Complications of Tracheostomies
Valerie Dobiesz, Samreen Vora, and Carissa Tyo
Tracheostomy placement is a mainstay in airway management of critically ill patients. A tracheostomy tube is placed because of mechanical obstruction, inability to clear secretions, or need for prolonged ventilation. A tracheostomy provides access for mechanical ventilation, clearance of secretions, and protection of the airway. Placement may be done in the operating room using an open technique, or at the bedside in the intensive care unit (ICU) using a percutaneous dilational tracheostomy (PDT) technique. This surgical procedure has been known for centuries, with references to this practice in Eber’s Papyrus (1550 BC) and the ancient Rig Veda texts (two of the three oldest known medical works) (1,2).
Complications of these devices range from minor inconveniences for the patient to life-threatening emergencies and may occur immediately postoperatively or may be delayed in nature. Complications include local bleeding, obstruction, infection, stenosis, tracheoesophageal fistula, pneumothorax, pneumomediastinum, air leaks, dislodgement, false passage, tracheostomy tube fractures with aspiration, and decannulation. Rarely, an extra-long tube can lead to right mainstem bronchus intubation recognized in the immediate postoperative period. The overall mortality rate is <1% with a total complication rate of up to 65%. A greater mortality rate and complication rate are seen in emergency situations, ICU patients, and pediatric patients (3,4). Because the tracheostomy tube is frequently encountered in the emergency department (ED), emergency physicians must be aware of the purpose, structure, and proper maintenance of these devices, so they will be prepared for complications.
HEMORRHAGE
Major hemorrhage during and soon after tracheostomy is rare but can be life threatening. Bleeding complications account for 20% of ED tracheostomy visits (5). There are numerous vessels in the vicinity that can bleed and cause problems, including the superficial blood vessels, thyroid vessels, carotid arteries, anterior jugular veins, and the innominate (brachiocephalic) artery. The lacerated thyroid gland can bleed, as can granulation tissue. Incisional or stomal bleeding may be controlled with cauterization or packing the wound with petroleum jelly gauze.
Of particular concern is the potential for a tracheoarterial fistula. This fistula is typically caused by erosion of the tip of the tracheostomy tube into the innominate artery, producing massive bleeding that is universally fatal if not recognized and treated immediately. Tracheo-innominate artery fistula (TIF) is reported in approximately 0.1% to 1% of surgical tracheostomy patients and 0.35% of PDT patients; moreover, delayed hemorrhage is underreported (6). Although rare, TIF has a mortality rate of 50% to 75% despite emergent management (5). The clinical presentation may include a sentinel bleed in the form of hemoptysis or mild bleeding at the tracheostomy site hours or days before massive bleeding occurs.
The ED evaluation should include a rapid assessment for airway patency and for signs of shock or coagulopathy. Basic laboratory studies and a type and screen are helpful in this regard.
The ED management should initially focus on resuscitation, if necessary. Vigorous resuscitation with isotonic fluids and possibly blood should be started for any brisk bleeding while emergent surgical consultation is obtained for definitive management. Bronchoscopy is the diagnostic method of choice. Temporizing measures should be attempted to control the bleeding, such as hyperinflation of the tracheostomy cuff to compress bleeding vessels against the sternal wall. If cuff inflation is unsuccessful, digital pressure should be applied to the anterior tracheal wall through the tracheostomy, compressing the anterior tracheal wall against the sternum until definitive care can be provided (7,8).
OBSTRUCTION
A patient with a tracheostomy who presents with respiratory distress must first be assessed for either a partial or complete obstruction of the tracheostomy tube. Patients with tracheostomies lack the humidification of air inspired by nasal passages, and this often results in thick, dry secretions. Improper care and maintenance of tracheostomy tubes in the outpatient setting are common. Mucus, inspissated secretions, blood, or dislodgement of the tracheostomy tube may cause life-threatening obstruction. Secretions may act as a ball valve, allowing air in but restricting outward ventilation (9).
The clinical presentation may range from slow, progressive shortness of breath to sudden obstruction and respiratory arrest.
The initial ED management should include verification of proper placement of the tracheostomy tube, with repositioning as needed. Treatment with high-flow oxygen should be initiated. Saline, hypertonic saline, or N-acetylcysteine may be used to help loosen secretions, followed by suction with an endotracheal suction catheter. Nebulized sodium bicarbonate raises the pH of secretions and weakens the saccharide structure of the mucus, and may offer an additive benefit when combined with nebulized N-acetylcysteine (10).
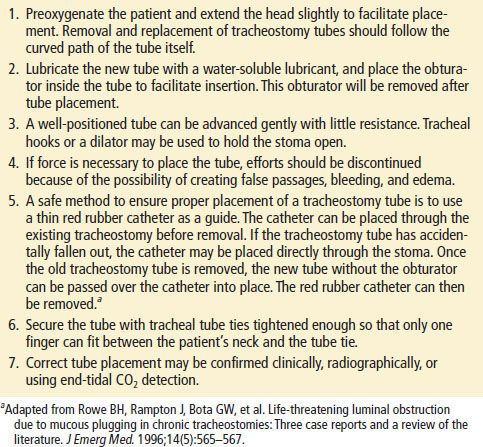
The inner cannula should be removed and cleaned, as this is a common source of obstruction. However, if the problem persists, the outer cannula should be removed and replaced with a new tracheostomy tube. Mechanical problems with the tube such as cuff leak or tube fracture may also necessitate tube replacement or consultation for bronchoscopy (9,11). Replacement of the tracheostomy tube in nonemergent circumstances is described in Table 72.1. However, the process may need to be abbreviated in the prehospital or emergency setting. A patient in respiratory distress not relieved by conservative methods such as suction, oxygen, and bronchodilators should be treated by immediate removal of the tracheostomy tube and tube replacement. Most obstructions occur in patients with long-standing tracheostomies, and those patients generally have uncuffed tracheostomy tubes that can be easily removed (12). If a new tracheostomy tube needs to be emergently replaced, the procedure may be simplified by passing a catheter or gum elastic bougie through the old tracheostomy tube and using it to guide the removal and replacement of the tube (12).
TABLE 72.1
Replacement of the Tracheostomy Cannula