125 Complications of Gynecologic Procedures, Abortion, and Assisted Reproductive Technology
• Complications with the highest morbidity and mortality are severe hemorrhage, serious infection, damage to intraabdominal structures, and pulmonary embolism.
• Complications seen in the emergency department are usually delayed in presentation, and often difficult to diagnose due to insidious onset, resulting in increased morbidity and mortality and a higher risk for litigation (i.e., ureteral injuries) High suspicion must be maintained.
• Emergency department bedside ultrasonography can provide rapid, early imaging for the evaluation of postprocedural patients, particularly unstable ones.
• Abortion is one of the most common procedures in the United States and overall has very low serious complication rates.
• Ovarian hyperstimulation syndrome is a potentially fatal complication of assisted reproduction in a generally healthy young woman. With no cure, early recognition, aggressive intervention, and close monitoring are key.
More than 146,000 cycles of ART were reported to the Centers for Disease Control and Prevention from 441 sites in the year 2009. In addition, approximately 600,000 hysterectomies are performed annually, which ranks it behind cesarean section as the most common major surgery in women of reproductive age.2
Complications of Gynecologic Procedures
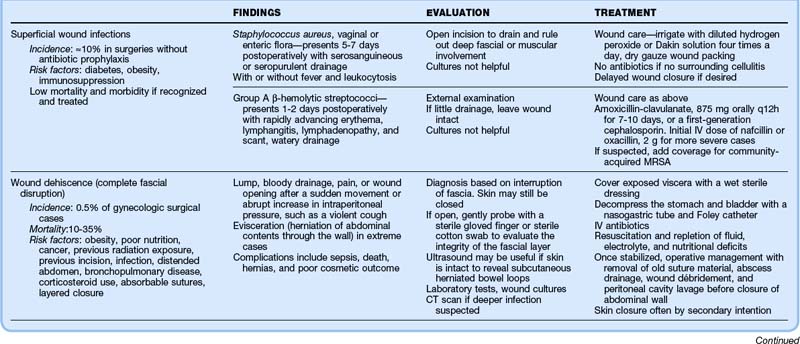
This section focuses on complications particular to gynecologic procedures that one might encounter in the ED setting and their evaluation and management (Fig. 125.1). Many complications of gynecologic procedures may go unrecognized before discharge, only to be seen later in the ED (Box 125.1). Box 125.2 lists the typical timing of these complications.
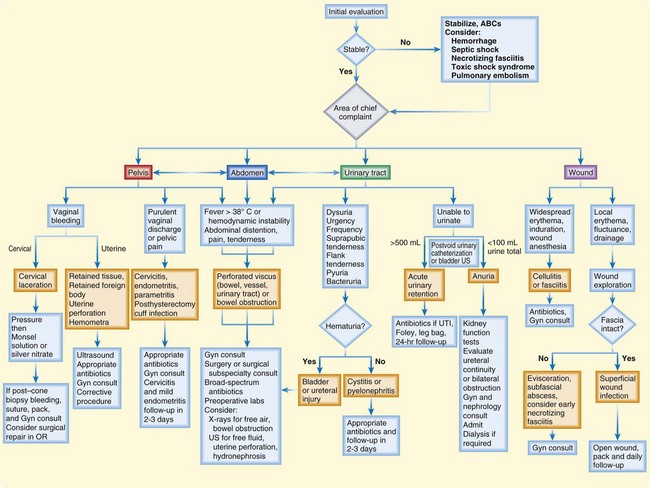
Fig. 125.1 Suggested algorithm for the evaluation and treatment of postoperative gynecologic patients.
Box 125.2 Complications of Gynecologic Procedures by Estimated Time Line
Differential Diagnosis and Medical Decision Making
For patients with complications after a gynecologic procedure, bedside ultrasonography (US) in the hands of a skillful operator can provide rapid recognition of intraabdominal and intrapelvic pathology. Possible ultrasonographic findings include free fluid heralding leakage from a perforated vessel, urinary tract, or viscus (Fig. 125.2); hydronephrosis as a result of ureteral obstruction; a full bladder secondary to urinary retention; fluid collections; and intrauterine contents. US can also be used to guide paracentesis for definitive fluid diagnosis or for the drainage of subcutaneous abscesses. It is important to remember that sensitivity and accuracy are very dependent on the user and interpreter and that anatomy, habitus, and elements such as bowel gas can greatly interfere with adequate imaging. US is a poor modality for evaluating the bowel or retroperitoneal space.
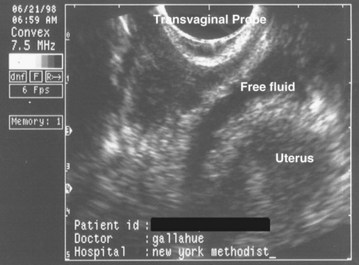
Fig. 125.2 Transvaginal ultrasound image showing free fluid in the cul-de-sac consistent with hemorrhage.
![]() Priority Actions
Priority Actions
Differential Diagnosis: Complications of Gynecologic Procedures
Abnormal Symptoms or Vital Signs?
Vaginal Bleeding—Is It Cervical or Uterine in Origin?
Unable to Urinate?
Wound Redness and Drainage?
Localized? If so, check the fascia; if it is intact, treat as a superficial wound infection with packing and close follow-up. If the fascia is not intact, consider a subfascial abscess, early necrotizing fasciitis, or hernia or evisceration; make sure that it is not an incarcerated hernia; gynecology consultation and possible surgical evaluation are required.
Widespread? Consider cellulitis or fasciitis; administer antibiotics and hospitalize the patient. If only mild cellulitis is present, oral antibiotics, very close follow-up, and explicit return instructions are required (consider priming with first dose of intravenous antibiotics).
CT, Computed tomography; ED, emergency department; US, ultrasound; UTI, urinary tract infection.
Urinary Tract Injury
The incidence of urinary tract injury in gynecologic surgery is between 0.33% and 4.8%. The great majority (80%) of these injuries involve the bladder. Ureteral injuries occur in just 0.3% to 1.0% of cases, but unilateral injury is discovered postoperatively in the majority of cases.3 This delayed recognition leads to increased morbidity. As a result, ureteral injury has become the leading cause of legal action against gynecologic surgeons.
Months to years after the procedure, watery drainage from the vagina heralds an ureterovaginal or vesicovaginal fistula, whereas watery wound drainage suggests a ureterocutaneous or vesicocutaneous fistula (Table 125.1).
Table 125.1 Clinical Findings and Bedside Diagnosis of Pelvic Fistulas
| TYPE OF FISTULA | FINDINGS | BEDSIDE DIAGNOSIS |
|---|---|---|
| Ureterovaginal | Copious, watery vaginal discharge; multiple urinary tract infections | |
| Vesicovaginal | Copious, watery vaginal discharge; multiple urinary tract infections | |
| Enterovaginal | Vaginal discharge may contain intestinal contents; severe vaginovulvar irritation may be present because of the pH | Acidity can be tested with litmus paper or the pH portion of a urine dipstick. Place a tampon in the vagina and administer oral activated charcoal. A stained tampon is diagnostic. |
| Colovaginal | Brown, feculent vaginal discharge | Place a tampon in the vagina and instill normal saline tinted with methylene blue into the rectum. A stained tampon is diagnostic of a rectovaginal fistula. Higher colonic lesions may be diagnosed by oral administration of activated charcoal. |
| Vesicocutaneous | Copious watery suprapubic wound discharge | Place a clean wound dressing and administer saline tinted with methylene blue into the bladder. A blue-stained dressing is diagnostic. To differentiate from ureterocutaneous fistulas, insert a urinary catheter, instill methylene blue via the catheter and clamp it off, wait  hour, and then drain the bladder until clear and perform the test described below. hour, and then drain the bladder until clear and perform the test described below. |
| Ureterocutaneous | Copious, watery wound drainage | Place a clean dressing and then administer methylene blue intravenously. A blue-stained dressing is diagnostic. |
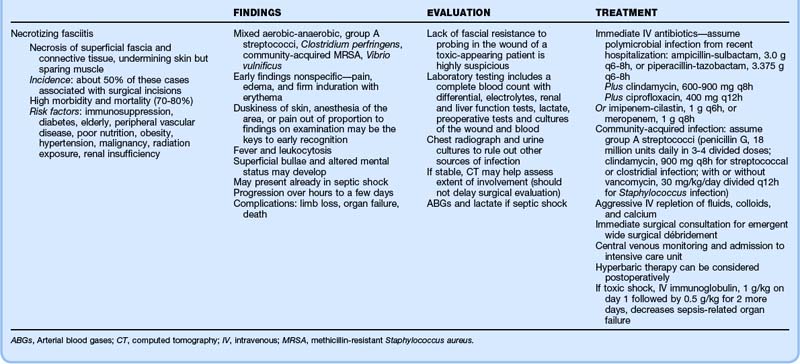
Wound and Abdominal Wall Infections
Thorough evaluation requires opening the wound for drainage and examination for deep fascial or muscular involvement. Superficial wound infections can be managed without antibiotics by meticulous wound care, irrigation with diluted hydrogen peroxide or Dakin solution four times per day, and dry gauze packing. Delayed wound closure can be performed if necessary. Table 125.2 details the clinical findings, evaluation, and treatment of wound infections, dehiscence, and necrotizing fasciitis.
Complications Specific to Laparoscopy
Laparoscopic procedures are characterized by more rapid recovery and lower complication rates than seen with open surgical procedures. However, unique complications are associated with needle or trocar insertion, induced pneumoperitoneum, and extensive use of electrocautery4,5 (Box 125.3). Most catastrophic complications are recognized intraoperatively. Management in the ED in the first month postoperatively is usually for wound complaints or symptoms caused by injury to the bowel, bladder, or ureters. Remote complications include hernias.
Box 125.3 Most Threatening and Most Common Complications of Laparoscopy Seen Postoperatively