Defibrillation: Practice
Vincent N. Mosesso Jr.
Cheryl Rickens
Defibrillation has a pivotal place in the management of pulseless cardiac arrest. Delivering an electrical shock to the heart is the sine qua non for the reversal of ventricular fibrillation (VF) and is often necessary for unstable ventricular tachycardia. Defibrillation remains the only therapy that directly reverses VF. However, there is an evolving understanding of the importance of adjunctive therapies to improve the myocardial metabolic state and the time-sensitive nature of defibrillation.
Defibrillation (delivery of an electric shock through the heart) is necessary for eradication of the lethal arrhythmia VF.
In general, the earlier defibrillation occurs, the higher the likelihood of survival from VF.
In cases of prolonged VF, a brief period of cardiopulmonary resuscitation (CPR) improves the likelihood of successful defibrillation.
Defibrillators (both manual and automated) and providers must be maintained in a state of readiness.
Introduction
Defibrillation has a pivotal place in the management of pulseless cardiac arrest. Delivering an electrical shock to the heart is the sine qua non for the reversal of VF and is often necessary for unstable ventricular tachycardia. While “defibrillation” literally means “the reversal or absence of fibrillation,” the term is commonly used to refer to the delivery of an electric shock in an attempt to terminate the fatal arrhythmia. Electrical defibrillation is intended to eradicate all active electrical current by depolarizing a critical mass of myocardium. Defibrillation literally stuns the heart, with the hope that a normal pacemaker site will then be able to regain control of the cardiac conducting system. Defibrillation remains the only therapy that directly reverses VF, although we are gaining an evolving understanding of the importance of adjunctive therapies to improve the myocardial metabolic state at the time of defibrillation. So while the concept of early defibrillation is still an important principle of management, guidelines now and in the future will address the timing of defibrillation for different patient populations and the integration of CPR and other therapies with defibrillatory shocks.
The Concept of “Early” Defibrillation
Early defibrillation is critical to survival from sudden cardiac arrest (SCA) for several reasons:
The most frequent initial rhythm in witnessed SCA is ventricular fibrillation.
The treatment for VF is electrical defibrillation.
The probability of successful defibrillation diminishes rapidly over time.
VF tends to deteriorate to asystole within a few minutes.1
Several studies have documented the effects of time to defibrillation and the effects of bystander CPR on survival from SCA. For every minute that passes between collapse and defibrillation, survival rates from witnessed VF SCA decrease 7% to 10% if no CPR is provided.1 When bystander CPR is provided, the decrease in survival rates is more gradual and averages 3% to 4% per minute from collapse to defibrillation.1,2 CPR can double1,2,3 or triple4 survival from witnessed SCA at any interval to defibrillation.
If bystanders provide immediate CPR, many adults in VF can survive with intact neurologic function, especially if defibrillation is performed within about 5 minutes after SCA.5,6 CPR prolongs the window of time during which defibrillation will be effective7,8,9 and provides a small amount of blood flow that may maintain some oxygen and substrate delivery to the heart and brain.10 CPR alone, however, is unlikely to eliminate VF and restore a perfusing rhythm.
Nearly all neurologically intact survivors, who in some studies number more than 90% of survivors, have a ventricular tachyarrhythmia that was treated by early defibrillation.10,11,12,13,14,15 In a subgroup of SCD patients, it appears from studies in which Holter monitors were used that a ventricular tachyarrhythmia is the initial rhythm disturbance in up to 85% of persons with sudden, out-of-hospital, nontraumatic cardiac arrest.16 These studies are biased somewhat because they examined patients with underlying heart disease; the majority took antiarrhythmic drugs at the time of the study. Ventricular tachycardia is frequently short-lived and converts rapidly to VF, from
which the only hope for successful resuscitation lies in early defibrillation. The proportion of patients with VF also declines with each passing minute as more and more patients deteriorate into asystole, from which successful resuscitation is extremely unlikely. Some 4 to 8 minutes after collapse, approximately 50% of patients are still in VF.1,2,17 In addition, the incidence of VF as the initial presenting arrhythmia in out-of-hospital cardiac arrest is declining. Patients without VF as the cause for their arrest have a lower probability of survival, potentially due to a different pathophysiology of cardiac arrest and the ineffectiveness (or lack) of current resuscitation techniques.
which the only hope for successful resuscitation lies in early defibrillation. The proportion of patients with VF also declines with each passing minute as more and more patients deteriorate into asystole, from which successful resuscitation is extremely unlikely. Some 4 to 8 minutes after collapse, approximately 50% of patients are still in VF.1,2,17 In addition, the incidence of VF as the initial presenting arrhythmia in out-of-hospital cardiac arrest is declining. Patients without VF as the cause for their arrest have a lower probability of survival, potentially due to a different pathophysiology of cardiac arrest and the ineffectiveness (or lack) of current resuscitation techniques.
Survival rates from cardiac arrest can be remarkably high if the event is witnessed. For example, when people in supervised cardiac rehabilitation programs suffer a witnessed cardiac arrest, defibrillation is usually performed within minutes. In studies of cardiac arrest in this setting, 90 of 101 victims (89%) were resuscitated.18,19,20 No other studies with a defined out-of-hospital population have observed survival rates this high. Adult patients in VF may survive neurologically intact even if defibrillation is performed as late as 6 to 10 minutes after arrest. When defibrillation is delayed, the critical factor determining survival is whether on-site bystanders perform effective CPR while waiting for the defibrillator.3,6,20,21,22
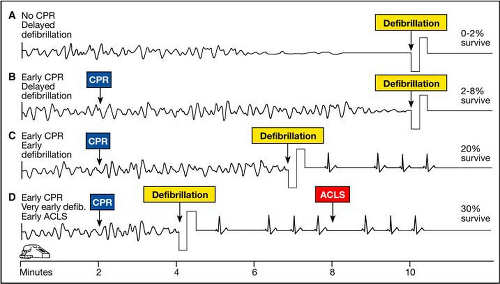
The interaction between early defibrillation and early CPR is displayed graphically in Fig. 13-1. This figure illustrates the probability of survival in relation to the intervals from collapse to first shock and from collapse to start of CPR. It clearly illustrates that the sooner CPR is started and the sooner the defibrillator arrives, the better the outcome. It also shows how starting CPR early changes the slope of the defibrillation survival curve and “buys time” for the defibrillator to arrive.
Development of Early Defibrillation Programs
More than 20 years ago, several communities with no advanced life support (ALS) services evaluated adding prehospital defibrillation. Invariably these “before and after” studies showed improved survival rates for cardiac arrest patients when the community added any type of program that resulted in earlier defibrillation (Table 13-1). Impressive results were reported from early studies in King County, Washington, where the odds ratio for improved survival (comparing survival after versus before the addition of an early defibrillation program) was 3.7,23 and rural Iowa, where the odds ratio was 6.3.24 Evidence continued to accumulate during the 1980s; investigators reported
positive odds ratios of 4.3 for improved survival in rural communities of southeastern Minnesota,25 5.0 in northeastern Minnesota,26,27 and 2.8 in Wisconsin.
positive odds ratios of 4.3 for improved survival in rural communities of southeastern Minnesota,25 5.0 in northeastern Minnesota,26,27 and 2.8 in Wisconsin.
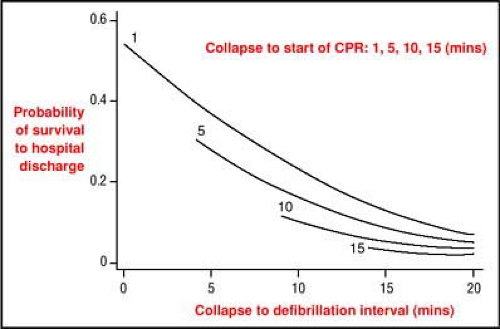 Figure 13-1 • Effect of collapse-to-CPR interval and collapse-to-defibrillation interval on survival to hospital discharge. The graph displays the probability of survival to hospital discharge in relation to four intervals from collapse to start of CPR (1, 5, 10, and 15 minutes) and collapse to defibrillation (5, 10, 15, and 20 minutes). To determine the probability of survival for an individual patient, identify the curve indicating the interval from collapse to CPR and then identify the point on that curve that corresponds to the interval from collapse to defibrillation (see horizontal axis). The probability of survival is then indicated on the vertical axis. Based on data from King County, Washington (N = 1667 witnessed VT/VF arrests),1 and Tucson, Arizona (N = 205 witnessed VT/VF arrests).2 (Adapted from Valenzuela TD, Roe DJ, Cretin S, et al. Estimating effectiveness of cardiac arrest interventions: a logistic regression survival model. Circulation 1997; 96[10]:3308–3313, with permission.) |
Table 13-1 • Effectiveness of Early Defibrillation Programs by Community | ||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||
Table 13-2 • Survival to Hospital Discharge From Cardiac Arrest by System Type: Data From 29 Locationsa | ||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||
When the survival rates were examined not by community but by the type of system deployed across larger geographic areas, that same pattern emerged: the system organized to get the defibrillator there the fastest—independent of the arrival of personnel to perform endotracheal intubation and provide IV medications—achieved better survival rates (Table 13-2).
Figure 13-2 illustrates this same concept in a different way. The figure compares survival among victims who receive different interventions (“links in the chain”) at different intervals.
In the earliest programs, EMTs with additional training used a manual defibrillator. Subsequently, personnel at the
first-responder level, such as firefighters, were trained and equipped with automated external defibrillators (AEDs). In 1989, a study of AED use by firefighter first responders in King County, Washington, found that this strategy improved the calculated survival among patients in VF from 19% to 30%.31 This study catalyzed the deployment of AEDs among firefighter first responders in many other parts of the country and served to establish the legitimacy and value of this technology.
first-responder level, such as firefighters, were trained and equipped with automated external defibrillators (AEDs). In 1989, a study of AED use by firefighter first responders in King County, Washington, found that this strategy improved the calculated survival among patients in VF from 19% to 30%.31 This study catalyzed the deployment of AEDs among firefighter first responders in many other parts of the country and served to establish the legitimacy and value of this technology.
While firefighters are often available to serve as first responders in urban areas, most suburban communities do not have this resource. In these communities, police officers often fulfill this role. In the 1990s, studies in two locations demonstrated the feasibility of police providing early defibrillation. A study from Rochester, Minnesota, reported a remarkable survival rate of 45% after police were equipped with AEDs (shock was provided by EMS or police officers depending on who arrived first).32 In suburbs of Pittsburgh, Pennsylvania, survival was improved nearly 10-fold if police performed defibrillation when they arrived before EMS rather than waiting for EMS personnel (survival to hospital discharge was 26% versus 3%, P = 0.027).33 This study also found that police officers were able to use the devices effectively with minimal errors and that the devices rarely malfunctioned.34 A national survey of law enforcement agencies (LEAs) found that 80% routinely respond to medical emergencies and that 39% of these deploy AEDs.35 This is a significant increase compared with a prior survey in the late 1990s, which found that only about 3% of LEAs were equipped with AEDs.36
For optimal effectiveness, defibrillation should be provided within about 5 minutes of collapse, a narrow therapeutic window that has been termed “the electrical phase of cardiac arrest”37 (see sidebar). Unfortunately, first responders and EMS personnel usually cannot respond to the location of a cardiac arrest victim rapidly enough to provide defibrillation within this time frame. That goal can be achieved on a consistent basis only through the availability of on-site defibrillators and their use by willing on-site rescuers. Several programs and studies have evaluated this concept, commonly referred to as public-access defibrillation (PAD).
Optimal Timing for Immediate Defibrillation
The Three-Phase Model of Cardiac Arrest and New Recommendations
Successful Defibrillation from the Metabolic Perspective
Successful defibrillation depends on the electrical and metabolic state of the myocardium, the amount of myocardial damage that occurs during hypoxic arrest, the prior functional state of the heart, and the cause of VF. From a metabolic perspective VF depletes more of the cardiac energy stores—adenosine triphosphate (ATP)—per minute than does normal sinus rhythm. Prolonged VF will exhaust the energy stores of ATP in the myocardium, particularly in the cardiac pacemaker cells. The longer VF persists, the greater the myocardial deterioration as energy stores become exhausted. In a heart stunned into electrical silence by a defibrillatory shock, no spontaneous contractions will resume if the fibrillating myocardium has consumed all its energy stores. When ATP is depleted and cellular functions are disrupted, shocks are more likely to convert VF to asystole than to a spontaneous rhythm because no “fuel” remains to support spontaneous depolarization in the pacemaker tissues or the contracting myocardium. With depleted reserves of energy, any postshock asystole or agonal rhythms will be permanent, not temporary.
Delayed Defibrillation
For this reason, VF of short duration is much more likely to respond to a shock delivered soon after VF starts. An important objective for resuscitation and any effort to improve outcome is to shorten the interval between the onset of VF and the first shock. In Emergency Cardiovascular Care (ECC) Guidelines 2000, the American Heart Association (AHA) recommended that all patients who have a VF arrest out of hospital receive shocks in <5 minutes; a goal for patients who have an in-hospital VF arrest is <3minutes.
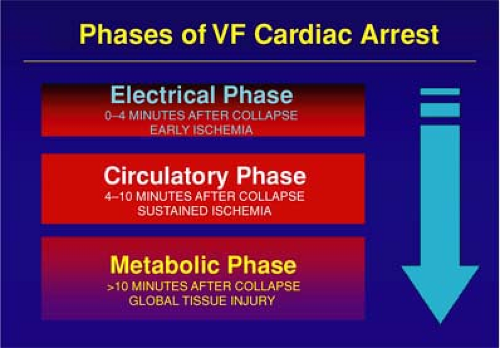
Cobb et al.6 noted, however, that as more Seattle first responders were equipped with AEDs, survival rates from SCA unexpectedly fell. The investigators attributed this decline to a reduced emphasis on CPR when defibrillation is delayed, and there is growing evidence to support this view. When VF causes cardiac arrest, three general phases of arrest occur: an electrical phase, a circulatory phase, and a metabolic phase (Figure).37 Whether a shock is delivered immediately (during the early electrical phase) or after a brief period of CPR, later during the circulatory phase, may be one explanation for this observation. During the circulatory phase, a brief period of CPR may “prime the pump” and provide a small but important period of oxygen and energy substrate.
Early Defibrillation Programs
Casinos
An innovative program implemented in casinos demonstrated the benefit of AED use by on-site responders. Security personnel were trained to use AEDs, which were deployed throughout the premises close enough to facilitate their use within 3 minutes of collapse. The average time interval from collapse to shock was 4.4 ± 2.9 minutes. The survival rate was 74% among patients shocked within 3 minutes and 49% among those shocked after more than 3 minutes.38
Commercial Aircraft
One venue where the need for defibrillation by on-site personnel was quite obvious was commercial aircraft. Qantas Airlines pioneered this concept by placing AEDs on their planes and training flight attendants in CPR and AED use.39 American Airlines reported that over a 2-year period, 200 (191 on aircraft and 9 in terminals) arrests occurred.40 The Federal Aviation Administration has now mandated that all aircraft staffed with at least one flight attendant must be equipped with an AED.
Another early PAD program was implemented at the Chicago airports. AEDs were deployed so that they were within a 90-second walk of each other. Over 3,000 airport workers were trained in CPR and AED use. Among 21 persons who experienced nontraumatic cardiac arrest, 18 were in VF and 11 (61%) survived. In five of these cases, persons who had no training or experience in the use of AEDs and no official duty to respond used the AED.40a This study suggested there is benefit in deploying AEDs in high-volume venues and making AEDs available for use by the general public.
Current Concepts
On-Site Rescuers with Defibrillator
If the collapse is witnessed, a defibrillator is present, and someone onsite is willing to use it, defibrillation should be administered as soon as the defibrillator is ready. The efficacy of on-site AED use is now supported by two large multicenter studies. The Public Access Defibrillation Trial compared outcomes between two on-site responder strategies at 1,000 locations through 20 different centers across the United States and Canada.41 Both strategies included development of a response plan and training of designated responders in CPR. Half of the sites were randomized to also have training in AED use and placement of on-site AEDs. Study sites comprised a range of settings, including office buildings, multiresidential units, and shopping malls selected to have an expected likelihood of one cardiac arrest per year. Survival was double in the AED arm. Interestingly, VF was the initial rhythm in 59% of victims at the AED sites; this is higher than what has been recently reported in some EMS-based cardiac arrest studies.
Surveillance data reported from the Resuscitation Outcomes Consortium (ROC) funded by the National Institutes of Health found that on-site AED use doubled the likelihood of survival after controlling for associated risk factors. This study looked at 10,663 patients with cardiac arrest treated by EMS at the 11 ROC sites. Overall survival to hospital discharge was 7%; this improved to 9% with bystander CPR and to 36% with bystander CPR and bystander AED use. Unfortunately only about 30% of patients received bystander CPR and only 2.4% bystander AED.42
Likely scenarios for defibrillation by on-site rescuers include AED use by lay-bystanders at a public location and use of an automated or manual defibrillator by health care personnel in a hospital or clinic.
Emergency Responders
There is mounting evidence from both animal and human research to suggest that resuscitation will be more successful if chest compressions are performed for a brief period prior to defibrillation for patients with longer than a brief period of VF (>5 minutes or so) (see Sidebar 13-1 above).6 The period of chest compressions is believed to improve the metabolic state of the myocardium and, therefore, make the heart more amenable to defibrillation and to resumption of an organized cardiac rhythm with mechanical contraction. Thus, when rescuers must respond to the victim from off site, particularly when the response interval is >5 minutes, it may be beneficial to provide 90 to 180 seconds of chest compressions prior to attempting defibrillation.5,6
The AHA ECC 2005 guidelines suggest that EMS personnel may administer about 5 cycles (roughly 2 minutes) of CPR before checking the ECG rhythm and attempting defibrillation in treating an out-of-hospital cardiac arrest they did not witness. This recommendation is supported by two clinical studies of adult out-of-hospital VF SCAs. In those studies, when EMS call-to-arrival intervals were 4 to 5 minutes or longer, victims who received 1.5 to 3 minutes of CPR before defibrillation showed an increased rate of initial
resuscitation, survival to hospital discharge, and 1-year survival when compared with those who received immediate defibrillation for VF SCA.5,6 One randomized study, however, found no benefit to CPR before defibrillation for SCAs not witnessed by a paramedic.43 There is no evidence to provide a current recommendation for CPR before defibrillation for in-hospital cardiac arrest. A large-scale, multicenter, randomized comparison of the two treatment strategies (immediate shock versus shock preceded by a defined period of CPR) is currently under way and may provide the basis for future treatment recommendations.
resuscitation, survival to hospital discharge, and 1-year survival when compared with those who received immediate defibrillation for VF SCA.5,6 One randomized study, however, found no benefit to CPR before defibrillation for SCAs not witnessed by a paramedic.43 There is no evidence to provide a current recommendation for CPR before defibrillation for in-hospital cardiac arrest. A large-scale, multicenter, randomized comparison of the two treatment strategies (immediate shock versus shock preceded by a defined period of CPR) is currently under way and may provide the basis for future treatment recommendations.
Defibrillators
Manual
Manual defibrillators are designed for use by health care providers with training in cardiac rhythm recognition and management. The device has a screen for visualization of the rhythm, often with the capability for viewing multiple leads. The operator sets the energy level, initiates charging of the capacitor, and manually triggers the delivery of current. Most devices allow shock delivery through both handheld paddles and self-adherent pads (see “Paddles Versus Pads,” below). Manual devices usually have the capability to provide synchronized cardioversion, defibrillation (unsynchronized cardioversion), and transcutaneous pacing. Further, they may incorporate other monitoring capabilities, including noninvasive and invasive blood pressure measurement, pulse oximetry, and capnography. Some can also be used in an automated mode for defibrillation.
Automated External Defibrillators
Automated external defibrillators (AEDs) are sophisticated, reliable computerized devices that use voice and visual prompts to guide lay-rescuers and health care providers to safely defibrillate persons in VF, as demonstrated in many clinical trials.24,33,38,40,44,45,46,47,48,49,50,51,52,53,54
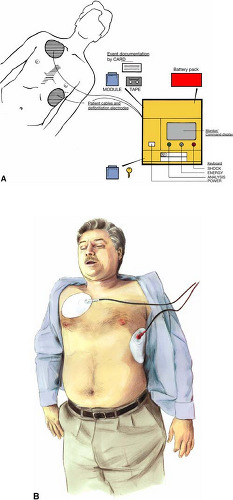
These portable devices are able to analyze the ECG rhythm, determine the presence of predetermined rhythms eligible for shock therapy, advise the user when such a rhythm is present, and deliver a defibrillation shock (Fig. 13-3). The ECG signal is input through two large self-adhesive pads that attach to the patient’s chest wall and connect to the AED with a several-foot-long cable; these pads also serve to deliver the shock. AEDs have microprocessors that analyze multiple features of the surface ECG signal, including frequency, amplitude, and some integration of frequency and amplitude, such as slope or wave morphology. Filters check for QRS-like signals, radio transmission, or 50- or 60-cycle interference as well as loose electrodes and poor electrode contact. Some devices are able to detect patient movement and, when this is detected, interrupt further rhythm analysis and shock delivery. The shock delivery function comprises a capacitor which is charged when an appropriate rhythm is detected. The energy source is typically a removable battery, either rechargeable or, more commonly, a long-life nonrechargeable type such as a lithium-based battery. In some models, the energy level of first and subsequent shocks is programmable in advance but not adjustable by the provider at the time of use, as it is with manual defibrillators.
AEDs use proprietary algorithms developed through the analysis of many ECG recordings to determine if a particular
rhythm should be shocked. “Shockable” rhythms include VF and wide-complex, rapid tachycardia. At least one brand will advise shock of narrow-complex tachycardia with a prespecified rate threshold, but this function can be disabled. All other rhythms are referred to as “nonshockable;” when these are detected, the user is directed to begin (or resume) CPR.
rhythm should be shocked. “Shockable” rhythms include VF and wide-complex, rapid tachycardia. At least one brand will advise shock of narrow-complex tachycardia with a prespecified rate threshold, but this function can be disabled. All other rhythms are referred to as “nonshockable;” when these are detected, the user is directed to begin (or resume) CPR.
AEDs have been tested extensively, both in vitro against libraries of recorded cardiac rhythms55 and clinically in many field trials in adults56,57 and children.58,59,60,61 They are extremely accurate in rhythm analysis, even in the presence of electromagnetic fields.62,63 While early models were noted to in rare instances shock inappropriately,64 in recent studies, sensitivity for VF is over 90% and specificity at or near 100%.34,41,65
AEDs come in a variety of models with varying levels of capabilities, complexity, and ruggedness. All are designed to be easy to use and provide voice and visual prompts to guide the user. The original models and some current models are designed with the premise that trained persons will use them, so prompts are more limited and may include jargon. Many of the newer models are designed with simpler-to-understand but more detailed instructions, such that even untrained laypeople can use them successfully.
Prototype devices were used in two recent clinical trials that recorded information about the frequency and depth of chest compressions during CPR.66,67 This suggests that in the future, AEDs may be able prompt rescuers to improve CPR technique in real time based on actual rescuer performance.
Automated External Defibrillator Operation
After confirming that the victim is likely in cardiac arrest (unresponsive, lack of normal breathing) and calling 911, the main steps in using an AED include the following:
Turn the device on (mechanism varies by model) and follow prompts.
Place electrode pads on patient’s bare chest (see Fig. 13-3) and attach cable to device if necessary.
Push “Analyze” button if necessary. Many devices will begin rhythm analysis automatically as soon as an adequate ECG signal is detected. No one should touch or move the patient during analysis.
Push “Shock” button if so prompted, or begin CPR if no shock is advised. Note that fully automated devices will deliver shock after warning without user action. No one should be touching the patient during shock delivery, although recent evidence suggests that there is minimal risk of shock to a gloved rescuer should there be such contact while performing CPR.68
Fully Versus Semiautomated
If a shockable rhythm is determined to be present, a fully automated AED will automatically charge and fire, while a semiautomated unit will prompt the operator to push a button for shock delivery to occur. The advantage to the fully automated device is that it may decrease operator delays in shock delivery once the device is ready to shock; the disadvantage expressed by some is that the user does not have control of shock delivery, such as if someone were to be touching the patient or in the rare instance that the patient were to regain signs of life.
Device Maintenance and Readiness
Defibrillators fall into the category of items that are used rarely or relatively infrequently but must be available and ready for immediate use when needed. Therefore, it is essential that a process be in place to assure that every defibrillator (whether manual or automated, whether in hospital or at a public location) is both present where it is supposed to be and is in a state of operational readiness. Most AEDs have an automated daily self-check function that confirms such items as residual battery power and the presence and, in some cases, intactness of pads. The “ready indicator,” easily visible on the AED, should be checked daily. Less frequently, typically monthly, many AEDs also do a more comprehensive check, including charge circuitry and capacitor testing. A manual check of every AED should also be performed at some regular interval (e.g., monthly or quarterly) to assure that battery or pads do not need to be replaced and that the device is otherwise intact. For both manual and automated defibrillators, the manufacturer’s recommendations should be reviewed and, if it is decided to deviate from these, this should be noted and explained in writing.
Implanted Cardiac Defibrillators (See also Chapter 24)
Indications and General Operation
Implantable cardioverter-defibrillators (ICDs) are now indicated for secondary prevention in most patients with a history of sudden cardiac arrest or hemodynamically significant ventricular arrhythmias and as primary prevention in those with New York Heart Association class II or III heart failure and ejection fraction <35%, prior myocardial infarction with systolic dysfunction (ejection fraction <35%), or other high-risk factors for VF or tachycardia (Fig. 13-4).69–70a ICDs can automatically detect cardiac arrhythmias and deliver programmable energy shocks directly to the myocardium, repeated if necessary, usually through a transvenous lead in the right ventricle. Modern implanted devices have the capability to also do both antitachycardic and bradycardic pacing. The generator boxes are usually implanted subcutaneously in the left infraclavicular area of the chest wall but may also be right infraclavicular or in the abdominal wall.
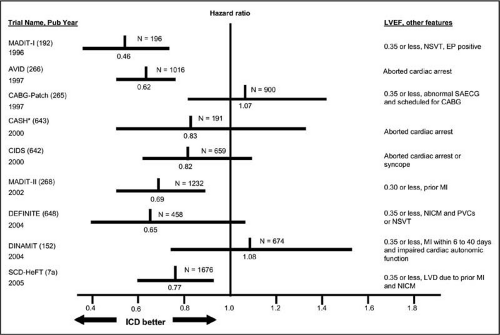 Figure 13-4 • Major implantable cardioverter-defibrillator (ICD) trials. Hazard ratios (vertical line
Get Clinical Tree app for offline access
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|