W1 Difficult Airway Management for Intensivists
 Supraglottic Airway Placement: Before Procedure
Supraglottic Airway Placement: Before Procedure
Indications
Equipment
 After Procedure
After Procedure
Suggested Reading
 Bougie-Assisted Intubation: Before Procedure
Bougie-Assisted Intubation: Before Procedure
Indications
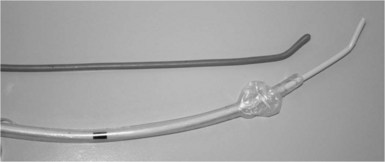
Equipment
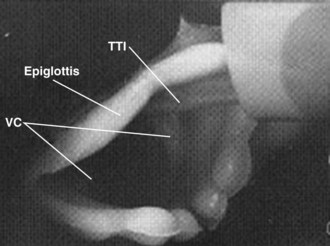
 Anatomy
Anatomy
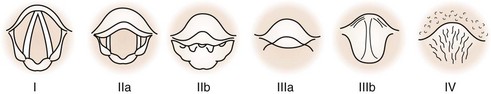
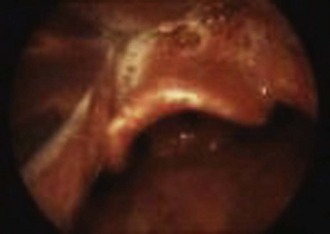
Though the bougie is capable of assisting intubation in nearly all airway situations except when “no view” is possible, it is most commonly used as an adjunct with Grade IIb, IIIa, and IIIb laryngeal views. Even when the laryngoscopy reveals a full view (grade I), the bougie may be useful when the hypopharyngeal opening is narrow (OSA, obesity, swelling) and passing the ETT may actually obstruct the view of the glottic opening. In this case, the narrower, more colorful tracheal tube introducer can be passed into the trachea with little visual obstruction taking place. Conversely, the floppy epiglottis is a challenge that may be technically difficult with many different airway adjuncts. The bougie may either be used to elevate the floppy epiglottis or be maneuvered around by virtue of the Coude tip. Though useful, the success rate is often less than 50%, and other alternatives may be needed (intubating laryngeal mask airway [ILMA], videolaryngoscope [VL], fiberoptic bronchoscope [FOB]) (Figure W1-7).
 Procedure
Procedure
 After Procedure
After Procedure
Postprocedure Care
Complications
Suggested Reading
 Use of the Intubating Model of the LMA for Emergency Airway Rescue (Fastrach) ILMA: Before Procedure
Use of the Intubating Model of the LMA for Emergency Airway Rescue (Fastrach) ILMA: Before Procedure
 Anatomy
Anatomy
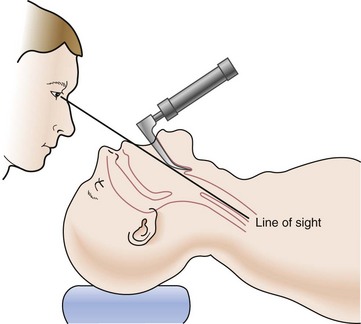
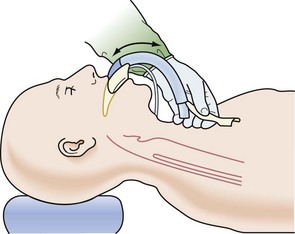
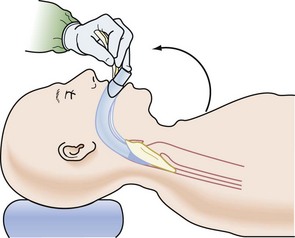
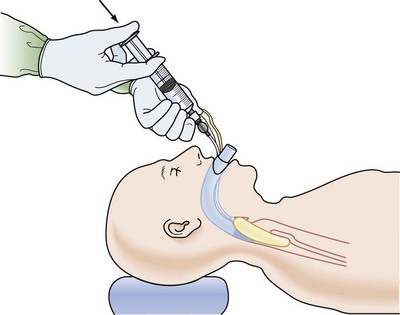
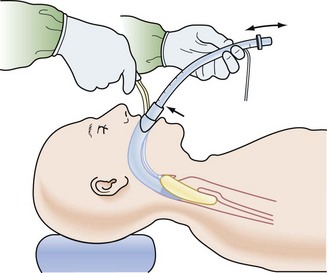
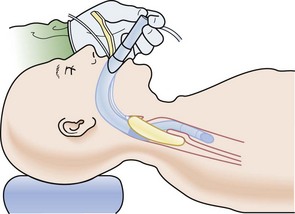
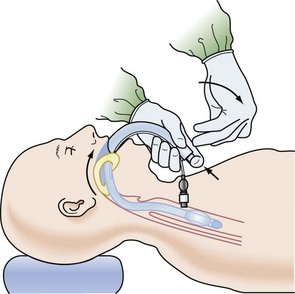
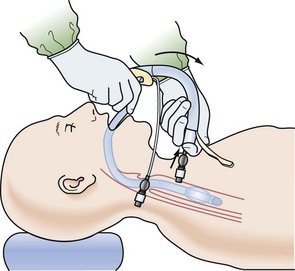
In general, placement of the ILMA can be performed in the exaggerated “sniff” position or the other extreme, a neutral cervical spine. The ILMA is lubricated and then passed along the roof of the mouth across the hard to soft palate, encouraging smooth advancement along the posterior throat so as to minimize getting hung up on the epiglottis or causing its downfolding. The distal tip of the ILMA typically comes to lie with its distal tip in the cricopharyngeal region. Unfortunately, the cuff end may buckle over on itself, come to lie over the glottic opening, or be displaced in a contorted position that impedes effective ventilation and oxygenation (Figures W1-9 through W1-16).
 Procedure
Procedure
 After Procedure
After Procedure
Postprocedure Care
 Outcomes and Evidence
Outcomes and Evidence
Suggested Reading
 Retrograde Wire Intubation: Before Procedure
Retrograde Wire Intubation: Before Procedure
Indications
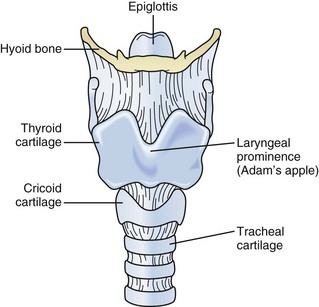
 Anatomy
Anatomy
The cricothyroid membrane is located between the superior thyroid cartilage and the inferior cricoid ring. The cricothyroid membrane is located just 1.5 to 2 cm below the vocal cords, so care must be practiced when advancing a needle caudad, as the underside of the vocal cords could be impaled. Passing the ETT over the wire or obturator/wire may be met with resistance at the 16- to 17-cm depth, as the ETT tip may impinge on the vocal cords or arytenoids. This is the inherent danger of passing the ETT blindly over the wire or obturator/wire assembly. The location of the distal tip (having met resistance) may or may not be at the position below the vocal cords. This is the challenge of the retrograde wire method; knowing the location of the ETT tip is unknown when the decision is made to remove the wire. If the ETT tip is erroneously positioned above the glottis, then the access to the airway is denied with wire removal; hence, the advantage of using the FOB as an intubation guide (Figure W1-17).
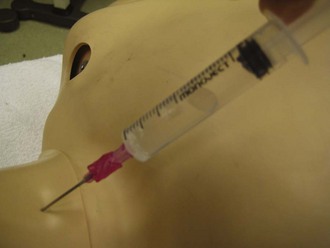
 Procedure
Procedure
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree