardias. In other cases, AV conduction may appear to be 1:1 on the surface electrocardiogram when, in fact, a second P wave is obscured by the QRS complex or T wave. Direct atrial recordings using transesophageal electrocardiography or temporary epicardial atrial pacing wires usually facilitate the diagnosis (see Figure 28-6, B). Vagal maneuvers or administration of adenosine to interrupt AV conduction transiently often helps characterize the true AV relationship and determine whether the AV node participates in the tachycardia mechanism.
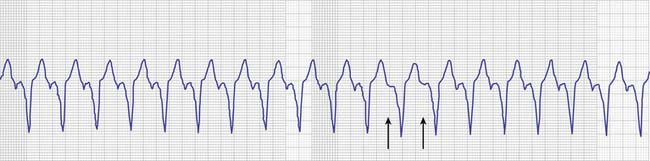
Tachycardias with Prolonged QRS
Generally, tachycardias with prolonged QRS should be presumed to be ventricular tachycardias until or unless evidence of an alternative diagnosis is demonstrated. VA dissociation, the hallmark ECG feature of ventricular tachycardia, may not be seen in childhood because of rapid retrograde conduction over the AV node (see Figure 28-4). The distinction between ventricular tachycardia and SVT with aberrant conduction can be difficult and may require invasive electrophysiologic study. Prolonged attempts to differentiate the two at the bedside by noninvasive means often are fruitless and may delay treatment. The wrong conclusion may prompt inappropriate and potentially dangerous therapeutic maneuvers. In the acute setting, treatment based on a presumed diagnosis of ventricular tachycardia is rarely deleterious, even when the mechanism subsequently proves to be supraventricular. However, an erroneous presumption of “SVT with aberrant conduction” may have disastrous consequences. When feasible, a full 12-lead ECG may aid in the diagnosis, particularly when a baseline ECG in normal rhythm is available for comparison. Apparent hemodynamic stability should not be mistaken for evidence of SVT rather than ventricular tachycardia, whether in an otherwise healthy child or in a patient with known cardiac disease.
Monitoring of Atrial Depolarization
Direct recording of atrial activity is necessary when the AV relationship cannot be determined from the surface ECG or otherwise inferred by the means described. Patients recovering from cardiac surgery frequently have temporary atrial epicardial pacing wires in place that can be used to record atrial electrograms directly while simultaneously recording the surface ECG (see Figure 28-6, B). Attachment of the atrial wires to a unipolar precordial lead (“V lead”) on the monitor is an easy way to observe atrial activation. Otherwise, atrial activity can be readily recorded with a bipolar esophageal catheter inserted in the esophagus behind the left atrium.
Diagnostic Uses of Adenosine
Although most widely used as an acute therapy for terminating SVT that involves the AV node, adenosine administration also may yield important diagnostic clues to the underlying arrhythmia mechanism.16 By producing transient block in the AV node during tachycardia, it often is possible to distinguish AV reentrant tachycardias and AVNRTs (either of which should terminate) from atrial tachycardias and ventricular tachycardias. However, adenosine’s effects are not confined to the AV node. Ectopic (automatic) atrial and junctional tachycardias, intraatrial reentry, and certain ventricular tachycardias also may terminate with adenosine. Extreme caution should be taken when administering adenosine during wide QRS tachycardia. Adenosine produces vasodilatation, which theoretically can result in hemodynamic deterioration and tachycardia acceleration, or even fibrillation, if tachycardia fails to terminate. Ventricular fibrillation has been rarely observed when adenosine is administered in the setting of WPW syndrome, probably as a result of atrial fibrillation that then is conducted rapidly to the ventricles. Prompt defibrillation should always be readily at hand when administering adenosine for diagnostic or therapeutic purposes.
Treatment of Rhythm Disturbances
A second important consideration in critically ill patients, particularly those undergoing cardiac surgery, is to favor therapies that maintain appropriate AV synchrony. In the setting of marginal hemodynamics, an otherwise acceptable ventricular rate during arrhythmias such as atrial tachycardias and fibrillation, junctional tachycardia, or AV block may further compromise cardiac output as a result of loss of AV synchrony (see Figure 28-8).
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree