Damage Control Surgery
Brett H. Waibel
Michael F. Rotondo
I. History and Evolution of Damage Control
The foundation of damage control surgery (DCS) focuses on exsanguinating truncal trauma. The underpinning for damage control is that a traditional operative approach risks physiologic exhaustion, and an abbreviated initial operation controlling only hemorrhage and contamination and allow aggressive resuscitation in the intensive care unit (ICU) is better. Once the trauma cascade of hypothermia, coagulopathy and acidosis is resolved, repair of all injuries begins.
Due to its success, the clinical application of “damage control” has expanded into other areas, such as the septic abdomen and orthopedics, and underlies many triage and planned surgical responses to mass casualties for both military and civilian surgeons.
II. Damage Control Indications
The patient’s physiology will drive the decision to perform DCS. Multiple variables interact to prevent absolute determinants for instituting DCS. The operative needs must be balanced with the condition and response to the injuries or insult sustained (i.e., fecal peritonitis). Thus, the patient must constantly be reevaluated to identify those who would benefit from an abbreviated approach versus definitive repair.
Critical physiologic factors
Hypothermia (temperature below 35°C)
Acidosis (pH below 7.2 or base deficit exceeding 8)
Coagulopathy defined as non-mechanical bleeding within or without the surgical field, increase in prothrombin (PT) and/or partial thromboplastin time (PTT), thrombocytopenia, hypofibrinogenemia, or massive transfusion requirements (greater than 10 units packed red blood cells [pRBC] or blood volume replaced)
Prohibitive operative time required to repair injuries (greater than 90 minutes)
Hemodynamic instability or profound hypoperfusion
Injury complexes generally leading to development of instability
High-energy blunt torso trauma
Multiple penetrating torso injuries
Multiple visceral injuries with major vascular trauma
Multiple injuries across body cavities, especially those with competing priority for treatment, such as closed head injury, major vascular injury, and pelvic trauma.
Other considerations
Presence of injuries that may be better treated with nonsurgical adjuncts, such as angiographic embolization: Hepatic or pelvic injuries, deep large muscular bleeding, endovascular stenting, etc.
Limitations in physiologic reserve, often seen in the elderly and those with multiple medical comorbidities.
Complex surgical procedure(s) beyond the scope and training of the initial surgeon or resources of the facility.
III. Damage Control Sequence
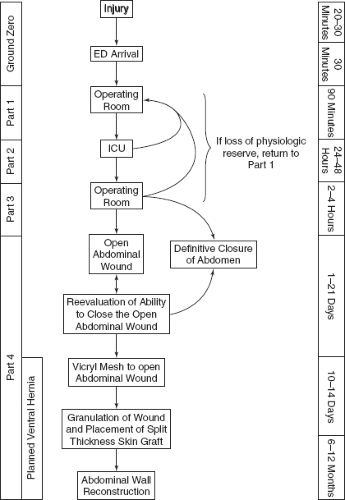
The DCS sequence was initially described in three phases. The initial abbreviated laparotomy (DC I) is followed by ICU resuscitation
(DC II) then definitive repair of injuries at a subsequent laparotomy (DC III). Definitive closure of the abdominal wall (DC IV) and the initial presentation and resuscitation (DC ground zero) were later added. Damage control is best seen as a series of tactical phases linked by the need to progress the patient from near death to reconstruction and recovery (Fig. 6-1).
(DC II) then definitive repair of injuries at a subsequent laparotomy (DC III). Definitive closure of the abdominal wall (DC IV) and the initial presentation and resuscitation (DC ground zero) were later added. Damage control is best seen as a series of tactical phases linked by the need to progress the patient from near death to reconstruction and recovery (Fig. 6-1).
Ground zero (initial resuscitation)
Prehospital care—see Chapter 9
Initial hospital resuscitation
In patients entering the damage control pathway, simultaneous resuscitation, diagnosis, and concurrent onset of definitive care are necessary to hasten the onset of operation. The use of permissive hypotension (targeting systolic BP of 90 mm Hg) is begun in the prehospital setting and continued during the initial resuscitation until surgical control of the bleeding can be obtained. The clinical picture of the patient is generally someone with critical injury, either single or multiple, and profoundly abnormal vital signs as a manifestation of exsanguinations and severe hypovolemia. If Class IV shock exists – hypotension and bradycardia are present and herald a profound under-perfusion of the heart – most of these patients will fail to respond to blood administration and can only benefit from the immediate identification and surgical control of bleeding.
Adjuncts – Focused Abdominal Sonography in Trauma [FAST], diagnostic peritoneal lavage, tube thoracostomy, and radiographic imaging of the chest and pelvis – allow rapid localization of hemorrhage sites, but are not infallible. In general, fluid in the peritoneal cavity with hypotension indicates need for celiotomy, while large initial volume evacuation or ongoing drainage from tube thoracostomy (>1,500 mL initial, >200 mL/h over 3 to 4 hours) indicates the need for thoracotomy.
Damage control resuscitation (DCR), the aggressive transfusion policy of 1:1:1 (pRBC:FFP:platelets), made popular by the military experience in Iraq has become prevalent for civilian trauma patients. The current opinion favors the combined approach of limited crystalloid infusion, early Type O blood administration, permissive hypotension, and balanced ratio type specific or type and crossmatched blood product resuscitation.
While the optimal transfusion ratios have not been proven, most favor equal numbers of packed cells and plasma with early platelet administration. The volume of crystalloid is limited to that which allows organ perfusion and function, but does not return hydrostatic pressures to normal (permissive hypotension). Blood component products provide both volume expansion and function, such as clotting factors and oxygen carrying capacity. Most civilian reports show similar improvements (to the military experience) in mortality with the DCR approach.
Massive transfusion programs require protocols to assure the availability of large volumes of blood components quickly. These programs have been shown to lower mortality and not be wasteful of blood products.
Damage control I (initial abbreviated laparotomy). The goals of the initial celiotomy are to obtain control of hemorrhage and ongoing contamination. Definitive repair of injuries is deferred until subsequent operations to allow a further resuscitation period in the ICU.
The peritoneal cavity is opened and packed to obtain initial control, especially for hepatic, retroperitoneal, and pelvic structures. Abbreviated maneuvers are used to control vessel bleeding and perforated or lacerated viscera are temporary packed to limit leakage.
Once all injuries are identified, a plan is set to provide minimal acceptable care of all injuries to allow the patient time to reverse the physiologic insult. Shed blood can be collected for autotransfusion, but is effectively devoid of clotting factors and platelets and if heavily contaminated best not re-infused. The guiding principle at this stage is that the more severe the injury(ies) and the more altered physiology, the less definitive repair during the initial laparotomy.
Positioning and packing
While positioning for obvious isolated abdominal or thoracic injuries is straightforward, combined thoracoabdominal injuries are less so as neither the supine nor lateral decubitus position will allow simultaneous access to both cavities. The taxicab hailing position will often allow for practical exploration of both cavities, as well as sternotomy. The patient is placed in supine position with the chest laterally rotated about 30 degrees off the coronal plane using folded blankets. The arm is abducted, elbow flexed, and arm rotated above the head to allow exposure to the chest wall.
Preparation of a wide area is preferable. The preparation should be from neck to knees bilaterally. Patient warming can be difficult given the extent of exposure, but warming of the environment and intravenous fluids and placement of appropriate warming devices underneath the patient can minimize further heat loss and aid in reversing hypothermia.
Upon entry into the abdominal cavity, the four quadrants should be packed to tamponade bleeding. If effective, this allows a period to further resuscitate the patient and communicate important physiologic and lab parameters (pH, temperature, BP, etc.). This pause is used to set the surgical tactics and plan. Packs should be initially removed from areas without active bleeding to develop working space. It is possible to overpack the peritoneal cavity producing decreased venous return via compression of inferior vena cava and inhibiting pulmonary excursion; continual communication with the anesthesia team is critical.
Hemorrhage control
Hemorrhage control is a continuum across the multiple body cavities/regions. The surgeon should begin with the most compelling source of bleeding and then proceed to other areas quickly as circumstances evolve. Important in this concept is that some bleeding sites may not be present in the exposed surgical field. For most injuries, control can be achieved with combinations of manual tamponade, vascular clamps, and suture ligation of nonessential vessels.
Most major vascular injuries do not need definitive repair at time of DC I. Surgical shunts in major arteries and veins can be used as conduits in the interim in preference to undertaking a complex repair and the time they required. Shunts also avoid ligation of critical vessels (e.g., external iliac artery, SMA, subclavian artery, etc.).
Solid organ injuries have approaches that are organ dependent. Some organs, such as spleen and isolated kidney, may be best sacrificed if unsalvageable or to expedite control. Hepatic injuries are generally amenable to packing followed by further definitive control using angio-embolization.
Avoid attempts to do more complex hepatorrhaphies or dissections, unless obvious large vessel bleeding in or around the liver is present.
Use angiography in any complex injury that is not controlled directly, such as complex renal, pelvic, or soft tissue injuries.
Ongoing arterial bleeding, whether in a viscera or cavity, will not be controlled with packing alone. Proximal control is needed, or the use of interventional radiology (ideally in the operating room) for these difficult injuries.
The operation should not end if ONGOING BLEEDING IS PRESENT, even though the patient remains hypothermic, acidotic, and coagulopathic. LEAVING AN ABDOMEN WITH ONGOING SURGICAL BLEEDING IS DESTINED TO FAILURE AND DEATH.
Contamination control
Hollow viscus injuries predominate and are straightforward in their treatment. Simple suturing or stapling techniques can control defects or rapidly removed injured segments to gain contamination control. Avoid definitive repair of these injuries, reestablishing intestinal continuity, stoma formation, or feeding ostomies at this time.
Biliary injuries can be temporized with external drainage, avoiding complex repairs.
Pancreatic injuries can be complex to manage. Packing alone is inadequate for control of pancreatic secretions. Wide area, closed suction drainage (multiple drains) of these injuries is required for control of the activated digestive enzymes to prevent secondary injury to the surrounding tissues. Definitive treatment and duct evaluation occur later.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree