Fig. 4.1
The progression of an intra-abdominal infection
Fig. 4.2
The persistent septic shock cycle
Fig. 4.3
Paradigm shift in management of patients with an abdominal infection and septic shock
Integrating Damage Control Laparotomy in Sepsis Management
Preoperative Optimization
This will take 2–3 h to accomplish. Patients are entered into the 24-h early sepsis management protocol. They are bolused with 20 ml/kg of ideal body weight of isotonic crystalloids and given rescue bolused norepinephrine as needed to maintain mean arterial pressure (MAP) greater than 65 mmHg. Broad-spectrum antibiotics are administered. At least two large-bore intravenous lines are needed. Given that the patient is in septic shock, a central line (via the internal jugular vein placed under ultrasound guidance) and an arterial line are placed. With ongoing volume loading, central venous pressure (CVP) is increased to above 10 cmH2O. At this point the patient is intubated. Avoid etomidate as an induction agent as it is known to suppress the adrenal function and its use in critically ill patients is associated with increased mortality [26]. Use ketamine instead, because it does not adversely affect cardiac function and it down-regulates pro-inflammation [27]. Ventilation is then optimized. Norepinephrine is titrated to maintain MAP >65 mmHg, and if high doses are required, stress-dose steroids are administered. Electrolyte abnormalities are corrected and blood products are administered based on institutional guidelines. Lactate and mixed venous hemoglobin saturations are measured.
Laparotomy
The goal is to have this completed as soon as possible and the priority of this operative intervention is source control. At the beginning of the operation the surgeons assess the degree of physiologic derangement (i.e., vasopressor requirements, acidosis, and evidence of DIC). If the patient is judged to be physiologically deranged then proceed into “damage control” mode. The surgeon should announce to the operating room team his/her intent to perform DCL and specific supplies that are needed (e.g., staplers, temporary abdominal closure supplies) and that this is going to be a short operation. Dead bowel is resected and debrided. Holes in the bowel are stapled to limit contamination. Big dissections are avoided to minimize consequent bleeding. Bleeding is packed as needed. Limited irrigation is performed to ensure no ongoing contamination. Use vacuum-assisted temporary abdominal closure. The operation should last 30–45 min.
Postoperative Optimization
The primary focus is to optimize resuscitation. The patient is volume loaded to increase CVP to >10 cmH2O and to decrease stroke volume variation to less than 13%. Non-responding patients should have an echocardiogram to assess for the presence of myocardial dysfunction, which often occurs with severe sepsis and should prompt the use of inotropic agents [28]. During acute resuscitation, the patient is sedated and provided full ventilator support. A short course of neuromuscular blockade is administered if the patient is fighting the ventilator until the clinical course stabilizes (usually within 12 h). If the patient develops acute lung injury, paralysis should be continued for 48 h to facilitate lung-protective ventilation, which improves outcome [29]. The goals are to correct abnormal physiology (e.g., hypothermia, coagulopathy, and acidosis) to prepare for a definitive second operation. Bladder pressure should be monitored in patients who require high-volume crystalloid resuscitation. Avoid large volume of hetastarch as this has been shown to cause AKI [30].
Second Operation
The temporary abdominal closure device and packs are removed and the abdomen is explored. Further resection and/or debridement are performed as needed. Next the surgeon needs to decide whether to perform an anastomosis or an ostomy. A left colon anastomosis should only be performed when conditions are ideal [31, 32]. A nasojejunal tube should be placed to facilitate early enteral nutrition. If feasible the fascia is closed, but the skin is not closed. If the fascia cannot be closed, replace a temporary abdominal closure device.
Ongoing Supportive ICU Care
By now the patient has completed the 24-h early sepsis management protocol that is implemented by CCDS and will be managed by the surgical intensivist using standard ICU protocols, including (a) sedation and analgesia, (b) lung-protective ventilation, (c) spontaneous breathing trials when indicated, (d) early enteral nutrition, (e) stress gastritis prophylaxis, (f) DVT prophylaxis, (g) tight glycemic control, (h) restrictive transfusions, and (i) early mobilization.
Recent Case Report
As part of the early sepsis management protocol hourly data are collected for 24 h. A flow sheet with these data is then given to the ICU team to review the next day on rounds so that they can see what happened during the sepsis resuscitation (see Fig. 4.4 as an example of one of these flow sheets). These data were collected from a 54-year-old male that was undergoing chemotherapy for a brain tumor and experienced a sudden change in mental status and became short of breath on the floor. He was transferred to the SICU due to the fact that the neurosurgical ICU was full. He presented with a systolic blood pressure of 70 mmHg, heart rate of 160 beats per minute (BPM), and temperature of 40.3°C. He was volume resuscitated and bolused with norepinephrine. The patient was in full-blown septic shock but the etiology was unclear. A screening abdominal X-ray (see Fig. 4.5) was obtained and demonstrated a dilated colon. Given the clinical presentation, this was presumed to be dead. The patient had ongoing hypotension despite aggressive volume resuscitation and was now on high-dose norepinephrine, low-dose vasopressin, and stress-dose steroids. He was too unstable for transport to the operating room. The family and the patient’s attending physician wanted to pursue all options. The ACS attending on call was notified and decided to perform a DCL in the ICU (see Figs. 4.6 and 4.7). The dead colon was removed and a temporary abdominal closure device was placed.
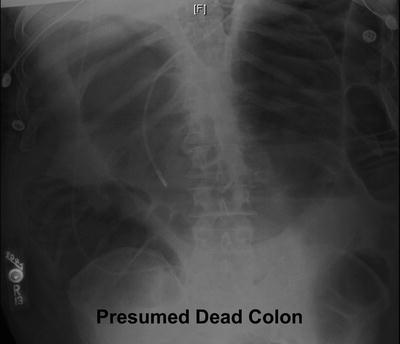


Fig. 4.4
Early sepsis management
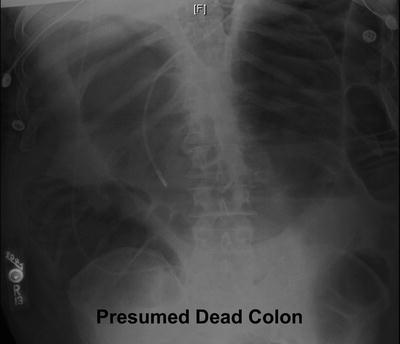
Fig. 4.5
Screening KUB X-ray

Fig. 4.6
Dilated colon found after opening the abdomen

Fig. 4.7
Abdomen after colon was removed
As can be seen in Fig. 4.4, this patient was gravely ill. He presented with a heart rate of 161 BPM, and he had a lactate of 3.9, and a creatinine of 2.5. With aggressive volume loading, the CVP was increased to 15 cmH2O and the heart rate decreased to less than 100 BPM. He required 7 l of lactated Ringer’s. Over the 24-h period, lactate levels normalized and the norepinephrine was weaned off. Of note, the creatinine levels normalized and there was no need for dialysis. The following day, the patient was taken to the OR where an ileostomy was performed and primary fascial closure was achieved. A nasojejunal tube was placed and the patient was placed on early enteral nutrition with an immune-enhancing diet. The patient underwent aggressive physical therapy and early mobilization. He was transferred to inpatient rehabilitation at day 11. His APACHE II score was 41 with a predicted mortality of 93%. This is an example of how DCL can salvage someone who would have previously died.
Our Recent Experience with an Early Sepsis Management Protocol in Surgical Sepsis
Over the last year a series of database analyses have been performed, some of which are relevant to this chapter. Fig. 4.8 depicts the 30-day mortality for severe sepsis/septic shock over 3 years of protocol development (2007–2009) [6]. Mortality data for 2006 and 2007 were collected by TMH Performance Improvement department as part of the Institute of Healthcare Improvement (IHI) Surviving Sepsis Campaign (SSC) [33]. The ACS group arrived in August 2006 and implemented a paper protocol in 2007 and 2008. Automated electronic medical record sepsis screening and CCDS were fully implemented in 2009. The 2008 and 2009 mortality were collected as part of the ACS sepsis database. These mortality data are also compared to the reported mortality of a recently published analysis of the National Surgical Quality Improvement Project (NSQIP) database and the 8th quarter mortality reported by the IHI SSC [11, 32]. As can be seen there was a tremendous reduction in mortality from 35% in 2006 prior to protocol development to 14% in 2009 after full implementation of early sepsis management protocol. We believe this is primarily due to (a) early detection of sepsis prior to the development of septic shock, (b) rapid implementation of evidence-based care with CCDS, and (c) selective use of DCL in patients presenting with abdominal catastrophes and septic shock.
Fig. 4.8
Decreased mortality with comprehensive sepsis management
Recent Experience with Damage Control Laparotomy in Surgical Sepsis
In 2009, we reported at the American Association for the Surgery of Trauma annual meeting the results of the 2007–2008 ACS sepsis database analysis (Fig. 4.9). Our objective was to determine the actual mortality versus the predicted mortality for patients undergoing DCL for intra-abdominal infection who were in septic shock (Fig. 4.10). We queried our prospective database over a 2-year period to identify patients with (1) septic shock, (2) intra-abdominal infection, and (3) those who had undergone DCL. We identified 41 patients who met the criteria for septic shock. Twenty-one patients had an intra-abdominal infection and underwent DCL. Sources of infection included the colon in 13, small bowel in 6, stomach in 2, and primary peritonitis in 1. Their average APACHE II score was 31.8 (±11.3) with a predicted mortality of 76%. Their P-Possum score was 74.9 ± 23.2 with a predicted mortality of 69.4%. The actual mortality was 27%, which is significantly lower (p < 0.02) than the predicted mortalities.