28 Dental Emergencies
• Adults have 32 permanent teeth. Children have 20 primary teeth.
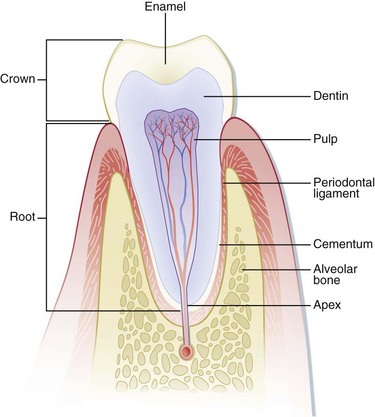
• A tooth consists of (1) the enamel, which is the outermost, hard protective layer; (2) the underlying elastic and porous dentin, which cushions the tooth during mastication and carries nutrients from the pulp to the enamel; (3) the pulp, which contains the neurovascular supply of the tooth; and (4) the cementum and the periodontal ligament, which anchor the tooth into alveolar bone.
• Use of bupivacaine in the form of a dental nerve block is an effective means of providing relief from severe odontalgia. A dental block should also be performed before manipulation of any significantly traumatized tooth.
• Radiographs are not usually necessary for most dental complaints, but they can be useful when one must search for a tooth fragment, an avulsed or intruded tooth, or a mandibular fracture.
• Any exposed dentin or pulp of an acutely fractured tooth should be covered. The covering aids in pain control and may prevent the need for a root canal.
• Subluxated or luxated teeth should be splinted if significantly loosened to prevent aspiration and maximize potential viability.
• Avulsed teeth should be placed in a storage medium immediately by emergency medical services or emergency department personnel to maximize potential viability.
Epidemiology
The incidence of dental complaints in emergency departments (EDs) appears to be rising, which may reflect the increasing use of EDs as primary care facilities.1 Injuries involving the younger population are most often secondary to falls or accidents, whereas those in older age groups are most often secondary to motor vehicle accidents, falls, or assaults.2 Traumatic dental injuries usually involve the permanent anterior dentition, but adult dentoalveolar injuries are frequently associated with fractures of the mandible and face. Patients who have fractures of both the mandibular condyle and body are more likely to have related tooth injury than are patients with either isolated body or condylar fractures.2
Structure and Function
The Stomatognathic System
The muscles of mastication are responsible for opening and closing the mouth and are those most frequently associated with temporomandibular disorders (TMDs). The clinician should be knowledgeable about the position of the muscles to perform an examination properly and to recognize the origin of certain painful conditions. The muscles that close the mouth are those most often associated with TMDs; these muscles are the masseter, the temporalis, and the medial pterygoid (Fig. 28.1).3 Contraction of this group of muscles bilaterally serves to move the condyle superiorly and posteriorly, which causes the mouth to close. The muscles that open the mouth are the anterior digastric, posterior digastric, mylohyoid, geniohyoid, and infrahyoid muscles (Fig. 28.2). The lateral pterygoid muscles are responsible for anterior translation and lateral movement of the mandible (Fig. 28.3). Unilateral contraction causes lateral movement away from the side of the muscle contraction, whereas bilateral contraction causes protrusion of the mandible.
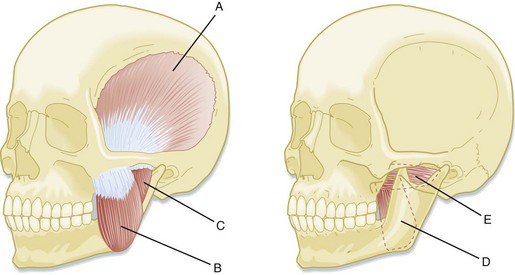
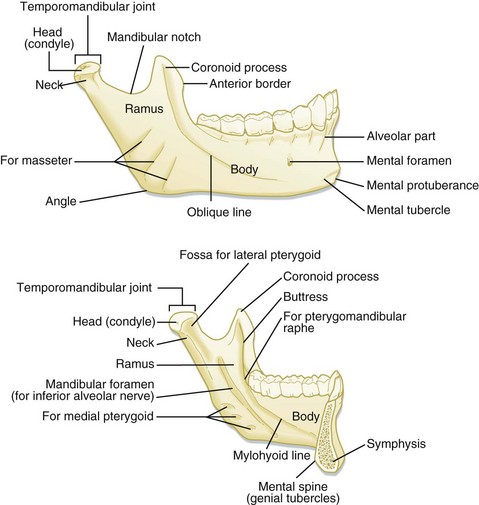
Fig. 28.1 Muscles responsible for closing and excursive mandibular movements.
(From King R, Montgomery M, Redding S, editors. Oral-facial emergencies—diagnosis and management. Portland, OR: JBK Publishing; 1994.)
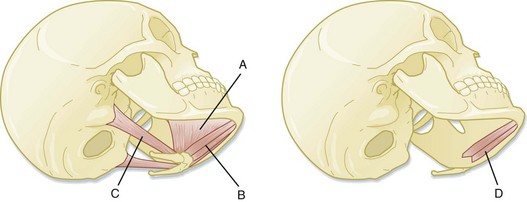
Fig. 28.2 Muscles responsible for mandibular opening.
(From King R, Montgomery M, Redding S, editors. Oral-facial emergencies—diagnosis and management. Portland, OR: JBK Publishing; 1994.)
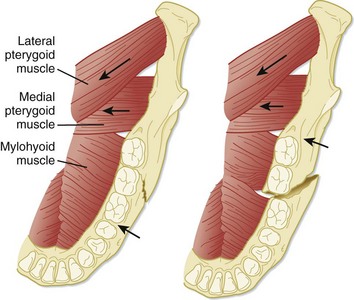
Fig. 28.3 Axial view of the floor of the mandible.
(From Eisele D, McQuone S, editors. Emergencies of the head and neck. St. Louis: Mosby; 2000.)
Each side of the mandible consists of the horizontal body and ascending ramus, which are connected by the angle. The bodies of the mandible are connected by the symphysis in the midline. The ascending ramus gives rise to two processes superiorly, the condylar process and the coronoid process (Fig. 28.4). The mandibular condyle, along with the mandibular fossa and the articular eminence of the temporal bone, make up the temporomandibular joint (TMJ). The TMJ provides both hinge and gliding actions. Between the mandibular condyle and the articular eminence lies the meniscus, a fibrous collagen disk. A ligamentous joint capsule surrounds the TMJ and serves to limit condylar movement. TMJ pain may be caused by a number of conditions, both traumatic and nontraumatic.
Teeth
Names
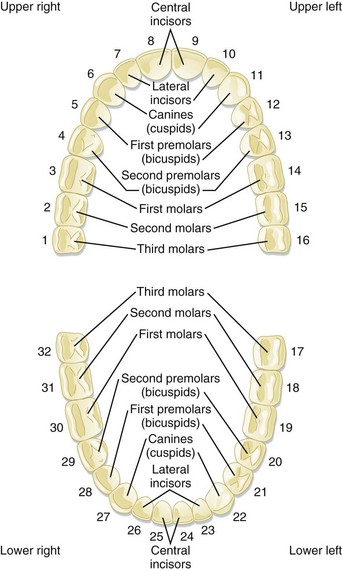
The adult dentition normally consists of 32 teeth, of which 8 are incisors, 4 are canines, 8 are premolars, and 12 are molars. From the midline to the back of the mouth on each side are a central incisor, a lateral incisor, a canine (eye tooth), two premolars, and three molars, the last of which is the troublesome wisdom tooth (Fig. 28.5).
Identification of Teeth
The primary teeth, or “baby teeth,” are also best described by determining which tooth is involved, not by its official classification. A full complement of primary teeth consists of 20 teeth: 8 incisors, 4 canines, and 8 molars. The earliest primary teeth to erupt are the central incisors, usually at 4 to 8 months. Children usually have a full complement of teeth by the time that they are 3 years old (Table 28.1).
| TOOTH DESIGNATION | NAME OF TOOTH | APPEARANCE IN THE MOUTH |
|---|---|---|
| Baby (Primary) Teeth | ||
| A | Central incisor | 4-14 mo |
| B | Lateral incisor | 8-18 mo |
| C | Canine tooth | 14-24 mo |
| D | First molar | 10-20 mo |
| E | Second molar | 20-36 mo |
| Adult (Permanent) Teeth | ||
| 1 | Central incisor | 5-9 yr |
| 2 | Lateral incisor | 6-10 yr |
| 3 | Canine tooth |  yr yr |
| 4 | First premolar (bicuspid) | 9-14 yr |
| 5 | Second premolar (bicuspid) | 10-15 yr |
| 6 | First molar (6-yr molar) | 5-9 yr |
| 7 | Second molar (12-yr molar) | 10-15 yr |
| 8 | Third molar (wisdom tooth) | 17-25 yr |
Anatomy
A tooth consists of the central pulp, the dentin, and the enamel (Fig. 28.6). The pulp contains the neurovascular supply of the tooth, which delivers nutrients to the dentin, a microporous system of microtubules. The dentin makes up the majority of the tooth and cushions it during mastication. The white, visible portion of a tooth, the enamel, is the hardest part of the body. A tooth may also be described in terms of its coronal portion (crown) or its root. The crown is covered in enamel, and the root is anchored in alveolar bone by the periodontal ligament and cementum.
The following terminology is used to describe the different anatomic surfaces of the tooth:
Facial: The part of the tooth that faces the opening of the mouth. This surface is visible when someone smiles. This is a general term applicable to all the teeth.
Labial: The facial surface of the incisors and canines.
Buccal: The facial surface of the premolars and molars.
Oral: The part of the tooth that faces the tongue or palate. This is a general term applicable to all the teeth.
Lingual: Toward the tongue; the oral surface of the mandibular teeth.
Palatal: Toward the palate; the oral surface of the maxillary teeth.
Approximal/interproximal: The contacting surfaces between two adjacent teeth.
Mesial: The interproximal surface facing anteriorly or closest to the midline.
Distal: The interproximal surface facing posteriorly or away from the midline.
Occlusal: Biting or chewing surface of the premolars and molars.
Incisal: Biting or chewing surface of the incisors and canines.
Apical: Toward the tip of the root of the tooth.
Coronal: Toward the crown or the biting surface of the tooth.
The Periodontium
The periodontium is the attachment apparatus. It consists of the gingival and periodontal subunits, which maintain the integrity of the entire dentoalveolar unit. The gingival subunit consists of gingival tissue and junctional epithelium. The periodontal subunit consists of the periodontal ligament, the alveolar bone, and the cementum of the root of the tooth (see Fig. 28.6). The gingival sulcus is the space between the attached gingiva and the tooth. The mucobuccal fold is that area of mucosa where the attached gingiva gives rise to the looser buccal mucosa. The mucobuccal fold is the area penetrated when most dental nerve blocks are performed.
Presenting Signs and Symptoms
1. When did the incident occur? This is important in the evaluation of avulsed permanent teeth because the decision to reimplant a tooth is based largely on the duration of the avulsion.
2. Were any teeth found at the scene?
3. Did the patient have any symptoms suggestive of tooth aspiration, such as coughing or choking at the scene?
4. Has the patient been using alcohol or any other sedatives or recreational drugs that may have made aspiration more likely?
5. Does the patient have amnesia, which may suggest loss of consciousness?
6. Does the patient complain of pain? Do the teeth feel as though they are touching normally? Is the pain associated with occlusion? Mandibular fractures typically worsen with jaw movement, and patients complain that their bite is off. Pain from TMJ injuries is often referred to the ear. Fractured teeth frequently hurt more with the inspiration of air or contact with cold substances. Luxated or subluxated teeth hurt during mastication or chewing.
7. Did the patient take any over-the-counter analgesics or apply any substances to decrease the pain? Over-the-counter topical anesthetics can cause sterile abscesses when applied directly to the pulp.3
8. Is the tooth a permanent or a primary tooth? Avulsed primary teeth are managed differently from avulsed permanent teeth.
9. Does the patient have a history of bleeding disorders or allergies?
Additional historical information must be obtained if the complaint does not involve trauma:
1. Has the patient had any recent dental work? Dry sockets, for example, occur several days after a tooth has been extracted.
2. Does the patient have a history of poor dentition or multiple caries?
3. Is the patient having difficulty opening the mouth, which suggests a TMJ problem?
4. Has the patient had any difficulty swallowing? Has a change in voice or any shortness of breath occurred? Has any swelling developed? These symptoms suggest a possible deep space infection or hematoma.
5. Is the patient immunocompromised? Deep space infections spread rapidly to the mediastinum and cavernous sinus in an immunocompromised patient.
6. Does the patient have a coagulopathy secondary to aspirin, warfarin, or other anticoagulants or symptoms or a history suggestive of a bleeding disorder?
7. Was the time course of the problem insidious or rapid? Has the patient had symptoms of infection, such as fever, chills, or vomiting?
8. Does the patient have a history of rheumatic fever or valvular disease, such as mitral valve prolapse?4 Does the patient have artificial joints, valves, or shunts? These may predispose to endocarditis or infection of the implant or shunt if dental infection is present.
Differential Diagnosis
Nontraumatic dental emergencies usually result from poor oral hygiene, recent dental instrumentation, or infection. Uncomplicated tooth pain (odontalgia) is often pulpitis, and further diagnostic testing is not necessary in the ED. The other consideration is periodontal or pulpal infection or abscess. Nonodontogenic sources may cause referred pain to the dentition. Referred pain from the sinuses or the TMJ must also be considered, especially for pain that cannot be localized (Table 28.2). A patient who has recently undergone dental instrumentation or extraction may be seen in the ED with dry socket, hematoma, or hemorrhage.
Table 28.2 Differential Diagnosis of Orofacial Pain
| Odontogenic pain | |
| Periodontal pathology | |
| Orofacial trauma | |
| Infection | |
| Malignancies |