117 Contrast-Induced Nephropathy
The use of intravascular iodinated radiocontrast media is very prevalent. After injection of these contrast agents, a mild transient kidney function impairment can be detected by sensitive tests.1 However, clinically important kidney injury, known as contrast-induced nephropathy (CIN) or contrast-induced acute kidney injury (CIAKI), is less common, especially with normal preexisting kidney function.
CIN is usually defined as an acute kidney function impairment within 72 hours of intravascular injection of iodinated radiocontrast media, in the absence of other etiology. For research purposes, CIN is commonly defined as a 25% increase or an absolute increase in serum creatinine of 0.5 mg/dL (44 µmol/L) relative to precontrast values. Acute kidney injury (AKI) markers such as serum cystatin C, urinary neutrophil gelatinase-associated lipocalin (NGAL), or interleukin (IL)-18 will possibly be used in upcoming studies of CIN and may predict later CIN-associated morbidity and mortality.1
Awareness of the nephrotoxicity of contrast and the factors predisposing to it have improved over time to the point that clinicians may now overestimate the risk associated with some specific medical conditions.2 However, the increasing use of radiographic contrast media, possibly combined with increasing age and comorbidity of the treated population, contribute to the continuing importance of contrast nephropathy. In reality, given the mild and transient nature of the AKI in most CIN cases, it is the association with later more momentous clinical adverse events that drives current interest in preventing CIN.
 Epidemiology
Epidemiology
The exact incidence of CIN is not clear, ranging from 1% to 30%. This variability is due to lack of consistent definitions, variation in patient risk, contrast dose, and likely route of injection (intraarterial versus intravenous [IV]).2–4
Typically, about 15% of patients undergoing coronary angiography have serum creatinine rise by more than 25%, but the risk for dialysis is less than 1%.3 In the recent Cardiac Angiography in Renally Impaired Patients (CARE) Study,5 CIN defined by serum creatinine rise occurred in 11.1% of the 414 enrolled patients, while smaller increments in creatinine or rise in cystatin C occurred more frequently.5
The frequency of similar kidney function impairment after IV contrast injection appears to be many-fold less common than after cardiac angiography.6,7 In several studies, IV injection of nonionic low-osmolality contrast media (LOCM) in patients with chronic kidney disease was associated with a low risk of CIN.8
The fluctuation in serum creatinine due to other causes makes control groups not receiving contrast necessary to truly judge the risk to the kidney from IV contrast. In a small study, Langner et al. found a similar pattern of kidney function in a group having multiple contrast-enhanced studies with IV iodixanol as in a control group receiving no contrast media.9
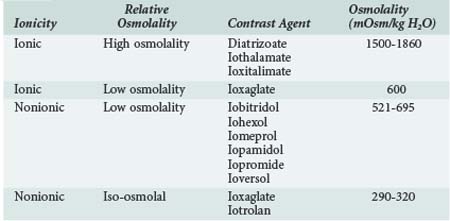
A variety of contrast media are available for use, and certain media are recommended ahead of others if a contrast study is required in a patient at risk for CIN. Contrast media are often classified according to osmolality and as ionic or nonionic (Table 117-1), but these factors are not necessarily the most important in determining nephrotoxicity. High-osmolality contrast agents such as diatrizoate are not commonly used nowadays and were associated with greater risk to the kidney. The relative toxicity of low and iso-osmolal contrast agents is controversial. Recent analyses suggest that CIN incidence may be higher with iohexol than with other LOCM, but the comparisons were across rather than within studies.10 A meta-analysis of pooled data from 16 randomized controlled trials (RCTs) including 2727 patients showed that intraarterial injection of the iso-osmolar contrast medium (IOCM), iodixanol, was associated with smaller rises in serum creatinine and lower incidence of CIN relative to low-osmolar contrast media (LOCM) (1.4% versus 3.5%, P = 0.003), especially in chronic kidney disease patients with or without diabetes mellitus (3.5% versus 15.5%, P = 0.003; and 2.8% versus 8.4%, P = 0.001, respectively).11 Nonetheless, a more recent meta-analysis of pooled data from 3270 patients and 25 trials including some of the above RCTs in addition to 7 new RCTs published within the last 3 years indicated that iodixanol is not associated with a significant decrease in the incidence of CIN compared with LOCM in the general population (relative risk [RR] = 0.80; 95% confidence interval [CI]: 0.61–1.04).12 Further, in this meta-analysis, iodixanol (IOCM) was less nephrotoxic than iohexol but not noticeably superior to other LOCM.12 Based on these data, current American Heart Association (AHA) guidelines recommend that either ioxaglate or a low-osmolality medium other than iohexol or ioxaglate be used in cases at risk for CIN.13
 Risk Factors
Risk Factors
The presence or absence of risk factors, especially preexisting kidney function, in addition to the type of imaging procedure are the most relevant predictors of CIN.3 The risk of dialysis-requiring CIN will increase considerably if precontrast creatinine clearance is less than 47 mL/min (0.78 mL/sec).3 Diabetes is a major risk factor,3,14 particularly in patients with diabetic nephropathy.15 Other factors associated with variable risk for CIAKI are: age older than 75 years, periprocedure volume depletion, heart failure, hypotension, cirrhosis, proteinuria, coadministration of nephrotoxins (e.g., diuretics, nonsteroidal antiinflammatory drugs [NSAIDs]), high doses of contrast, and intraarterial injection. The tolerable contrast dose depends in part on kidney function.3,16 Exceeding a maximum recommended contrast dose derived from serum creatinine and body weight strongly predicts dialysis-requiring CIN.4,16 The risk for CIN can be predicted by counting the number of risk factors present17 or by specific risk prediction models such as that shown in Table 117-2.18,19
TABLE117-2 Risk Prediction Score for Contrast-Induced Nephropathy Following Percutaneous Coronary Intervention
| Risk Factor | Score | |
|---|---|---|
| Systolic blood pressure <80 mm Hg longer than 1 h, requiring inotropes or intraaortic balloon pump (IABP) within 24 h of procedure | 5 | |
| Utilization of intraaortic balloon pump | 5 | |
| Heart failure (NYHA class III/IV) and/or history of pulmonary edema | 5 | |
| Age >75 years | 4 | |
| Hematocrit <39% in males, <36% in females | 3 | |
| Diabetes | 3 | |
| Volume of contrast medium | 1 for every 100 mL | |
| Serum creatinine level >1.5 mg/dL (133 µmol/L) | 4 | |
| Estimated GFR (eGFR) <60 mL/min per 1.73 m2 | 2; 40-59 mL/min/1.73 m2 4; 20-39 mL/min/1.73 m2 6; < 20 mL/min/1.73 m2 | |
| eGFR = 186 × (serum creatinine mg/dL)−1.154 × age−0.203 × (0.742 if female) × (1.21 if black) | ||
| Total Risk Score | Risk of CIN % | Risk of Dialysis % |
| ≤5 | 7.5 | 0.04 |
| 6-10 | 14.0 | 0.12 |
| 11-15 | 26.1 | 1.09 |
| ≥16 | 57.3 | 12.6 |
CIN, contrast-induced nephropathy; NYHA, New York Heart Association.
Adapted from Mehran R, Aymong ED, Nikolsky E, Lasic Z, Iakovou I, Fahy M et al. A simple risk score for prediction of contrast-induced nephropathy after percutaneous coronary intervention: development and initial validation. J Am Coll Cardiol 2004; 44:1393–9.
 Pathogenesis
Pathogenesis
Although debate remains about the exact pathogenesis in humans and the relevance of animal models, pathogenetic considerations inspire most efforts to prevent CIN. In vitro and animal studies suggest CIN results from direct toxic injury to renal tubular cells and medullary ischemic injury secondary to subcorticomedullary congestion.20,21
Injection of a contrast agent induces a biphasic renal hemodynamic change, resulting initially in a transient increase and then a more prolonged decrease in global renal blood flow.21 Cortical vasoconstriction and outer medullary vasodilation and congestion occurred during the hypoperfusion phase.20 Vasoactive substances including endothelin, vasopressin, prostacyclin, nitric oxide, and adenosine are involved in the cortical vasoconstriction.22–25
In humans, the pathogenesis of CIN is still unclear, and there is no specific diagnostic marker for CIN. Contrast may be a contributory rather than a sole cause of AKI in specific cases of CIN. Concomitant insults may include intravascular volume depletion, surgery, atheroembolic disease, or coadministration of other nephrotoxins (e.g., NSAIDs). The mechanism of cellular injury may also vary by contrast viscosity, dose and concentration, associated ions, concomitant hypoxemia, and oxygen free radicals.21,26
 Clinical Features and Diagnosis
Clinical Features and Diagnosis
Patients with CIN are generally asymptomatic but have an acute rise in serum creatinine concentration 24 to 72 hours after administration of the contrast agent. The renal failure is usually nonoliguric, but it may be oliguric, especially if there is significant preexisting renal impairment.27,28 Serum creatinine level typically peaks at 3 days and returns to baseline within 10 days.29 Clinically significant deterioration is unlikely if the serum creatinine concentration does not increase by more than 0.5 mg/dL within 24 hours.30 In a minority of cases, the renal failure is severe enough to require dialysis, or renal function does not recover to precontrast values. To make an unequivocal diagnosis of contrast nephropathy, other potential causes of acute renal failure must be ruled out. Prerenal factors, atheroembolic disease, and other nephrotoxic insults should be excluded. The relatively rapid onset and typical course may help differentiate CIN from other causes of AKI. Urinalysis may be unremarkable or may show granular casts, tubular cells, or proteinuria. Fractional excretion of sodium can be low.27,29
 Prognosis
Prognosis
Most episodes of CIN are self-limiting and resolve within 10 days, but CIN is consistently associated with increased morbidity, prolonged hospital stay, major adverse cardiac events, and early death.3,31 In the United States and Europe, CIN is the third leading cause of AKI in hospitalized patients, accounting for 10% of all causes of hospital-acquired renal failure.32 Less than 1% of CIN cases may require dialysis, and 13% to 50% of such cases may become permanently dialysis dependent.3,33
Although the association of CIN with adverse clinical outcomes other than requirement for dialysis has been clearly and consistently shown, it is not yet known whether CIN events are causally linked to early death and adverse cardiovascular events.5 If in fact CIN is causally related to these later events, efforts to prevent CIN become even more important. However, if CIN does not cause early death or major adverse events, it may be a less important health issue. Future trials using a variety of interventions with different mechanisms of action showing parallel diminution in CIN and adverse events are required to establish some evidence for causality.
 Preventive Interventions
Preventive Interventions
As outlined in Box 117-1, the risk of CIN can be reduced by general and specific measures. The first step is to assess the presence of risk factors and indications for use of a contrast agent. Most risk factors can be detected with a routine history and physical examination. It is not practical or necessary to measure serum creatinine concentration on every patient before use of a contrast agent, but this should be done in those patients with other risk factors.34 The following specific prophylactic measures have been studied and should be considered for high-risk patients.
Box 117-1
Recommendations to Reduce the Risk of Contrast-Induced Nephropathy
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree