Complications of Translaryngeal Intubation: Introduction
The term endotracheal intubation, or tracheal intubation, broadly refers to the insertion of a definitive artificial airway into the trachea by either the translaryngeal or transtracheal route. Translaryngeal intubation (TLI), a more specific term, is transoral or transnasal intubation of the airway through the larynx. The term endotracheal tube (ETT), as opposed to tracheostomy tube, refers to a tube passed via the mouth or nose into the trachea.
Macewen is usually given credit for the first successful translaryngeal intubation. In a landmark paper in 1880, he described TLI in four patients for as long as 35 hours and reported complications, including cough, discomfort, tracheal mucosal congestion, and thickening of the vocal cords and posterior rim of the glottis.1 The modern era of TLI began in the 1950s when it was used to manage respiratory failure from drug overdose2,3 and polio,4 and to provide an alternative to immediate tracheotomy when patients required prolonged ventilator support. As experience with TLI grew, so did knowledge of its complications and limitations. Comprehensive reviews of this subject appeared first in 19505 and frequently thereafter.6–14
This chapter provides a practical review of complications of TLI in critically ill adult patients, helps the reader understand the mechanisms underlying these adverse events, and illustrates how awareness of these complications may lead to their prevention, earlier recognition, and successful management. The chapter reviews important complications and consequences of TLI with standard ETTs that are encountered in the practice of adult critical care medicine. They are arranged according to the outline in Table 39-1. Complications of anesthetic intubations are occasionally cited to add awareness of complications that may also be seen in the critical care setting.
|
Frequency of Complications
The complication rate of TLI varies with the setting, the urgency of the procedure, the skill of the intubator, patient anatomy, and other factors. In the prehospital setting, the rate of complications of TLI ranges from 9.515 to 22.7%.16 In the emergency department, 8%17 to 38%18 of patients undergoing TLI experience one or more complications.
In a prospective study in the adult critical care setting, Stauffer et al observed that 62% of all TLIs had one or more associated adverse events either during intubation or while the ETT was in place.19 The mean number of complications per patient was 1.2. The most common early clinical problems were, in descending order of frequency, excessive cuff pressure required to seal the airway, self-extubation, inability to seal the airway, right main-stem bronchus intubation, and aspiration (Table 39-2). Other prospective studies have reported that 28% 20 to 39%21 of TLIs in the intensive care units (ICUs) of academic centers were associated with one or more complications, many of which were life-threatening. The complication rate of emergency TLI by anesthesia residents in ICUs and wards of large tertiary academic health centers ranges from 4.2%22 to 16.1%,23 with endobronchial intubation, airway trauma, aspiration, and esophageal intubation leading the list of observed complications.
| Clinical Problem | No. | Percentage |
|---|---|---|
| Excessive cuff pressure to achieve seal by minimal occluding pressure techniquea | 42 | 19 |
| Self-extubation | 29 | 13 |
| Inability to seal airwayb | 24 | 11 |
| Right main-stem bronchus intubation | 21 | 9 |
| Aspirationc | 17 | 8 |
| Lip ulceration or cellulitis | 16 | 7 |
| Pharyngeal injury or bleeding | 15 | 7 |
| Mechanical problems with the ETTd | 14 | 6 |
| Difficulty suctioning via the ETT | 12 | 5 |
| Pain in nose, mouth, pharynx, or chest related to the ETT | 8 | 4 |
| Glottic edema | 5 | 2 |
| Oral mucous membrane injury | 5 | 2 |
| Tooth avulsion | 4 | 2 |
| Laryngospasm at the time of extubation | 3 | 1 |
| Pneumothorax | 2 | 1 |
| Esophageal intubation | 2 | 1 |
| Miscellaneouse | 49 | 22 |
| Total number of complications observed: 268 |
Little is known about the impact of TLI complications on utilization of health care resources. One report found a significant increase in health care costs and hospital length of stay resulting from tracheal injury from ETTs.24
Complications during Endotracheal Tube Placement
Nasal intubation may inflict trauma to the nose, especially when it is performed urgently or without adequate premedication. A retrospective study of 105 nasotracheal intubations in the emergency department revealed a 26% rate of immediate complications, including epistaxis, emesis, and main-stem bronchus intubation, and a 23% rate of late complications such as pneumonia, sinusitis, and sepsis.25 Nasal bleeding complicated 54% of attempts at nasal intubation in an adult ICU.19 Dislodgment of nasal turbinates26 and nasal polyps27 is rare. Intracranial placement of nasotracheal tubes, particularly in the setting of facial trauma, has also been reported.28
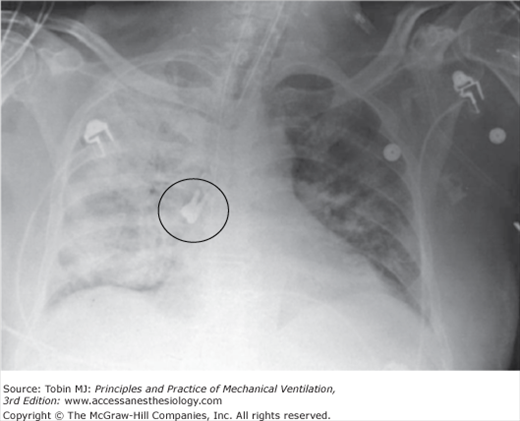
Overall, dental injury from TLI is uncommon, occurring in approximately 0.9% of prehospital TLIs,29 0.04%30 to 0.13%31 of anesthesia TLIs, and 0.2% of emergent nonoperating room TLIs.22 In anesthetic intubations, loosening, luxation, or avulsion of teeth, damage to crowns and bridges, and crown or root fracture were the most commonly observed dental injuries in two large series.30,31 Dental injury is the most common reason for anesthesia-related malpractice claims.31 Avulsed teeth and dental appliances may be aspirated into the trachea or bronchi.32 Figure 39-1 illustrates aspiration of a tooth in the setting of endotracheal intubation.32 Difficult intubation, poor dentition, and inexperience of the intubator predispose to dental injury.30 Oral mucous membrane injury has been observed in 1% to 2% of attempts at oral intubation.19 Lip injury occasionally occurs from pressure exerted by the laryngoscope blade. Temporomandibular joint dislocation is a very rare complication of anesthetic orotracheal intubation.33
Figure 39-1
Chest radiograph showing an aspirated molar tooth in the right main bronchus of an intubated patient. Pneumonia in the right lung was also observed. (Reproduced, with permission, from Ostrinsky Y, Cohen Z. Tooth aspiration. N Engl J Med. 2006;354:e25. Copyright © Massachusetts Medical Society.)
Lacerations, bleeding, contusions, excoriations, submucosal hemorrhage, and edema may result from intubation trauma to the nasopharynx, oropharynx, or hypopharynx. Oropharyngeal and hypopharyngeal injuries occur from trauma by the laryngoscope blade, ETT, stylet, or dislodged dental appliances.
Perforation of the posterior pharyngeal wall or hypopharynx is a particularly serious complication. It may result in mediastinal and subcutaneous emphysema, hematoma, upper airway obstruction, abscess formation,34,35 mediastinitis, pneumothorax, pneumomediastinum,36 pneumoperitoneum,37 and even cardiac arrest.8,38,39
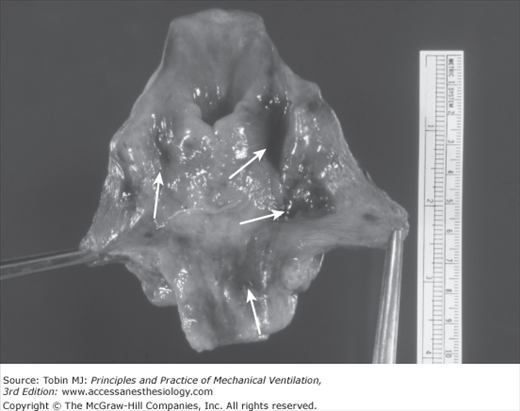
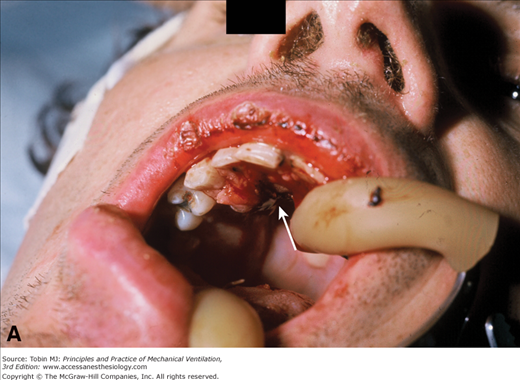
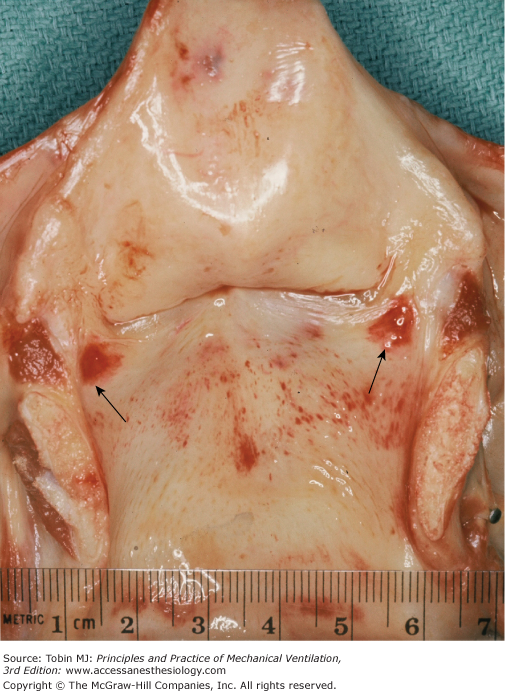
Hypopharyngeal injury from TLI has been the subject of a number of reports in both adults8,37–42 and children.43 Like oral injury, pharyngeal trauma from TLI occurs mainly in emergency settings and in the hands of inexperienced intubators, but it may occur in the anesthetic setting as well.44 Piriform sinus laceration by forceful blind intubation may result in severe barotrauma with bilateral pneumothorax, pneumomediastinum, mediastinal abscess, and cardiac arrest.40 Figure 39-2 illustrates hypopharyngeal contusions from repeated unsuccessful attempts at oral intubation by an inexperienced intubator.
Figure 39-2
Autopsy specimen of larynx, hypopharynx, and upper esophagus opened posteriorly. The patient was an older man with chronic obstructive pulmonary disease (COPD) and acute respiratory failure in whom repeated forceful attempts at oral intubation by an inexperienced physician were not successful. The tip of the ETT traumatized the airway. Multiple areas of submucosal hemorrhage in the piriform sinuses and hypopharynx are evident (arrows).
Reports of laryngeal complications that occur during ETT placement come mainly from the anesthesia literature. The larynx is the most common site of airway injury in anesthesia claims analysis.45 Laryngeal injuries during ETT placement include glottic contusion, vocal cord hematoma and laceration, vocal process avulsion,46 and arytenoid cartilage dislocation.46,47 Vocal cord hematomas are reported to be more common on the left true vocal cord,48 a finding that has been attributed to the fact that most intubators are right-handed.10 Epiglottic hematoma from TLI is considered very rare.49,50 Arytenoid dislocation from traumatic intubation occurs in up to 1.7%47 of anesthetic intubations, leading to complications such as hoarseness and aspiration47 and acute respiratory failure.51 Colice et al observed no cases of this complication in critical care intubations.52
Tracheal tears, reported variously as perforation,53 laceration,54 and rupture,55–59 are rare complications of TLI. The large majority of cases occur in women and in patients older than 50 years of age,60 and involve the posterior membranous portion of the trachea at or near the carina.61 Causes of tracheal tears include emergency intubation, damage to the posterior membranous trachea by a stylet,56 overinflation of the cuff,43,56 excessive coughing or movement during intubation, and preexisting abnormalities of the trachea such as tracheomalacia.55,60,61 Subcutaneous emphysema, pneumomediastinum, and respiratory distress are commonly seen after this type of tracheal injury.55,56
Malpositioning of the ETT in the trachea is a frequent consequence of emergency TLI in both the prehospital and the intensive care settings. In one report of prehospital airway management in a large urban region, malposition of the ETT was detected in 5.2% of 846 patients with attempted TLI in the field who were transported to a hospital.62 In a prospective series of 271 emergency TLIs in critically ill adults, Schwartz et al observed nine (3.3%) cases in which the ETT tip was too high (>6 cm above the carina) and twenty-three (8.5%) cases in which it was too low (<2 cm from the carina), in addition to ten cases (3.7%) of right main-stem bronchus intubation.63 Malpositioning of the ETT was significantly more common in women than in men.
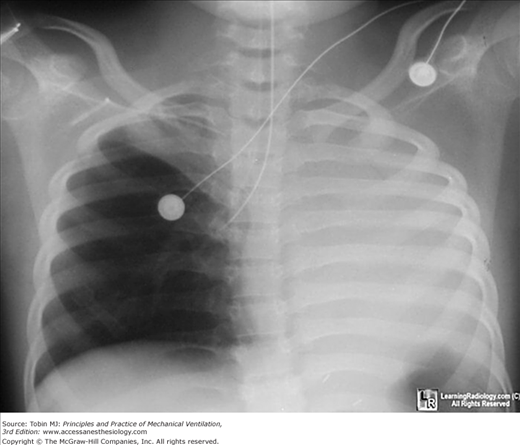
Intubation of a main-stem bronchus is a potentially serious complication of intubation.19,64,65 Right main-stem bronchus intubation has been reported in 10.7%66 and 15.2%67 of prehospital TLIs and in 3.7%63 and 9.6%64 of cases in prospective series of critical care intubations. In contrast, only 1.6% of anesthetic TLIs are complicated by endobronchial intubation.68 Left main-stem bronchus intubation is very rare.69 Potential complications of right main-stem bronchus intubation include hyperinflation of the right lung, right pneumothorax, atelectasis of part or the entire left lung, and impaired gas exchange. Figure 39-3 illustrates right main-stem bronchus intubation with the complication of atelectasis of the left lung.
Figure 39-3
Chest radiograph showing the tip of the endotracheal tube in the right main-stem bronchus. This case of right endobronchial intubation is complicated by left lung atelectasis. (Reproduced, with permission, from William Herring MD, www.learningradiology.com. Published with permission from LearningRadiology.com.)
Pulmonary aspiration, which is usually defined as the appearance of new infiltrates on the chest radiograph immediately after intubation, has been observed in 2% to approximately 6% of emergent intubation procedures.20–22,29,70 The prospective investigation of 297 TLIs in critically ill adults reported by Schwartz et al revealed twelve cases (4%) of new unexplained lung infiltrates attributed to aspiration and two cases of pneumothorax (1%).70 Aspiration of gastric contents was second only to failed intubation among all major complications of anesthetic airway management in a recent national survey in the United Kingdom.71 Besides pneumothorax, other types of barotrauma may occasionally be seen. Failed intubation attempts may lead to worsening gas exchange, including severe hypoxemia.72 Hypoxemia (oxyhemoglobin saturation <90%) has been reported in 18%72 to 21%73 of emergency TLIs. Hypoxemia was observed in 10.5% of TLIs when two or fewer intubation attempts were made, compared with 70% of TLIs requiring three or more attempts.72 Bronchospasm was reported in three (0.8%) of 358 prehospital TLIs.29 The bronchospasm response to TLI is rarely severe. Patients with asthma are at the highest risk.
Without adequate premedication, critically ill patients may experience pain in the upper airway, generalized discomfort, and anxiety during intubation. These important complications are difficult to assess objectively and are usually overlooked in large case reviews in the literature.
Bacteremia is an overlooked but potentially important consequence of both orotracheal and nasotracheal intubation.74,75 Staphylococci and streptococci are the most common bacterial isolates.75 The frequency of transient bacteremia following orotracheal intubation ranged from 3.2%74 in elective TLI for anesthesia to 9% in urgent TLI performed in ICU patients.76 In the latter series, only Streptococcus species were isolated immediately after TLI, and no patient had streptococcal bacteremia before or 1 hour after TLI. Bacteremia has been detected following 5.5%77 to 16%78 of nasotracheal intubations.
An analysis of claims for airway injury from anesthesia showed that the esophagus was the third most common site of injury, and esophageal injuries were more severe than all other types of airway injury combined.45 Inadvertent perforation of the posterior wall of the esophagus or pharynx by the ETT tip or rigid stylet is a rare but serious complication of TLI. Risk factors for this injury include inexperience of the operator, anatomic abnormalities, and difficult intubation, especially in the setting of cardiopulmonary resuscitation. The literature describing this complication is limited to single case reports79,80 and small series. O’Neill et al described two cases of esophageal and pharyngeal perforation from elective anesthetic intubation, noting that this severe complication is not always limited to emergency or difficult intubations.41 The potential consequences of esophageal perforation include subcutaneous emphysema, pneumomediastinum, pneumothorax, mediastinitis, and mediastinal abscess. Anterior esophageal perforation from TLI has not been reported.
Esophageal intubation is a common complication of TLI, particularly in emergency settings, and it has potentially severe consequences, including hypoxemia, regurgitation and aspiration of gastric contents, cardiac arrest, and irreversible hypoxic brain injury.81–83 Esophageal intubation occurred in ten (6.7%) of 149 patients intubated in the prehospital setting in Germany 66 and in thirty-seven (5.4%) of 691 patients intubated in the prehospital setting in France.29 It was reported in thirty-three (5.5%) of 603 patients intubated in an emergency department.17 In tertiary care centers the frequency of esophageal intubation complicating emergency TLI ranges from 1.3% to 9.7%.22,67,70,72
Gastric distension may result from esophageal intubation. Swallowing of foreign objects such as teeth and dental fixtures may also occur.84 TLI may stimulate the gag reflex, leading to vomiting.
Musculoskeletal complications during intubation are un- common. Injuries to the cervical spine and cervical spinal cord during orotracheal intubation have been reported.85
Hypoxic brain injury may result from ineffective ventilation, oxygenation, or circulation as a result of failed intubation or mishaps such as esophageal intubation. Cervical spinal cord injury is reportedly a rare complication of anesthetic TLI.86 Neck hyperextension during direct laryngoscopy to facilitate TLI in patients with restricted neck mobility or preexisting cervical spine instability has been proposed as a risk factor for cord injury,87 but proof of this relationship has been difficult to establish.88 Transient increases in intracranial pressure occur with TLI, particularly with endotracheal suctioning,89 putting patients with head injury at risk for secondary brain injury.90
The cardiovascular pressor response to laryngoscopy and TLI includes transient and variable increases in heart rate and both systolic and diastolic blood pressure as a result of pharyngeal stimulation. The magnitude of these responses varies with the route and ease of TLI,91 the use of anesthetic agents, concurrent medications, underlying cardiovascular status, and many other factors. In healthy individuals these cardiovascular responses are usually inconsequential, but complications may result when they are exaggerated92 or occur in patients with hypertension, cardiac disease, or cerebrovascular disease.93 Some, but not all, studies document a rise in plasma epinephrine and norepinephrine levels with TLI.94–97
The hypertensive response to nasotracheal intubation is greater than that to orotracheal intubation.96 The hemodynamic response to orotracheal intubation is greater than that to insertion of the laryngeal-mask airway (LMA North America, San Diego, CA),94 but less than that to insertion of the esophageal-tracheal CombitubeTM (Covidien, Mansfield, MA).94
Hypotension may also occur during TLI. In the setting of rapid sequence intubation for general anesthesia, Istvan observed hypotension in 27% of 248 patients undergoing appendectomy.98 Franklin et al observed that twenty-four (29%) of eighty-four patients requiring TLI in an emergency department developed life-threatening hypotension, which was significantly associated with the presence of chronic obstructive pulmonary disease, hypercapnia, and hypoxemic respiratory failure, but not with the administration of sedatives or paralyzing medications.99 Griesdale et al observed severe hypotension in thirteen (9.6%) of 136 patients requiring TLI in an academic ICU.21
MacKenzie et al reported cardiac arrhythmias in 58% and 32% of nasal and oral anesthetic intubations, respectively.100 Bradycardia was observed in 1.6% of emergency intubations in a large tertiary hospital when two or fewer intubation attempts were required versus 18.5% of intubations requiring three or more attempts.72 Most cases with bradycardia were associated with severe hypoxemia (arterial oxyhemoglobin saturation [SpO2] <70%) and half culminated in cardiac arrest.72
Cardiac arrest from emergency TLI is common. Mort reported cardiac arrest in sixty (2%) of 3035 critical care patients during emergency TLI in a tertiary care institution. Inadvertent esophageal intubation with profound hypoxemia, regurgitation, aspiration, and bradycardia were highly associated risk factors for cardiac arrest.103 Adnet described cardiac arrest as a complication of TLI in four (1.1%) of 358 patients with initial conditions other than cardiac arrest who required intubation in the prehospital setting.29
Schwartz et al reported a mortality rate of 0.85% during or within 30 minutes of emergency TLI in critical care patients without preexisting hypotension.70 Biboulet et al prospectively recorded eleven anesthesia-related cardiac arrests in a series of 101,769 anesthetics performed from 1989 to 1995 (frequency: 1.1 per 10,000), and the mortality rate was 0.6 per 10,000.104 All the cardiac arrests were considered avoidable.
Complications While the Endotracheal Tube Is in Place
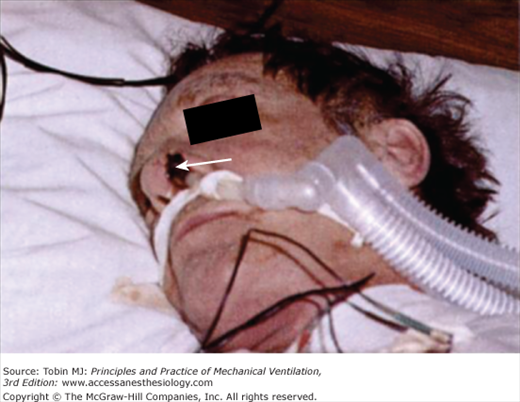
In a prospective series of 379 patients with nasotracheal intubation, Holdgaard et al found inflammation and ulceration of the nostrils or nasal septum in 110 patients (29%) within 5 days of extubation.105 Nasal bleeding occurred in 19% of patients and conchae fractures in 11%. Necrosis of the nasal alae may occur at the site of constant pressure on the nose by an upturned nasotracheal tube (Fig. 39-4).106 This injury was seen in 4% of nasotracheal intubations,107 and it may be accompanied by bacterial invasion with cellulitis.108 Nasal septal ulceration is uncommonly seen.19
Figure 39-4
Hemorrhagic ulceration of the left ala nasi (arrow) as a result of pressure exerted by a previously upturned nasotracheal tube. This type of injury can be prevented by positioning the endotracheal tube so that its proximal end points straight down from the anterior naris. (Modified, with permission, from Zwillich and Pierson.106)
Nasotracheal intubation for more than a few days commonly results in accumulation of fluid in the paranasal sinuses.108–110 Fassoulaki and Pamouktsoglou found computed tomographic (CT) scan evidence of paranasal sinus fluid accumulation, opacification, or mucosal thickening in all of sixteen adult patients studied prospectively by the eighth day of nasotracheal intubation.109 The maxillary and sphenoid sinuses each were affected in 87% of cases, followed by the ethmoid (50%) and frontal (12.5%) sinuses. Sinus effusions were unilateral and on the same side as the nasotracheal tube. Involvement of more than one sinus at a time was common.109 Ultrasound evaluation has demonstrated sinus effusions in 30% of patients with nasotracheal intubation108 and 63% of patients with orotracheal intubation.110
In 1982, Knodel and Beekman called attention to nasotracheal intubation as a cause of maxillary sinusitis with fever in mechanically ventilated patients.111 Sinusitis has subsequently been recognized as a common and potentially serious complication of TLI, particularly nasotracheal intubation (see Chapter 47).109,110,112–114 Sinusitis may also complicate orotracheal intubation115 and the use of nasogastric tubes.
Severe complications of TLI-associated sinusitis include fever, bacteremia, pneumonia, sepsis, and meningitis. Van Zanten et al reported that sinusitis was discovered as the sole cause of fever in fifty-seven (16.2%) of 351 critically ill patients with orotracheal intubation who were evaluated for fever of unknown origin.115 Gram-negative bacteria such as Klebsiella and Enterobacter species are commonly isolated from sinus aspirates in patients with sinusitis complicating nasotracheal intubation. Gram-positive bacteria, particularly Staphylococcus aureus, and fungi are also frequently isolated. Anaerobic infection, particularly with Bacteroides species, also occurs. Polymicrobial infections are common.
Middle ear effusion is an underrecognized but common complication of prolonged TLI, occurring in as many as half of patients.116,117 Cavaliere et al observed that twenty-eight (80%) of thirty-five unconscious ICU patients had middle ear effusion, and there was a significant association with TLI and mechanical ventilation.118 Lucks et al found middle ear effusions in twenty-three (29%) of seventy-eight adults with prolonged TLI, most of whom were intubated orally.119 Tympanocentesis revealed organisms in 22% of patients with middle ear effusion, particularly Pseudomonas aeruginosa, Klebsiella oxytoca, and Enterobacter cloacae, typical of the gram-negative organisms colonizing the airway in patients with TLI.118
Ulceration or cellulitis of the lips was noted in 7% of TLIs in critically ill adults.19 Lip edema, bleeding, and hemorrhagic crusts are very common during TLI as a result of pressure injury and abrasion by the orotracheal tube, oropharyngeal airway, tape, orogastric tube, or ETT holder.19,120 Figure 39-5 illustrates lip injury from prolonged orotracheal intubation.120 Hanley et al reported reactivation of herpes simplex virus infections in 53% of patients with oral TLI longer than 48 hours, but clinical findings were noted in only half of these cases.121 Figure 39-6 demonstrates herpes simplex virus type 1 complicating orotracheal intubation.122 Dental injury, stomatitis, erosion of the hard palate, and soft-tissue injury to the tongue and oral mucosa may develop during TLI, and in some cases these complications are severe (Fig. 39-7).19,123 They are reported to be more likely to occur in patients with concurrent use of oropharyngeal airways or those with rigid contracture of the jaw or propulsive movements of the tongue.123
Figure 39-5
Ulceration of the right side of the upper and lower lip in a patient with prolonged orotracheal intubation. This type of injury can be prevented by proper securing of the endotracheal tube (ETT), minimizing the direct pressure transmitted to the mouth from the ETT and ventilator tubing, and regular oral examination during the period of translaryngeal intubation. (Modified, with permission, from Stauffer.120)
Figure 39-6
Severe hemorrhagic lesions on the lips of a patient with an oral endotracheal tube (ETT) in place. Herpes simplex virus type 1 (HSV-1) was identified by culture and polymerase chain reaction assay. Reactivation of HSV-1 was considered to be related to immunosuppression of critical illness and friction trauma of the lips by the ETT. (Reproduced, with permission, from Tang JW, Chan PKS. Herpes labialis. N Engl J Med. 2007;357:1855. Copyright © Massachusetts Medical Society.)
Figure 39-7
Severe injury to the mouth may occur during translaryngeal intubation because of pressure-induced necrosis. This patient was a young man who was intubated because of status epilepticus and need to control the airway. Rigid contracture of the jaw occurred repeatedly while an oral pharyngeal airway was in place to prevent occlusion of the endotracheal tube by biting. Evidence of oral injury included erosion of the hard palate (arrow) by the oropharyngeal airway (A), and complete transection of the tongue, photographed at the time of surgical repair (B). (Modified, with permission, from Stauffer and Petty.123)
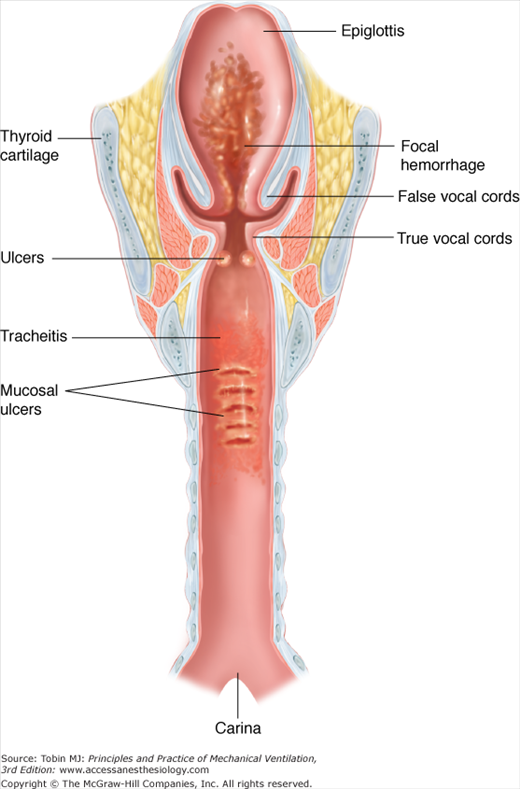
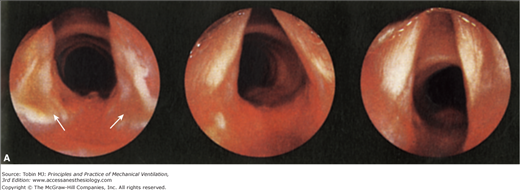
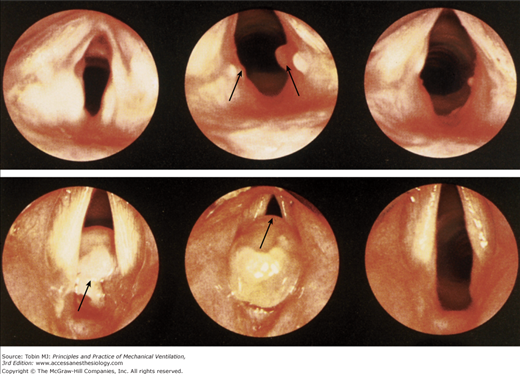
Laryngeal injury is the most common and potentially the most severe complication of TLI,52,124–134 and fear of late laryngeal complications of TLI is cited as the primary reason for performing tracheotomy for long-term airway maintenance. The most common postmortem findings in the larynx after prolonged TLI are mucosal ulceration, edema, and submucosal hemorrhage (Table 39-3).19,135 Figure 39-8 presents a schematic and illustrations of common TLI-induced laryngotracheal lesions. Figure 39-9 presents endoscopic views of selected cases of glottic injury from TLI in Lindholm’s comprehensive study.130
| Mucosal | ||||||
|---|---|---|---|---|---|---|
| Mucosal Ulceration | Inflammation and/or Edema | Submucosal Hemorrhage | ||||
| Site | No. | % | No. | % | No. | % |
| Epiglottis | 5 | 12 | 3 | 7 | 2 | 5 |
| Glottis | 21 | 51 | 12 | 29 | 5 | 12 |
| Subglottis | 5 | 12 | 1 | 2 | 3 | 7 |
| Trachea, cuff site | 6 | 15 | 16 | 39 | 3 | 7 |
| Trachea, other site | 2 | 5 | 20 | 49 | 3 | 7 |
| Total | 39 | – | 52 | – | 16 | – |
Figure 39-8
Schematic of the larynx and trachea opened posteriorly, illustrating common laryngotracheal lesions following translaryngeal intubation in the critical care setting (left). Autopsy specimen of larynx and trachea from an orally intubated patient showing hemorrhagic ulcers on the posterior aspect of the true vocal cords (arrows), patchy areas of mucosal hemorrhage on the anterior wall of the trachea from the subglottis to the carina (arrows), and a superficial mucosal ulcer at the site of the endotracheal tube cuff (arrows) (right). (Left panel modified, with permission, from Stauffer.135)
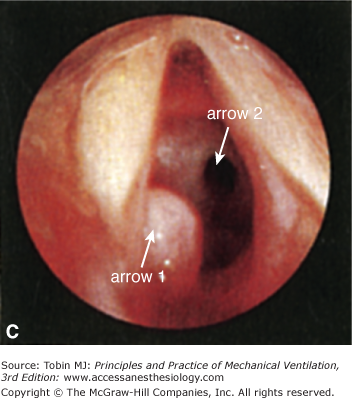
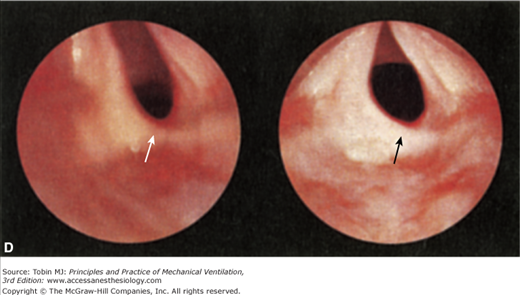
Figure 39-9
Endoscopic views representing types of translaryngeal intubation (TLI)-induced laryngeal injury observed by Lindholm in his prospective study of complications of endotracheal intubation.130 A, Superficial posterior glottic ulcers (left) (arrows) with healing over 18 days (center) and 32 days (right). B, Bilateral granulomas (arrows) that were absent at extubation but appeared by 44 days after extubation. C, Left subglottic granuloma (arrow 1) 14 months after TLI and tracheotomy. Tracheal stenosis (arrow 2) attributed to the tracheotomy is also evident. D, Fibrous scar at the left arytenoid region (arrows) 15 months (left) and 32 months (right) after TLI. (Modified, with permission, from Lindholm.130)
Experience with prolonged TLI in the 1970s showed moderate to severe laryngeal injury in 4.2%136 to 7.2%137 of cases. Kambic and Radsel found severe laryngeal injury in sixty-two (6.2%) of 1000 patients after anesthetic intubations, indicating that TLI for short periods and in a controlled setting was not without risk.124 Most prospective studies reveal that serious permanent laryngeal injury from TLI is very uncommon.19,129,138 All but a few TLI-induced laryngeal injuries tend to heal within 6 to 8 weeks and leave no permanent sequelae.52,128,138,139
Mucosal ulceration, significant inflammation or edema, and submucosal hemorrhage at autopsy have been noted in 12%, 7%, and 5%, respectively, of patients with prolonged TLI (see Table 39-3).19 Astrachan et al found severe supraglottic edema in 1% of TLIs.107
Ulceration of the posterior aspect of the true vocal cords and arytenoids has been reported in 51%19 to 79%130 of TLIs. This injury represents the most common significant complication of TLI.47,108,131–134,136,139,140 Investigators first reported posterior laryngeal ulcers from TLI in the early 1950s.141,142 Lindholm observed postmortem macroscopic ulceration or necrosis in the interarytenoid area, the medial side of the arytenoids, and the inner posterolateral area of the cricoid cartilage in 9%, 79%, and 68% of adults, respectively.130 Laryngeal ulcers from TLI are symmetrical, triangular-shaped erosions of the posterior and medial aspects of the vocal processes (Fig. 39-10) and arytenoids and the posterolateral area of the cricoid cartilages.47 They are typically 4 to 12 mm in diameter and 1 to 5 mm in depth, and they may penetrate into the cartilage131 and the cricoarytenoid joints. The areas most vulnerable to ulceration by pressure from the shaft of the ETT are the posterior endolarynx, the arytenoids, the cricoarytenoid joints, and the interarytenoid space.126 Using telelaryngoscopy, Deeb et al examined 142 adults who required tracheotomy because of failed extubation.143 They observed that mucosal erosions and ulcerations, often with exposed cartilage, were common, and the most severe ulcers affected the intercartilaginous glottis and posterior subglottis, often with extensive granulation tissue. In some cases, the paired posterior ulcers may be large enough to join each other, producing a “horseshoe lesion.”108
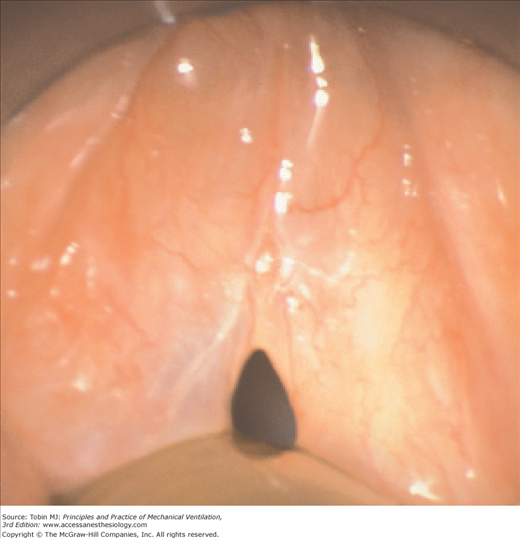
Varying degrees of hyperemia, edema, and inflammation of the glottic mucosa occur in practically all patients during TLI.19,52,125,130,139,140 Stauffer et al found severe edema and inflammation at autopsy in 29% of patients following TLI, particularly in the posterior commissure area.19 Figure 39-11 illustrates an example of intubation-related laryngeal edema.144
Figure 39-11
Laryngoscopic view of edema of the vocal folds following translaryngeal intubation. Some patients with this complication, which presents as postextubation stridor, may require reintubation. (Used, with permission, from Wittekamp.144)
This complication during TLI presents after extubation and is discussed (see the section Early Complications After Extubation/Laryngeal/Vocal Cord Paresis and Paralysis).
The incidence of glottic hemorrhage developing after intubation is not known. Stauffer et al found evidence of submucosal hemorrhage in the glottis in 12% of TLI cases at autopsy (see Table 39-3).19
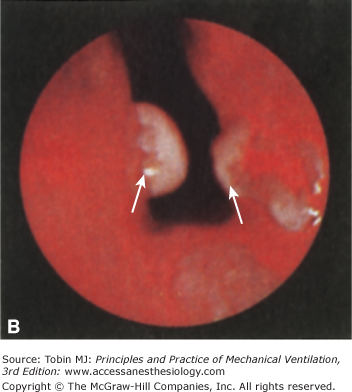
The term vocal fold granuloma refers to growths of granulation tissue at the site of mucosal injury as a result of abnormal tissue healing. These lesions typically appear at the site of laryngeal ulceration and vary in size from 2 to 3 mm to more than 1 cm in diameter. They may be unilateral or bilateral.130 Figures 39-9B and C and 39-12 from the series of Lindholm et al,130 present endoscopic views of small and large laryngeal granulomas following extubation. Laryngeal granulomas during TLI have been observed in up to 16%128 of patients during TLI. Although usually associated with prolonged TLI, laryngeal granulomas may also occur after short-term intubation.145,146 This topic is discussed in “Late Complications After Extubation.”
Figure 39-12
Laryngeal granulomas are growths of granulation tissue that may result from abnormal wound healing at the site of laryngeal ulcers. The top panel shows endoscopic views of the larynx 24 hours after extubation (left view), 20 days after extubation (middle view), and 34 days after extubation (right view). Small laryngeal granulomas (one on the left vocal fold and two on the right vocal fold) are evident in the middle view, and marked spontaneous improvement is observed 14 days later (right view). The bottom panel shows a very large polypoid laryngeal granuloma 5 months following short-term intubation (left and middle views) that caused respiratory difficulty and required surgical removal. Healing was achieved following surgery (right view). (Used, with permission, from Lindholm.130)
Cricoid cartilage abscess results from bacterial invasion of the cricoid cartilage after pressure ulceration by the ETT.10,108 Cricoid cartilage abscess may appear as long as 8 weeks after extubation and predispose to posterior glottic stenosis.10
Tracheal injury during TLI (Table 39-4) may occur at the site of the inflated cuff, at the level of the tip of the tracheal tube, and at the site of injury by suction catheters. Cuff-site injuries are the most common.19
|
Fiberoptic bronchoscopy during TLI often reveals varying degrees of tracheal inflammation and edema below the tip of the ETT. Mucosal edema or inflammation is found at autopsy in 39% of TLI patients at the cuff site and in 49% at other levels of the trachea (see Table 39-3).19 Infiltrates of neutrophils and mononuclear cells are found in the mucosa and submucosa at the cuff site.147
The use of high-volume, low-pressure cuffs on ETTs has greatly reduced the frequency of cuff-site ulceration. Figure 39-8 (right panel) illustrates a small cuff-site ulcer with exposed cartilage on the anterior tracheal wall. Severe cuff-site ulcers that were common in the era of hard-cuff ETTs148,149 are now rarely seen. Modern soft-cuff ETTs, however, do not completely protect the mucosa from injury. Stauffer et al reported tracheal mucosal ulceration at autopsy in 15% of patients with prolonged TLI with soft-cuff ETTs at the cuff site and in 5% at other tracheal sites (see Table 39-3).19 Soft cuffs apply lateral pressure over a longer segment than hard cuffs, and pressure from overlapping folds of the fabric of soft cuffs may create channels in the tracheal mucosa.150
Granulomas in the trachea are much less common than in the larynx following prolonged TLI, because tracheal ulceration is now much less common than laryngeal ulceration. All of the laryngotracheal granulomas observed by Lindholm were in the larynx.130 Astrachan et al found tracheal granulomas in only 1% of patients.107
Submucosal hemorrhage was found at autopsy in 7% of patients at both the cuff and other tracheal sites (see Table 39-3).19
Abbey et al reported a case of massive tracheal necrosis and suppuration after 10 days of TLI.151 Possible risk factors include sepsis, hypotension, and elevated cuff pressures.
Ulceration and eventual destruction of the C-shaped cartilaginous tracheal rings may occur as a result of sustained elevation of cuff pressure,152 resulting in tracheal dilation, tracheomalacia, and injury to the adjacent great vessels and esophagus.
Tracheal laceration and tracheal rupture are rare complications of TLI during the period when the ETT is in place.
Dilation of the trachea, a sign of severe tracheal wall damage,152 may appear even with soft-cuff ETTs during TLI or after extubation (See the section Late Complications After Extubation/Tracheal/Tracheal Dilation),153 although this complication is mainly related to tracheotomy.154 When tracheotomy is performed following long-term TLI, it may be difficult to determine whether the cuffed ETT or the cuffed tracheostomy tube was primarily responsible for the injury.155
Although tracheomalacia has been reported in patients with tracheotomy following TLI,156 tracheomalacia after TLI alone is very rare when ETTs with high-volume, low-pressure cuffs are used.
Cuff pressure–induced necrosis and erosion of the posterior membranous portion of the trachea and anterior wall of the esophagus may result in tracheoesophageal fistula.132,157,158 This rare complication of artificial airways has been mainly associated with tracheotomy,132,159,160 but TLI, even with soft-cuff ETTs, is also a risk factor.161 The concurrent use of a nasogastric tube could conceivably enhance the risk. Tracheoesophageal fistula may be silent or present with the appearance of gastric contents in tracheal secretions or with massive gastric distension.162 After cuff deflation or extubation, it may present with cough following ingestion of food.161
Tracheoarterial fistula is a very rare complication associated with long-term tracheotomy. This usually fatal event has been attributed to high cuff inflation pressure leading to tracheal necrosis and erosion of the wall of the innominate artery. Only a few cases of tracheoarterial fistula during prolonged TLI have been reported.163–165 In one of these cases, erosion into the innominate artery occurred at the level of the tip of the ETT, leading to fatal exsanguination on the fortieth day of TLI.165 There is one report of tracheoinnominate artery fistula complicating short-term anesthetic orotracheal intubation.166
Contact of the tracheal surface with an inflated cuff, ETT tip, or suction catheter results in loss of columnar tracheal epithelium cells and distortion of their cilia.167–169 Regeneration of the ciliated surface and restoration of ciliary structure and function occurs within 2 weeks after extubation167,168
Squamous metaplasia of the tracheal mucosa has been observed in dog models of intubation and in humans147,170,171 and is attributed to abrasion of the mucosa by the inflated cuff or suction catheter. It may involve both surface and glandular epithelium adjacent to necrotic tracheal ulcers following prolonged TLI.172
Tracheal injury at the cuff site depresses mucociliary clearance in both experimental animals and humans. Cuff inflation,168 squamous metaplasia,173 and loss of cilia169 all contribute to impaired mucociliary transport during TLI.
Colonization of the trachea with bacteria occurs in nearly all patients during TLI,174–176 mainly from aspiration of secretions above the inflated ETT cuff and from infected ETT biofilm.177 Gram-negative bacteria, particularly Pseudomonas species, have a particular tropism for the tracheobronchial mucosa. Bacterial colonization of the trachea during TLI is a risk factor for ventilator-associated pneumonia (VAP; see Chapter 46).177,178 Ventilator-associated tracheobronchitis in intubated patients (fever, purulent lower airway secretions, positive sputum cultures, and absence of new or progressive lung infiltrates) is also increasingly recognized as an important clinical infection in the ICU.179,180
Pseudomembranous tracheitis, a rare and little known complication of TLI that has been attributed to ischemic cuff-site injury, was first reported in 1969.131 Lins et al reported five cases and reviewed a total of twenty-four cases.181 Tracheal epithelial injury from aspiration of gastric contents during TLI has been also cited as a cause of tracheal pseudomembrane formation.182 Harbison et al reported a patient who presented with acute stridor from a fibrinous tracheal membrane 3 days after TLI lasting 48 hours.183 Removal of the membrane by rigid bronchoscopy was curative. Deslee et al described one fatal case of fibrinous tracheal pseudomembrane from TLI.184
Tracheobronchitis, protracted coughing, and consequences of ETT suctioning,89,185 such as chest pain, hypoxemia, and cardiac arrhythmias, are sometimes observed.
Main-stem bronchus intubation (see Fig. 39-3) is mainly a complication during ETT placement, but it may also occur after intubation. In a retrospective series of 278 adult ICU patients with TLI, Kollef et al found that seven (2.5%) had inadvertent endobronchial ETT placement.186
Pulmonary complications during TLI include aspiration, pneumonia, retained secretions, and atelectasis.
Aspiration of oropharyngeal secretions or gastric contents can be a serious complication while the ETT is in place.35,177,187–189 Leakage of contaminated subglottic secretions around the ETT cuff into the lower airway increases the risk of VAP.177 Estimates of the frequency of clinically significant aspiration during TLI range as high as 20%.188 Aspiration of gastric contents during TLI may be less common than aspiration of oral and pharyngeal secretions, but data are sparse.
VAP (see Chapter 46) is a common and serious threat to patients with artificial airways who require mechanical ventilation.35,177,178,190 VAP occurs in as many as 28% of patients during the course of mechanical ventilation.190 A large, retrospective, matched cohort study showed that VAP developed in 9.3% of adult patients receiving mechanical ventilation for more than 24 hours.191 The mortality rate of VAP ranges from 24% to 50%.190 Mechanisms of pneumonia related to TLI are discussed (see the section Pathogenesis of Complications of Translaryngeal Intubation/Complications While the Endotracheal Tube Is in Place/Clinical Influences in Pulmonary Complications/Pneumonia and Tracheobronchitis).
TLI may promote retention of bronchopulmonary secretions in the lung because of impaired cough performance.192
Atelectasis may complicate TLI as a result of retained bronchopulmonary secretions, migration of the ETT into a main-stem bronchus, and other factors operative during mechanical ventilation.
Certainly all who have cared for intubated patients recognize that anxiety, depression, feelings of isolation and withdrawal, and frustration with impaired communication are major psychological detriments related to TLI. The immediate and long-term psychological impact of TLI, however, has been the subject of only a few investigations. The psychological health of intubated patients is influenced not only by TLI, but also by noise, light, sleep deprivation, stresses of underlying illness, and other adverse influences in the ICU.193 In a study that was not entirely limited to TLI patients, Swaiss and Badran recorded the following distressing complaints in interviews of adult patients 1 day after discharge from the ICU: anxiety (68%), discomfort from the ETT (60%), fear (54%), pain (52%), discomfort from the nasogastric tube (48%), difficulty in communicating (33%), dreams and hallucinations (31%), discomfort from physiotherapy (24%), noise (15%), insomnia (13%), and thirst (10%).194
“Unplanned extubation” is a broad categorical term that includes self-extubations and other extubations that are variously called “accidental,” “deliberate,” and “inadvertent” in the literature.19,64,107,195–197 The overall frequency of unplanned extubations in critically ill adults is 8.6%.197 In a prospective epidemiologic study of more than 5000 critically ill adults with TLI, self-extubation was the most common accident related to TLI.198 Unplanned extubation is more likely to occur with oral than with nasal TLI.199,200 In a large case series, Chevron et al reported that unplanned extubation was usually deliberate (87% of patients) and associated with insufficient sedation.200 Unplanned extubation may occur from forces applied to the ETT by ventilator tubing, bedrails, patient motion, bucking, coughing, and forcing the tube forward with the tongue.
Coppolo and May reported a 12-month experience with self-extubation in adult ICU patients and noted self-extubation in 11%, cardiorespiratory sequelae of self-extubation in 31%, and need for reintubation in 31% of cases.195 Others have documented reintubation rates following self-extubation as high as 74%.201 Not surprisingly, the need for reintubation is much lower when self-extubation occurs during weaning from mechanical ventilation than during the period of full ventilator support.202 Besides the need for reintubation, sequelae of unplanned extubation include longer ICU and hospital stays,199,203,204 prolongation of mechanical ventilation,203 and complications of TLI.204
Various mechanical problems with ETTs occur in approximately 6% of intubations (Table 39-5),19 and they may place patients at risk for serious complications and need for reintubation. Beckmann and Gillies examined a large database of voluntary incident reports from ICUs in Australia and New Zealand to determine the frequency of reintubations not related to accidental or self-extubation.205 Among 143 such incidents, the reasons for reintubation included the following mechanical complications: tube malposition (twenty-five [17%]), tube securing or taping problems (twenty-four [16%]), pilot tube or cuff problem (twenty-three [16%]), and blocked or kinked airway (twenty [14%]), in addition to failed extubation (nineteen [14%]), inadequate preparation for extubation (eight [6%]), and other events (twenty-four [17%]).205
|
Dislocation or misplacement of an ETT may result in endobronchial intubation (see Fig. 39-3), carinal irritation by the ETT tip, high placement at the level of the upper trachea or hypopharynx, and self-extubation. Potential complications of high tube placement include injury to the larynx and adjacent structures including the recurrent laryngeal nerves, inability to seal the airway, leading to aspiration and inadequate ventilation, and subglottic stenosis. Kollef et al reported that twenty-two (8%) of 278 adult ICU patients had at least one significant ETT dislocation, with complications such as anoxic encephalopathy, hypoxemia, gastric aspiration, atelectasis, and pneumothorax.186 An earlier prospective study revealed ETT malposition in five (8.2%) of sixty-one patients with prolonged TLI.35
If an ETT is positioned too low in the trachea, flexion of the neck may allow it to migrate into a main-stem bronchus, and conversely, if an ETT is positioned too high in the trachea, extension of the neck may allow it to migrate into the pharynx, potentially leading to unplanned extubation.206 Conrardy et al showed that flexion of the neck moved the tip of the ETT an average of 1.9 cm toward the carina (range: 0 to 3.1 cm), and extension of the neck moved the ETT a similar distance away from the carina (range: 0.2 to 5.2 cm).206 The route of intubation (nasal vs. oral) and cuff inflation or deflation did not affect tube movement.
The ETT may become partially or completely obstructed during placement or while it is in place by patient biting, retained secretions, blood or blood clots, foreign bodies, tumor, or other material. Obstruction from tube kinking or external compression by cuff overinflation is very rare. The tip of the ETT may impact on the tracheal mucosa leading to tube obstruction if the tube lacks a Murphy eye.207
ETT cuff problems during TLI include leak, rupture, and inability to seal the airway. Rashkin and Davis noted leaky cuffs during TLI in fifteen (25%) of their sixty-one patients.35 Cuff rupture is now rarely observed. Inability to seal the airway by inflating or overinflating the cuff was the most common early clinical problem following TLI in one series.19 Vyas et al checked cuff pressures in thirty-two patients intubated with ETTs with high-volume, low-pressure cuffs and found that 62% had elevated cuff pressures, some as high as 100 cm H2O.208 They performed a telephone survey that revealed that cuff pressure was checked regularly in only 17% of ICUs.
A wide variety of other mechanical problems have been encountered while the ETT is in place, including malfunction of the one-way inflation valve, inadvertent severance of the inflation tube or pilot balloon, disconnection from the ventilator, and difficulty passing a suction catheter through the ETT.
TLI precludes effective swallowing and necessitates feeding by way of enteric tubes or intravenous lines. Chapter 41 discusses malnutrition in patients with TLI.
Tracheoesophageal fistula may develop during TLI (see the section Complications While the Endotracheal Tube Is in Place/Tracheal/Tracheoesophageal Fistula).
Gastric distension may occur if a tracheoesophageal fistula develops during TLI.162
Musculoskeletal and neurologic complications directly related to TLI while the ETT is in place have not been reported.
Compared with a normal upper airway, an ETT increases the resistance to airflow. Gal and Suratt demonstrated that TLI in healthy men increased total airways resistance from 0.99 cm H2O/L/s to 2.25 cm H2O/L/s, an increase of 178%.209,210 Approximately half of this increase was attributed to the ETT itself, and the remainder to reflex bronchoconstriction.209,210 TLI increases lower airway resistance slightly in normals without reactive airways disease by stimulation of irritant receptors, provoking bronchoconstriction,211 and prophylactic treatment with bronchodilators has a protective effect.212
Airflow resistance during TLI increases as the length of the ETT increases or its diameter decreases.213 Because they increase airflow resistance, ETTs increase the patient’s work of breathing.214 The work of breathing increases as the patient’s minute ventilation increases and as the diameter of the ETT decreases.214–216 At minute ventilation rates at or below 8 L/min, an ETT has little impact on the work of breathing.215 Although the extra work of breathing imposed by an ETT is not clinically important in most patients, it may be clinically significant in patients with poor ventilatory function.
Complications during and after Extubation
Oral, nasal, pharyngeal, and laryngeal complications that developed while the ETT was in place may, of course, first be detected at extubation. Table 39-6 lists complications of TLI that Stauffer et al observed immediately after extubation in the ICU.19 Hoarseness and sore throat are the most common symptoms at extubation. New complications occurring in the brief period of extubation are transient and uncommonly reported. They include discomfort, pain, and anxiety.193 Significant increases in heart rate, blood pressure, and plasma catecholamine levels occur at extubation.94 Nasal bleeding and dental injuries may occur during extubation, but such events are rarely reported.
| No. | Percent (%) | |
|---|---|---|
| History (obtained in sixty-nine patients) | ||
| Symptoms related to TLI | 59 | 86 |
| No symptoms related to TLI | 10 | 14 |
| Specific symptoms | ||
| Hoarseness | 49 | 71 |
| Sore throat | 29 | 42 |
| New cough | 18 | 26 |
| New sputum production | 15 | 22 |
| Hemoptysis | 7 | 10 |
| Other upper airway complaints | 9 | 13 |
| Physical examination (obtained in seventy-eight patients) | ||
| Abnormal, related to TLI | 42 | 54 |
| Normal | 36 | 46 |
| Specific abnormalities | ||
| Auscultatory abnormalities over the trachea | 20 | 26 |
| Lip ulcer or cellulitis | 12 | 15 |
| Pharyngeal bleeding or ulceration | 7 | 9 |
| Ulceration of the palate | 6 | 8 |
| Nasal bleeding | 6 | 8 |
| Oral mucous membrane bleeding, ulceration, or inflammation | 5 | 6 |
| Stridor | 4 | 5 |
| Nasal ulceration | 2 | 3 |
| Tooth avulsion | 2 | 3 |
| Tongue injury | 2 | 3 |
Partial laryngeal obstruction at extubation is most often related to laryngeal edema (see the section Early Complications After Extubation/Laryngeal/Edema). Laryngeal injury and other complications during self-extubation of an ETT with an inflated cuff have not been adequately studied. Surprisingly, few patients appear to develop laryngeal complications following self-extubation. Pulmonary aspiration may occur if extubation and suctioning techniques are faulty. The requirement for reintubation soon after extubation is usually caused by laryngeal edema or respiratory failure. Difficult extubation should be anticipated in patients whose intubation was difficult.217
This section discusses those complications of TLI that appear during roughly the first week after extubation. This period is dominated by symptoms of pharyngeal and laryngeal injury from TLI, including hoarseness, dysphonia, sore throat, cough, dysphagia, and odynophagia.
There are no specific new complications that develop in this time interval, but complications that began earlier may of course be observed.
Postextubation sore throat has been reported in up to 42%19 of ICU patients, similar to the frequency observed in patients who required TLI for general anesthesia.218,219 Persistent and severe dysphagia after extubation following prolonged TLI should alert the clinician to the possibility of active infection in the posterior larynx.
There may be a temporary loss of the gag reflex after extubation. This was observed in 24% of patients who had direct laryngoscopy within 24 hours of extubation, supporting the notion that some patients have a sensory denervation of the pharynx and larynx from TLI.52 Loss of upper airway reflexes increases the risk of aspiration.52 We found pharyngeal bleeding or ulceration in 9% of patients at extubation (see Table 39-6),19 although Colice et al did not report this complication after prolonged TLI.52
Prospective studies using fiber-optic laryngoscopy within 24 hours of extubation in the ICU setting have revealed laryngeal injury in 73% to 94% of patients.52,220,221 Colice et al performed direct fiber-optic laryngoscopy within 24 hours of extubation in eighty-two patients who had been intubated for 4 or more days (mean: 9.7 ± 0.6 days).52 Seventy-seven (94%) of their patients had laryngeal injury (42% mild, 29% moderate, and 23% severe). Nearly all patients had posterior true vocal cord ulceration. Laryngeal edema was present in the patients with moderate to severe damage. Two patients had such large ulcers that the vocal cords could not be adducted, permitting free aspiration into the trachea.52 Most patients who displayed initial laryngeal damage had complete resolution of laryngeal findings on laryngoscopy within 4 weeks after extubation.52 Kastanos et al reported the following early laryngeal lesions in nineteen patients after extubation: true vocal cord granulomas in eight (42%), true vocal cord ulcerations in seven (37%), true vocal cord paresis in one (5%), and subglottic edema in one (5%).128 Thomas et al performed fiber-optic endoscopy through the ETT just before extubation and found visible laryngeal pathology in 131 (88%) of 150 patients.222 Table 39-7 summarizes the important laryngeal complications after TLI.
|
In fifty-four adult male patients followed closely by Colice et al after TLI, thirty (56%) had significant hoarseness.52 Holdgaard et al observed hoarseness in 42% of ICU patients following nasotracheal intubation.105 Hoarseness following TLI usually resolves within a few days in most patients as laryngeal edema and inflammation subside and normal vocal cord adduction is restored.125 In some cases, transient postextubation hoarseness requires 7 to 10 days to resolve. Hoarseness persisting beyond 10 to 14 days suggests serious laryngeal injury such as granuloma formulation, vocal cord paresis or paralysis, or cricoarytenoid joint dysfunction, and requires the attention of an otolaryngologist–head and neck surgeon.
Postextubation laryngeal edema (see Fig. 39-11), an important complication of TLI, may occur at the supraglottic, glottic, or subglottic levels.8 It presents with postextubation stridor and dyspnea and commonly precipitates the need for reintubation. Laryngeal edema is observed immediately after extubation in approximately 40% of patients after anesthetic intubation and in a roughly a third223 to half of critical care patients.52
Postextubation laryngospasm in the recovery from general anesthesia is a well-known phenomenon. Although postextubation stridor in the ICU is sometimes attributed to laryngospasm, this complication after extubation of ICU patients is not well documented. Colice et al reported true laryngospasm in only one of eighty-two ICU patients within 24 hours of extubation.52 True laryngospasm following extubation of the critically ill patient should be distinguished from laryngeal edema and other more common causes of postextubation stridor.
A literature review by Wittekamp et al reported postextubation stridor in up to 30.2% of critically ill adults.144 Many studies have investigated postextubation stridor.19,52,224–226 Stridor occurring after extubation is usually inspiratory, indicating variable extrathoracic airway obstruction. Mackenzie et al observed severe stridor after prolonged TLI in 0.1% to 0.6% of patients.224 This complication was found to be caused by vocal cord edema or subglottic stenosis, not laryngospasm. Symptoms of stridor appeared from 5 minutes to 4 hours after extubation.224 Repeated intubations or tracheotomy were required in the majority of patients. Postextubation stridor should always indicate the possibility of subglottic stenosis at the level of the cricoid cartilage, a level that is particularly vulnerable to airway narrowing in children.
Laryngeal incompetence is common after extubation and has been attributed to a sensory impairment or mechanical dysfunction of the larynx.227 The frequency of aspiration secondary to laryngeal incompetence in postoperative patients ranges from 22% to 35%.227,228 Inability of the vocal cords to adduct increases the risk of aspiration.52,125
Unilateral vocal cord paresis or paralysis is a serious but uncommon complication of TLI.47,125,229,230 It presents in the early postextubation period as persistent hoarseness. Santos et al reported vocal cord immobility in sixteen (20%) of ninety-seven patients after extubation, and in half of these cases, a delayed presentation over a period of 1 to 10 weeks following extubation was observed.139 Others have reported vocal cord paralysis in less than 1% of cases.47 True bilateral vocal cord paralysis after TLI, which presents as severe stridor, is very rare.
Whited evaluated sixteen patients with vocal cord paresis or paralysis after TLI of 5 days or longer.125 Common features in these patients were symmetry of vocal cord paresis or paralysis, edema and erythema of the arytenoids and posterior commissure, median or paramedian vocal cord positioning, late return of vocal cord abduction, a tendency for aspiration to occur, and spontaneous recovery in nearly all patients within 4 weeks.125 Postextubation vocal cord paresis or paralysis may result from traumatic dislocation of the arytenoids,231,232 cricoarytenoid joint arthritis, cuff inflation immediately below the vocal cords resulting in compression of the anterior branch of the recurrent laryngeal nerves,233 or the mechanical effects of laryngeal edema and inflammation.108 Bilateral vocal cord paralysis from intubation injury may present with hoarseness and recurrent aspiration233 or with upper airway obstruction requiring immediate tracheotomy.
Hematomas of the vocal cords that occur during placement of an ETT apparently resolve by the time of extubation. They were not seen after extubation in eighty-two patients studied by Colice et al.52
Severe odynophagia or odynophonia after extubation should suggest the possibility of posterior glottic infection or cricoid cartilage abscess.108 Posterior glottic infection may result in destruction of laryngeal cartilage and predispose to posterior glottic stenosis.108
In a prospective study of nineteen patients, Kastanos et al reported finding tracheal granulomas in six patients (31%) and cuff-site tracheitis in three (16%).128 Tracheal pseudomembranes leading to airway obstruction in the first few days after extubation have been the subject of individual case reports.181,182
Specific bronchial complications of TLI in this time period have not been reported.
Pulmonary aspiration may occur with laryngeal incompetence after extubation.52,125,227 Pulmonary aspiration was observed after extubation in two (2.4%) of eighty-two patients after prolonged TLI in the series of Colice et al.52 This finding was attributed to vocal cord dysfunction and temporary loss of sensorimotor function of the larynx and pharynx.52 Burgess et al observed aspiration of swallowed contrast material in 33% of surgical patients immediately after extubation.227 Endoscopic evaluation of swallowing after prolonged TLI has revealed aspiration in 14%234 to 45%235 of patients.
Postextubation negative pressure pulmonary edema secondary to laryngeal or tracheal obstruction following TLI and prolonged forceful inspiration has been described in small case series or individual case reports.236,237
There are no significant miscellaneous complications of TLI in the early postextubation period.
Late complications of TLI, those appearing in the weeks to months after extubation, are usually the result of abnormal airway mucosal healing with fibrosis or granuloma formation. Laryngeal stenosis is the most serious of these events (see discussion below).
Nasal stricture and nasal septal perforation following prolonged nasotracheal intubation are rare.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree