Chapter 8 Common features of posturomovement dysfunction
The imbalanced activity between the deep and superficial muscle systems and between the flexor and extensor systems is expressed in a number of clinically observable altered features of postural and movement control, which appear to be more or less common in those with spinal pain and related disorders.
Defective antigravity support and control
A general or regional lack of axial extension control
The manner in which the spine is postured when upright highly influences patterns of trunk muscle activity.1 Conversely, patterns of muscle activity determine how the spine is postured. By and large people with spinal pain syndromes can move but they can’t ‘posture’ very well: if they manage to align the spine in neutral they have difficulty maintaining it in movement.
Poor pelvic base of support
The alignment and control of the spine in sitting, standing and bending forward is compromised, jeopardizing its safety. See defective pelvic control (p.170)
Common altered strategies for sitting and standing
The habitual adoption of poor sitting positions is probably the single most significant instigator and perpetuator of the postural and related movement dysfunction associated with the development of spinal pain and related disorders. In a modern industrial society long periods of sitting and relatively reduced general activity levels begin with schooling. The advent of computers and increasing sedentary work and leisure practices mean we do even more of it. Thecentral nervous system (CNS) is relatively starved of decent proprioceptive inputs and automatic responsesbegin to suffer (see Ch.11). Altered alignment changes the motor memory, affects muscle activation demand, the line of pull of muscles, creates the need for ‘holding patterns’ and leads to changes in the myofascial matrix.
Passive strategy
Sitting. The common strategy involves rolling back onto the posterior ischia and staying there. Repeated enough, the person begins to lose options for varied position change in sitting. Poor initiation and control of the base of support through the ischial tuberosities compromises the ability of the axial spine to adjust and move. This is particularly so when the commonly habitual strategy of crossing the legs is adopted. Even worse is ‘putting the feet up’ on stools or similar, often advised when the ‘circulation is bad’ which only serves to worsen it! The alignment and control of the whole spinal column is affected (Fig. 8.1).

Fig 8.1 • Passive collapse in sitting creates eccentric loading in the spine of a 15 year old (also in Fig 8.10).
Collapsed sitting switches off demand in the systemic local muscle system (SLMS), rendering the joints and soft tissues vulnerable. In ‘normal’ pain free subjects, slump sitting has been shown to decrease activity in the internal oblique and multifidus1–3 transversus and internal oblique,4 particularly if the legs are crossed5 or higher than the pelvis. Some normative studies have reported increased lumbar extensor muscle activity6,7 in slump sitting, yet the subjects shown in the study by Callaghan and Dunk7 are not in the position that most potentially or actually symptomatic subjects commonly adopt.
The posterior pelvic tilt creates hyper flexion of the spine8 – particularly over the lower levels, including the lumbosacral junction with well documented detrimental consequences. Cadaveric studies of lumbosacral motion segments have demonstrated the dramatic impact of increased segmental flexion on fatigue failure.9 Solomonow et al.10 showed induced flexion creep in feline viscoelastic tissues desensitized the mechanoreceptors and dramatically diminished muscular activity in multifidus. Later studies11 showed prolonged flexion results in tension-relaxation and laxity of viscoelastic structures, loss of reflexive muscular activity within 3 minutes and EMG spasms in multifidus and other posterior muscles. The spasms and muscular hyperexcitability in response to 20 minutes static loading even when very light loads were applied were still evident after 7 hours of rest12 and lasted for more than 24 hours.13 In addition, the micro-damage from sustained loading of the viscoelastic tissues results in time dependent development of inflammation14 setting the stage for chronic neural irritation and a plethora of referred symptoms of which pain is just one.
Usually, any attempts to ‘sit up straight’ are not initiated from the pelvic base of support but by intermittent systemic global muscle system (SGMS) activity of the muscle groups over the thoracolumbar junction.15 O’Sullivan2 draws attention to the critical role of pelvic position in determining spinal muscle activation patterns. ‘Holding oneself up’ is tiring and poorly sustained and so shortly the patient collapses again. In ‘normal’ subjects, significantly less superficial lumbar multifidus and internal oblique activity has been demonstrated in this postural strategy.16
The work of Solomonow and colleagues clearly demonstrates that a cumulative neuromuscular disorder develops because of repetition of static lumbar flexion, the severity of which is magnified by the number of repetitions. Full recovery of creep may not occur.17 O’Sullivan et al.18 showed a relationship between flexed sitting postures, reduced back muscle endurance, physical inactivity and flexion provoked low back pain. In sitting, twisting mobility significantly increases when the spine is flexed further increasing vulnerability of the posterior annulus to injury.19
Importantly, collapse of the lumbopelvic spine will affect the alignment of the rest of the spine including the head and neck, a fact which is often overlooked in some studies on cervicothoracic posture.20 It also contributes to the development of the shoulder crossed syndrome21 (see Ch.10).
In standing, the same postural pattern of posterior pelvic rotation is invariably carried through from sitting – the tendency being, to shift the pelvis forward with posterior rotation, hang off the iliofemoral ligaments in hip external rotation, with hyperextended knees and a collapsed spine. The sacrum is counternutated and L5 in relative flexion – an unfavorable loading state of the lumbosacral and SIJ region. This ‘locking’ of the lower limb kinetic chain limits the pelvis’ ability to be an adaptable and appropriate base of support for movement control of the spine. Further, when the pelvis is shunted forward, there is reduced lumbopelvic SLMS demand. Snijders et al.22 showed posterior pelvic rotation decreased activity in internal oblique. There is little buoyancy or ‘lift’ in the axial column or through the pelvis-leg base of support– the whole SLMS is relatively ‘switched off.
Overactive strategy
Sitting. The person ‘holds himself up’ (Fig. 8.2) – from extensor system dominance and often also as a result of a mistaken belief that it is ‘good posture’ to do so. This is generally achieved by more consistent over activity of SGMS muscles – particularly the extensor groups over the thoracolumbar junction.3,15 However, control of the pelvis as an effective and adaptable base of support for the axial skeleton is still deficient. Dankaerts et al,23 using an electromagnetic measuring device, examined sitting postures in those low back pain subjects who actively extend in sitting and reported an increased lumbar lordosis. While the low lordosis was reported as greater than the controls, it is suggested that clinically, even this group usually demonstrate reduced intersegmental joint play into extension over the lower levels when assessed by skilled palpation. Appearances can be deceptive. In a radiographic study, Roussouly et al.24 showed that while lordosis was increased, segmental extension between L5 and S1 was reduced. In the main, reduced extension over the lower levels (relative to the upper levels) and associated deficient intersegmental neuromuscular control is clinically apparent.
The superficial muscle overactivity reduces the ability to posturally adjust and shift weight over the support base. Intentionally stiffening the trunk by co-activating the superficial muscles has been shown to degrade postural control in unstable sitting.25
Standing. The standing overactive patterns are again a reflection of the sitting posture patterns – primarily relying upon dominant activity of thoracolumbar extensor groups and related considerable underactivity of the anterior abdominal wall. The thorax is shunted forward in relation to the pelvis. In an important and really nice ‘normal’ study, Harrison et al.26 demonstrated that anterior translation of the thorax resulted in posterior displacement and anterior tilt of the pelvis with extension of the upper lumbars and flexion of the lower lumbars. Reduced SLMS activity in the lower pelvic unit means that the dynamic base of support through the pelvis-leg kinetic chain is still inadequate.
The superficial muscle hyperactivity splints the spine and further disallows it to adequately prepare for, dissipate and dampen the forces created by head movement breathing and particularly in response to limb movements. Reduced segmental adjustments mean balance suffers. Mok et al.27 showed decreased preparatory and resultant increased correctional lumbopelvic movements in response to rapid arm movements. Smith et al.28 experimentally induced low back pain and found reduced motion of the trunk associated with breathing.
The tendency to uneven patterns of control is also apparent in the asymptomatic population as Gregory and Callaghan29 found when ‘university population’ subjects stood for 2 hours as they performed four light manual tasks. 13 of the 16 subjects developed some level of low back pain during that time. One of only three variables to significantly change was an increase in lumbar spine flexion. When central support is reduced because of inadequate deep local muscle system activity, the person is forced to rely more on abnormal SGMS activity in low load activities. Gregory et al.30 had a group of college students stand for 2 hours and found that those who developed substantial back discomfort showed greater superficial extensor trunk muscle activity at the beginning and end of the standing period with further increased responses to sudden trunk perturbations. After discomfort developed, the superficial abdominal activity also increased.
Defective pelvic control
In the clinical setting, it is an almost universal finding that those people with spinal pain and related disorders demonstrate to a greater or lesser extent, inadequate neuromotor control of the pelvis in many, if not all, of the different aspects of its functional movement repertoire. This affects pelvic joint kinematics and transmission of forces and loads through the pelvis. Joint findings generally reflect the movement difficulties. Mechanical dysfunction of the pelvic joints is generally in the form of a ‘functional biomechanical block’ where ‘distorsion’ is reduced or fixed. This may not necessarily be directly pain producing but is accompanied by associated signs when palpating the ligaments and myofascia and for joint ‘play’. This ‘functional block’ may be symmetrical or asymmetrical and affects segments higher up and down the kinetic chain. Pelvic asymmetry has been shown to create functional kinematic compensations not only in the lumbar spine but also in the thoracic region.31 Pelvic dysfunction acts as a potent and important contributor to the development and perpetuation of many lumbopelvic and related pain disorders including hip and knee pain as well as underpinning a lot of mid and upper torso dysfunction syndromes.
Defective intrapelvic control (refer to Ch. 6 Part B)
Inadequate control of Lower Pelvic Unit (LPU) muscle synergies result in difficulty performing the Fundamental Patterns of Pelvic Control. Attempts to do so invariably utilize strategies involving a lot of SGMS activity – either from large pelvi-femoral muscles and/or those higher up the torso normally responsible for controlling the relationship between the thorax and pelvis. Manual movement testing predictably reveals patterns of joint hypomobility which are also reflective of the motor control difficulties.
Fundamental Pelvic Pattern 1 (FPP1)
FPP1 is consistently the pattern that most if not all have little idea of the action and the most difficulty performing. Low lumbar segmental movement into extension is generally reduced with underactivity in multifidus, lower transversus, internal oblique, iliacus and probably psoas. The prime movers responsible for FPP2 are generally hyperactive and do not adequately eccentrically lengthen further hindering the proper performance of this pattern. Instead the action is more likely attempted by activating the thoracolumbar erector spinae, serratus posterior inferior higher up around the mid torso – a bilateral ‘posterior cinch’ which serves to ‘fix’ the thoracolumbar segments, thrust the lower anterior pole of the thorax forward and limit diaphragm activity and basal chest expansion. This may be overt or subtle yet readily discernable by palpation (Fig. 8.3). Because of difficulty with or habitual non use of this pattern, the pelvis is generally more posteriorly rotated, the sacrum counter-nutated and posterior hip opening is reduced as is low lumbar extension and control.
Fundamental Pelvic Pattern 2 (FPP2)
Generally this movement seems easier though appearances can be deceptive. Commonly, poor eccentric co-activation from those muscle groups with a prime role in FPP1 means there is imbalance in the force couple producing the movement. Principal activity involving the pelvic floor and obturator group including piriformis, is augmented by the tendency to create the habitual ‘dysfunctional posterior pelvic tilt’ by pushing through the feet, clenching the buttocks or ‘butt gripping’32 with associated overactivity from hamstrings. The underactivity of the lower abdominals is associated with over activity of the upper abdominals in some subgroups (Fig. 6.30).
Defective spatial control of the pelvis
Normally, the lumbopelvic stabilizing muscles including the pelvic floor are active when maintaining optimally aligned erect postures.1,3,33 Hodges34 states ‘there is considerable debate as to whether pelvic and lumbar positions are different in low back and pelvic pain although changes have been identified in specific subgroups’. Clinical observation reveals definite patterns of altered spatial position and control and this is described.
Sagittal plane
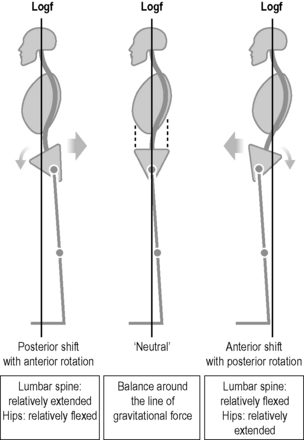
Here the observed preference is to posture and initiate subsequent movement from either an anteriorly or posteriorly shifted spatial relationship to the vertical neutral. The habitual preference for either forms the basis for a clinical classification system based on altered function (see Ch. 9). While whole synergies of muscles control the spatial position of the pelvis, psoas appears to play a large role. When underactive the pelvis shifts forward and when overactive it shifts back. The postural shift is always accompanied by a coexistent sagittal rotation as shown in Figure 8.4:
While the anterior and posterior pelvic shifts and associated sagittal rotations are clinically apparent, there is little acknowledgement found in the literature except in a personal article by Schleip on the structural typology of Hans Flury.35 In a very recent paper, Brumagne et al.36 discuss the inconsistent results in the small amount of studies which report altered body inclination in relation to postural control. Two studies found a more anterior centre of mass36,37 with related increased back muscle activation, while two others reported a more posteriorly located centre of mass.38,39 Clinical classification into the two primary pictures of dysfunction may help explain these diverse findings (Ch. 9).
Coronal plane
The postural habit of passively ‘hanging’ the body predominantly on one leg is common and partly contributes towards the high incidence of hip ‘bursitis’ (Fig. 8.5). Reduced LPU activity subsequently affects the ability to laterally shift weight through the hip joints; either the pelvis over the weight bearing leg, or the leg medially under the pelvis. Instead control is attempted higher up via a bilateral ‘cinch’ which then affects the spines ability to posturally adapt in the coronal plane and maintain three dimensional control of its alignment.
Horizontal plane
Diminished control of backward and forward pelvic rotation affects adaptive postural pre- positioning of the pelvis to support lower limb movements as well as rotation in the horizontal plane and related spinal rotation. Gracovetsky draws attention to the importance of pelvic rotation in walking.40 Tightness and/or imbalance in the hip rotators, particularly tighter external rotators, limit transverse plane pelvic rotation. A combination of reduced intrapelvic rotation or ‘distorsion’ and reduced rotation of the pelvis as a whole on the hips means that the mid lumbar spine becomes the site of relative rotary flexibility. Because of the poor spatial control, the pelvis is easily shunted around and movements of the hips invariably end up being movements of the low back.
Poor pelvic control affects the ability of the sacrum to direct alignment and control of the rest of the spine
Regional or general reduction of the lumbar lordosis is universally common clinically,41 and as noted by Adams et al.42 particularly in the lower lumbar spine. Poor control of anterior pelvic rotation and the habitual adoption of posterior pelvic rotation or tilt means the sacrum is carried into flexion and the lumbosacral region moves more into relative flexion in posture and movement. Generally, closed chain hip flexion and open chain hip extension are more difficult. Both rely on control of sagittal anterior pelvic rotation which is coupled with lordosis in the lumbar spine. The importance of being able to control posture and movement around the neutral lordosis for a healthily functioning spine is acknowledged by clinicians and has been stressed by noted researchers such as McGill43 and Adams.42 Loss of control of the neutral lumbosacral position jeopardizes local segmental control,44 and also transmission of the movement wave and control up and down the whole axial spine, including coupled rotation and side bending amongst other things.
Altered control of sagittal pelvic tilt generally reflects imbalanced activity between the iliopsoas and obturator/hamstrings groups
Sagittal tilting movements of the pelvis on the femur are the largest and most employed in functional movement. It is necessary that each muscle in the LPU synergy works enough but not too much so each can effectively contribute to the synergy and co coordinated movement patterns ensue (see Ch. 6).
The relationship between back pain syndromes and hypo or hyper tonus of iliacus and psoas is understood by clinicians yet there is a dearth in the literature. Mostly considered as open chain hip flexors,45 a postural stabilizing role is increasingly accorded to psoas46–49 particularly if hip flexion is part of the movement.50 Except for inclusion with psoas as the ‘iliopsoas’, iliacus barely rates a mention. However the two muscles differ anatomically, neurally and functionally.50 Andersson et al.47 demonstrated individual and task specific activation patterns between iliacus and psoas which varied according to the particular demands for stability and movement at the lumbar spine, pelvis and hip. The scant attention paid to iliacus in the literature is indicative of paucity in the understanding of functional movement control around the lumbopelvic region. Both these muscles provide important internal bracing of forces and movements within the pelvis51 including stability of the sacroiliac joint as well as controlling the pelvis on the femur and the alignment and stability of the spine over the legs. Unilateral spasm of iliacus and psoas can contribute to a fixed intrapelvic ‘distorsion’.52,53
The influence of the deep external hip rotators on modulating pelvic tilt control is practically nowhere to be found in the literature. Their influence is also important in transverse plane rotation of the pelvis on the fixed femur.
Imbalance in the ‘swing’ is also reflected in the position of the hips. When the obturator group dominates, the hips are more externally rotated and internal rotation is reduced. When the iliacus/psoas are tighter (less common), the hips move more freely into internal rotation and less into external rotation. Both groups can be tight where the neutral rotation position is more balanced but range into rotation, flexion and extension is more limited (see Ch.10 ‘Mixed syndrome’).
When adaptive pelvic tilt support for functional spinal movement is insufficient, compensatory regional hyperactivity around the centre of the body is seen, serving to further limit spinal control mechanisms as the region becomes hyperstabilized. Increased activity in the superficial abdominals is increasingly reported30,54–57 as well as extensor hyperactivity30,58,59 (see Ch. 10, ‘Central cinch patterns’).
Difficulty controlling closed chain movements of the hip joint and subsequent effect on lumbar spine (see Ch. 6, Part B)
It is interesting to ponder the manner in which we personally and conceptually view dysfunction. The noted researcher McGill states ‘I am continually surprised at the number of people with back troubles who also have hip troubles’.50 They are always interrelated; and emanate from defective pelvic control. The huge numbers of people with back pain and those increasingly undergoing hip replacement surgery attest to the extent of the communal dysfunction.
Sagittal plane
Forward bend pattern
Ideally this is achieved from a ‘pelvic swing and shift pattern’ based upon FPP1 (see p.127). However, habitual buttock clenching and not ‘letting go’ of the posterior pelvic floor60 and pelvi-femoral muscles contribute to difficulty initiating and controlling this action from the pelvis. Instead the pelvis commonly rolls into posterior rotation where the sacroiliac joint and the mid/low lumbar spine levels are the victim as they are pulled into hyper flexion to compensate (Fig. 8.6). This is common and has also been described as a ‘click-clack’ movement.5,61The sacroiliac joint is especially prone to shear forces if loaded in the counter-nutated position.71
Roussel et al.62 described a study which found that reduced control of this pattern in dancers as a basis for performing open and closed chain hip flexion was predictive of risk for developing future musculoskeletal injuries. A large epidemiology study by Vingård et al.63 found the strongest risk factor for LBP of biomechanical origin in men was working in a forward bent position. It makes no sense to attempt to ‘stabilize’ the lumbar spine – or the sacroiliac joint for that matter, if they are being constantly forced to abnormally compensate for movements which should be initiated from the pelvis during our many and varied activities of daily living. The disinclination to shift the pelvis posteriorly and weight bear through a flexed hip is also apparent in kneeling, all fours and variations of these positions. In fact loading weight through a flexed hip in any position such as supine is usually challenging e.g. ‘bridging’ is generally only achieved by posterior pelvic rotation. Achieving functional lengthening in the hamstrings and obturator group can only occur when the pelvis can be controlled in anterior rotation.64
Lifting or return from forward bend pattern
Ideally this is based upon control of FPP2 which brings the pelvis forward and extends the hips while balanced activity of the flexors and extensors controls the ‘body cylinder’ alignment. When control is defective, the patient tends to principally rely upon the hamstrings and passive tension in the posterior myofascial structures with the spine in flexion and posterior pelvic rotation or conversely, he excessively relies upon the back extensors (see Ch.9).
Transverse plane
In the transverse plane it is common to see:
Cibulka et al.65 found subjects with sacroiliac joint pain has significantly more hip external rotation with a limitation of internal rotation on the side of the posterior innominate.
Coronal plane
In the coronal plane, reduced control of the LPU and lateral and medial weight shift at the hip engenders the need for holding patterns higher up in the torso or for excess activity in the large pelvi-femoral muscles. Underactivity in iliacus-psoas reduces control of lateral weight shift while overactivity disrupts the neutral pelvic position and feeds into central ‘cinch posterior cinch’ behavior (Ch.10; Fig. 8.7). Reduced intrapelvic control provides a less stable base to support well controlled activity of the large SGMS pelvifemoral muscles – in particular the adductors and hamstrings both of which are notorious for ‘sprains’. Mens66,67 draws attention to the fact that ‘adduction-related groin pain’ in the athlete may not be caused by adductor tendonitis but by instability of the pelvic ring. In a study of 44 athletes with groin pain clinically elicited by resisting the adductors in crook lying, he then applied a pelvic belt placed inferior to the iliac spines and just above the greater trochanter. Subsequent retesting generally but variably improved adductor force and lessened pain during the maneuver. It is suggested that the pelvic belt is performing the action that would otherwise be provided by the synergy of the LPU in performing the first fundamental pelvic pattern. In particular the lower abdominals and iliacus provide intrinsic medial stability of the upper pelvic bowl and ipso facto mediolateral stability of the inferior bowl to support actions of the large pelvifemoral muscles. He notes the strong association between groin pain and abdominal wall weakness. He also describes67 two other studies where cases of osteitis pubis, instability of the symphysis and adduction related groin pain were treated either by surgical fusion of the symphysis or intraarticular injections into the symphysis with improvement in the adductor related groin pain. Increased adductor tension/activity possibly not only causes tendonitis but overstress of the ligaments of the joints of the pelvic ring.
Three-dimensional control of closed chain movements of the hip is not only critical in being able to functionally move at the hips but is also particularly important when ‘stretching the hips’. The ‘catch 22’ is that the hips are tight because of poor control of the fundamental patterns, yet often, subsequent hip stretching is performed as ‘stupid stretches’ (Fig. 8.8) with no attention paid to initiation and control from the pelvis. The lumbar spine is generally pulled into end range flexion or extension and rotation and becomes the site of relative flexibility68 and even more vulnerable, setting up a vicious cycle where the dysfunction is perpetuated. This is particularly so in the case of tightness of the hamstrings and piriformis (see the ‘hamstrings/hip conundrum’ (Ch.12).

Fig 8.8 • This common stretch perpetuates her problem. Note the axis of movement in the stretch is the lumbo pelvic junction rather than the hip. See Fig 8.26 and text.
Reduced pelvic control at the hip particularly during dynamic single leg exertions has also been associated with patellofemoral pain syndromes.69
Impaired movements of the femur on a stable pelvis
Movements at the hip are generally better understood and considered in terms of ‘open chain’ movements – the pelvis providing a stable platform for the moving femur. This is also an important component of pelvic function and most contemporary rehabilitation strategies do focus on this aspect. However attention to the ability to control sagittal pelvic rotation and the neutral lumbar lordosis, as well as isolating the movement to the hip is frequently overlooked in practice. Reduced lumbopelvic or intra/extra pelvic control means that the pelvis is an ineffectual platform to support open chain hip movements. This is particularly important with large long lever actions of the leg such as the ASLR test and particularly so if they are ballistic as in kicking a football. The lumbar spine again becomes overstressed setting up a vicious cycle where the dysfunction is perpetuated. Tightness of the pelvifemoral muscles further compounds the problem. This helps explain the prevalence of various ‘diagnoses’ of hamstring problems in the sporting arena – pulls, tightness, tears, tendinopathies etc. is (see ‘The hamstrings conundrum’ Ch.12).
The close functional relationship between hip–pelvis myomechanics
The more common patterns of habitual posturomovement tend to underutilize available hip range of movement and control and certain patterns of movement become more prevalent. Reduced activity and imbalance within the LPU and an over reliance on the outer SGMS muscles affects intrapelvic stability and control e.g. dominance of rectus femoris over psoas for hip flexion; of TFL over gluteals for abduction. The tendency is to ‘hang’ relying on the ‘outer’ muscles rather than find ‘inner’ support. The neuromuscular predominance of closed chain hip extension, abduction external rotation patterns with reduced antagonist activity, causes the inferior pelvic bowl to become hyperstabilized and more ‘closed’ and the sacrum counternutated. Altered loading stresses and reduced ‘distorsion’ in the pelvic ring ensue. Articular and neuromuscular freedom of patterns of hip movement into various combinations of flexion, internal rotation and adduction and related opening of the inferior bowl begin to show restriction. This limits closing of the superior bowl and control of the lumbar lordosis. Clinically, this is more common (Fig. 8.9).
Sacroiliac Instability?
Vleeming et al.70,71 considered that the articular surfaces of the sacroiliac joint (SIJ) were relatively flat and as large forces needed to be transferred across the joints, they were potentially unstable. They introduced the notion of a self locking or self bracing mechanism which acted to stabilize the joint. This model comprised a combination of ‘form closure’– the specific anatomic features of the joint, and ‘force closure’ – compression generated by lateral muscle forces and ligaments with friction, in order to withstand potential shear at the joint from gravitational forces and during load transfer. Nutation of the saccrum is crucial in this self locking mechanism and tensions most SIJ ligaments.70 The four muscles they listed as specifically important in providing joint compression were erector spinae, gluteus maximus, latissimus dorsi and biceps femoris. Through their attachments including those to the thoracolumbar fascia, they were considered to form part of three muscle slings: the longitudinal, posterior oblique and anterior oblique slings (see p.121) which acted to compress the joint70and provide support. Van Wingerden et al.72 managed to show that sacroiliac joint stiffness did increase when individual muscles were activated, especially the erector spinae. Failure in the system is said to occur when erector spinae and gluteus maximus become weak with an increase in hamstrings tension which serves to hold the sacroiliac joint in counternutation, and so more vulnerable to shear forces in loading.70 Note that practically all these muscles belong within the SGMS and are not intimately related to pelvic ring myomechanics, hence are unlikely to provide a truly effective postural pre-stabilizing role to support integrated load transfer through the pelvis. As those authors suggest, the superficial slings will play an important role in gross motor activities such as walking and running, but it is suggested only if they are able to act on a stable base of support provided by deep system preactivation. With the benefit of more recent evidence by Australian researchers73–77 into function of various muscles within the deep system, the authors later suggested including the contribution of ‘core muscles’ to the self bracing mechanism.71
The instability model was further developed when in 1999 Mens et al.78 published a paper which showed that impairment of the active straight leg raise test (ASLR) correlated strongly with instability of the pelvic ring in patients with peripartum pelvic girdle pain (PPPGP). The increased mobility was demonstrated on X-ray and occurred at the symphysis pubis and was most evident when passively hanging the symptomatic leg while standing on a raised box. The ASLR was improved by the application of a pelvic belt either just below the anterior superior iliac spines or at the level of the symphysis pubis. This external compression provides pelvic ring stability either above or below the hip joint. The researchers surmised that the caudal shift of the pubic bone seen on X-ray was possibly caused by an anterior rotation of the innominate about a horizontal axis near the sacroiliac joint. However, normally, weight bearing is considered to produce a posterior rotation of the weight-bearing innominate while the superincumbent body weight causes the sacrum to nutate.79,80 It can be reasoned that hanging the contralateral leg will produce further physiological ‘distorsion’ in the pelvic ring. If the pelvic ring is unstable at the symphysis, this will ‘appear to be’ excessive anterior rotation of the free innominate. While this study does show instability at the symphysis it does not necessarily show it at the SIJ. However, largely through it, a positive ASLR has somehow become construed as indicative of ‘SIJ instability’.
Furthermore, clinically there is also a danger that pelvic girdle pain and the associated finding of a positive ASLR test have become readily interpreted as confirming ‘sacroiliac instability’. This author agrees with O’Sullivan56 who suggests many clinicians hold confused beliefs that the pelvis is unstable or displaced, which are then transferred to their patients with unfortunate consequences. While Mens et al.78 found a strong correlation between positive ASLR and actual demonstrated pubic joint laxity in PPPGP, the test can also be positive in cases of pelvic joint stiffness. Clinically in a general population, the joint is more often symptomatic because of stiffness which may or not be directly pain producing. Pain provocation tests are not necessarily clinically reliable and it is generally necessary to apply composite tests to arrive at a diagnosis.81 Examining the quality and ‘feel’ of the tissues and specific movement testing of the spinal, hip and pelvic joints including control of key functional movement patterns without necessarily reproducing ‘the pain,’ generally delineates the source and reasons for the pain and informs appropriate treatment direction. O’Sullivan et al.77 identified altered motor control in subjects who had pain over the sacroiliac joint, positive pain provocation tests and a positive ASLR. During the active ASLR test, not only did the pelvic floor descend but this was associated with bracing and decreased descent of the diaphragm and alterations in respiration which improved with external pressure over the ilia. Rather than necessarily indicating ‘sacroiliac instability’, this study nicely showed that it is the operant suboptimal motor control strategies of the whole torso that are ‘unstable’ in many with pelvic girdle pain syndromes.
The Netherlands model of ‘sacroiliac instability’ has been popular and adopted by clinicians 32,82,83 and researchers.84–86 An improved understanding of function in the deep system has led to the inclusion of those muscles responsible for generating IAP, also considered to have a role in maintaining pelvic stability and respiration (transversus, internal oblique diaphragm and pelvic floor).77 However, highly significant is that apart from the pelvic floor and piriformis muscles, the influence of the very functionally important ‘other internal pelvic muscles’ – the iliacus and obturator group have to date not yet been well considered. Andersson et al.47 showed that during ASLR, moderate to high activity was present for both psoas and iliacus. Clearly they contribute to providing internal support for load transfer through the pelvis. Eminent clinicians87,88 describe spasm of iliacus as a potent factor in maintaining sacroiliac dysfunction. In the Mens study the raised leg was ‘relaxed in lateral rotation’.78 Clinically, preactivation of the FPP1 with the hip in neutral rotation can impressively change the ASLR test result. Interestingly, in an earlier paper documenting the results of a survey of 518 women with PPPGP, Mens et al.89 noted the high frequency of delivery positions with a bent spine. They concluded a flexed position during delivery may enhance the risk for PPPGP. Post partum tasks involve constant flexion patterns, undoubtedly further feeding the dysfunction.
Gracovetsky90 refutes the Netherlands ‘instability model’ suggesting that there is an evolutionary advantage to instability – function drives the anatomy and not the other way around; ‘the viscoelastic nature of biomechanical material precludes straightforward application of these engineering concepts’. Even a steady erect stance is maintained by cycling through a sequence of different but closely related postures so that no one structure is continuously loaded. He proposes a ‘SG ridge’ on the sacrum locks into a corresponding shape in the innominates allowing coupled motion similar to that seen in the lumbar facets, but of smaller magnitude though greater force. The SG ridge acts as a fulcrum transferring the vertical loads, leaving the SIJ relatively free to rotate around the hinge in two planes, thus allowing axial rotation of the pelvis and nutation. The joint surfaces are warped and so do not slip past each other; the ligaments are strong and the geometry of the joint is such that there is no need for additional force closure to keep it together. The spine needs to be impulse loaded40 with oscillating load sharing roles between the passive and active tissues.
Neuromyo-articular dysfunction of the spinopelvic–hip complex underlies most pelvic girdle pain and related disorders
Pain in the pelvic girdle can either arise from the local joints or myofascia including the hip, or be referred from the spine or manifest from a combination of the above. Groin pain in the sporting population can be associated with pathology in the hip, pubic symphysis91 and associated dysfunction in the lumbar spine and SIJ. While traumatic injuries including childbirth can precipitate the development of symptoms, more often than not their onset is insidious, seemingly occurring for no apparent reason. The pelvic organs receive sympathetic supply from the thoracolumbar outflow while the parasympathetic is via the sacral outflow. It should also be borne in mind that psoas is innervated by L12394 and iliacus by L2394, and the adductors by L234.94 Spasm in iliacus can result from L23 and/or SIJ dysfunction. Palpation of joints over the thoracolumbar spine can reproduce scrotal, haunch, hip and pelvic pain. The functional relationship between the thoracic and pelvic diaphragms means that clinically, thoracolumbar dysfunction is usually part of the dysfunction picture in many pelvic girdle pain disorders. Clinical assessment readily delineates underlying patterns of neuromyo-articular dysfunction precipitating and perpetuating symptoms. In an excellent review synthesizing current evidence with clinical observation, O’Sullivan and Beales56,92 make the case for clinically classifying and diagnosing pelvic girdle pain disorders based upon the dysfunctional mechanisms underlying the disorder. Currently, theories about the sacroiliac joint are popular yet confused and poorly validated, and these authors attempt to clarify the known facts. Importantly they suggest that ‘directional strain’ may be more significant than positional changes. In agreement with these authors, clinical findings generally delineate patterns of both neuromuscular hyperactivity and hypoactivity with a tendency for two main clinical subgroups. Those they classify as having ‘reduced force closure’ fairly much equates to the anterior pelvic crossed syndrome group (APXS; see Ch. 9) while those with ‘excessive force closure’ bear similarity to the mixed syndrome (MS; see Ch.10). Assessing and redressing joint function and activation and control of the fundamental pelvic movements and functional patterns generally ensures symptom amelioration.
Postural asymmetry of the pelvis
Clinically this is quite common87,88 even in children, where Lewit found approximately 40% prevalence in children from nursery school age onwards. The asymmetry may be directly or indirectly responsible for the patient’s symptoms. Lewit87 considers that pelvic distortion is always secondary to some other lesion which must be found and treated, atlanto-occipital joint dysfunction being common, particularly in children. As Lewit87 describes it: viewed from behind, the pelvis deviates slightly to one side (usually the right) and is slightly rotated (usually to the left). There is a fixed ‘distorsion’ where one innominate is anteriorly rotated against the other (usually the right) where the PSIS is higher and the ipsilateral ASIS is lower. Related to this is the ‘overtake’ phenomenon where in forward bending in sitting or standing, the lower PSIS (usually the left) overtakes the other becoming more cranial for about 20s after which the two spines return to a symmetrical position. There is usually muscle imbalance in the pelvic region and spasm of iliacus is frequent on the side of the lower PSIS, gluteal muscle bulk and activity is usually asymmetrical as is PFM activity. Clinically, the side of the lower PSIS is usually the painful side.88 When torsion is present the leg lengths appear unequal.88
Pelvic floor dysfunction
Effective function of the pelvic myofascial floor requires the ability to coordinate the static, ‘opening’ and ‘closing’ actions appropriate to the combined situational demands of breathing, continence and posturomovement control. Much of the interest generated in pelvic floor function stems from the problem of stress urinary incontinence (SUI). A recent longitudinal study by Smith et al.93 provides evidence of a relationship between back pain, incontinence and respiratory problems, suggesting a common underlying mechanism.
Pelvic floor and continence
Good coordination is required between the pelvic diaphragm (levator ani and coccygeus94) and the urogenital diaphragm as the floor may need to open spatially in movement such as the dancer’s high kick, while the sphincters remain closed. Pelvic posturomotor control dysfunction is likely to have consequences for the continence mechanism.34 When the pelvic floor muscles (PFM) lose their automatic coordinated function, it is the timing of muscle recruitment, as well as the endurance and strength which is deficient95 and activation may be asymmetrical.99
The incidence of stress incontinence is, or apparently was, low in Chinese women and cadaver studies have shown better developed levator ani muscle mass when compared to occidentals. This was attributed to hard work, minimal obesity and squatting.95 Altered spatial control of the pelvis and its inclination affect the gravitational forces acting on the floor33,96 and the line of pull of the muscles. When habitually forward and posteriorly tilted, postural demand is reduced. Increased sustained vertical loading on the PFM and increase stretch weakness is likely.97
A close functional interrelationship exists between the PFM and the abdominals and co-activation has been shown.98 Given the underactivity of the entire abdominal wall in some groups reasoning suggests probable associated underactivity of the PFM.
An association between uterovaginal collapse and decreased lumbar lordosis has been described.99 Similarly, postural collapse has been shown to relate to decreased PFM activity.100 Lordosis facilitates activation.57,95,100 Incompetent PFM response to sudden increases in IAP have been observed to be greater in spinal flexion in both sitting and standing.95 Poor tonic PFM activity is likely if tonic holding ability in transversus is reduced.33 Carrière101 notes weakness of the PFM can occur from damage to the pudendal nerve from heavy falls onto the bottom, and if the parasympathetic nerves are also injured, various pain syndromes can also occur. SUI has a general connotation of a ‘weak pelvic floor’ and the need to strengthen it. While low muscle tone, reduced or delayed activity may relate to prolapse102 and defective sphincter control,32 subjects with SUI can also have EMG-demonstrated increased activity of all the PFM.57,95 This is related to problems in the coordination and timing of activity between the abdominals and PFM57,103 The abdominal activity can be either decreased or increased. When decreased, the increased PFM activity is probably more likely in those who attempt to control the pelvis by the posterior inferior pelvic force couple (see Altered control of sagittal pelvic tilt p.173) with or without buttock clenching and related underactivity of the lower or entire abdominal wall. The obturator group is hyperactive and shortened and the pelvic diaphragm is in the ‘closed’, shortened position and hyperactivity more likely. The coccyx becomes hyperstabilized creating an inferior ‘tether’ of the syndesmosis part of the SIJ which restricts nutation of the sacrum and the lumbar spine moving into lordosis. When abdominal activity is increased, particularly the external oblique,95,103,104 the associated PFM hyperactivity may be in response to the increased intra-abdominal pressure so created. Retraining diaphragmatic breathing is indicated as a first step.33 The current fad of inappropriate overtraining the abdominals as ‘core muscles’ is compounding a lot of spinopelvic girdle dysfunction syndromes and probably contributing to SUI incidence. Furthermore, there is a subgroup of patients with SUI who have diligently performed ‘PFM exercises’ only to experience increasing leakage. Freeing the sacrum-coccyx and mastering the 1st fundamental pelvic pattern which opens the floor, coupled with complementary postural advice can lead to dramatic improvement in one treatment.
Importantly, Rock105 draws attention to ‘reflex incontinence’ whereby changes in PFM tone occur from reflex changes which occur in response to disorders of neuromyo-articular function elsewhere in the body e.g. functional disorders of the diaphragm can result in a reduction in both the elasticity and strength of the PFM due to diminished eccentric and concentric contractility respectively.
Pelvic floor and breathing
The close functional synergy between the diaphragm and PFM is disturbed when diaphragmatic breathing is compromised and can be further reflected in altered tone in the pelvic floor.105,106 Chaitow102 draws attention to the effects of PFM trigger points which in the main serve to increase PFM tone. Rock105 describes a study where external palpation of the PFM in continent male and female physiotherapists found all cases were hypertonic with painful trigger points and clear cut differences in tone between the two sides. Local PFM pain from trigger points cleared after 2–5 inspirations which focused upon ‘pushing the palpating finger away’. Improving diaphragm activity can thus change the tonus of the PFM. Clinical correlations between pelvic myo-articular dysfunction, PFM dysfunction and thoracolumbar dysfunction are common and treating either can affect the other.106 The complex innervation to the pelvic organs and pelvic floor includes somatic nerve fibres from S234, sympathetic nerves which originate T10 – L2, and parasympathetic supply originating in spinal segments S2-S4.107 Trigger points, altered muscle tone, SUI and various pain syndromes are often associated with disturbed related spinal segmental function and associated irritation of the spinal nerve roots supplying that particular pelvic muscle or tissue. The clinical findings of symptomatic segmental dysfunction can extend higher than the thoracolumbar junction and certainly appears to implicate autonomic contributions to PFM dysfunction and symptoms.
Pelvic floor and posturomotor control
Because the PFM forms part of the ligamentous/ myofascial syndesmosis119 contributing to the mechanics of the sacroiliac joint, their altered length/tension relationships and coordination will affect intrapelvic alignment and control and moderation of the dimensions the inferior pelvic bowl. Electrical stimulation of one side of the PFM demonstrated altered pelvic alignment with significant displacement of the coccyx, femur and innominate on the stimulated side.108 During the ASLR test, PFM hypoactivity has been demonstrated77 while others have reported increased activity.103 Unfortunately many sufferers have been taught to activate the PFM by ‘pull up and in’ in isolation without incorporation into appropriate synergistic and functional patterns of posturomovement control. This risks further imprinting the tendency for axial ‘holding patterns’, further disturbing motor control in the torso.
Movement control becomes coarser resembling more primitive and total flexion/extension movement patterns
In Chapter 7 we noted features of more primitive movement behavior, which can be variably apparent in subjects with spinal pain disorders and this is further explored. Instead of an infinite variety of adaptable postural sets, and movements, the patient often demonstrates a reduced repertoire, tending to adopt more primitive and stereotyped posturomovement strategies reminiscent of aspects of earlier developmental stages and possibly reflecting less than ideal integration; the early postural reflexes. The person tends to posture and move from say a pattern of more dominant flexion and will have some difficulty achieving pattern break up into combinations of flexion and extension such as hip flexion with spinal extension. This is associated with imbalanced muscle co-activation in the proximal limb girdles with poor regional or general axial control and patchy SGMS dominance. For example:
Flexor pattern influence