Chapter 58 Coma and Depressed Sensorium
Pathophysiology
The brain tolerates only limited physical or metabolic injury. Coma implies advanced brain failure, and the longer the brain failure lasts, the greater the possibility that the injury will result in permanent neurologic impairment. Coma may be described simplistically as a lack of consciousness. Posner and colleagues1 describe coma as a “state of unresponsiveness in which the patient lies with eyes closed and cannot be aroused to respond appropriately to stimuli even with vigorous stimulation.” Comatose patients may grimace in response to pain and the extremities may move in stereotypical withdrawal patterns, but the patient cannot localize responses or make defensive movements. As a coma deepens, responsiveness even to painful stimuli may be lost. Because motor reflexes are preserved, the depth of a coma cannot be assessed based only on motor responses. In many comatose patients, reflex movements will develop in response to stimuli. The depth of coma is best assessed by the patient’s level of consciousness.
Consciousness is a set of neural processes that allows an individual to perceive, comprehend, and act on and in the internal and external environment.1,2 Two neurophysiologic functions, arousal and awareness, which have discreet neuroanatomic locations, are integrated in the conscious person.3 Arousal or wakefulness describes the degree to which an individual appears to be able to interact within the environment. Awareness reflects the depth and content of the arousal state. When one is aware, one is alert (or aroused) and cognizant of self and surroundings. The relationship between wakefulness and awareness is hierarchical: Awareness cannot occur without wakefulness, but wakefulness may be observed in the absence of awareness (e.g., sleep/wake cycles in a vegetative patient).
Sleeping and waking are common examples of different states of arousal. Although coma and sleep both abolish conscious interaction with the environment, they differ physiologically because sleep is an active physiologic process with several distinct stages, and mechanisms for arousal remain intact. Sleep is dominated by a cortically generated slow wave (electroencephalogram [EEG]) activity within networks of neurons and glia, modulated by extracellular ion currents. Wakefulness is produced through the activation of brainstem and basal forebrain structures that disrupt sleep oscillations and elicit a global change in extracellular ion flow that results in modifications of glial and cerebral blood flow. Coma, however, occurs as a result of an impairment of physiologic components responsible for arousal and an inability to consciously interact.4–6
Anatomy of Arousal and Ascending Reticular Activating System
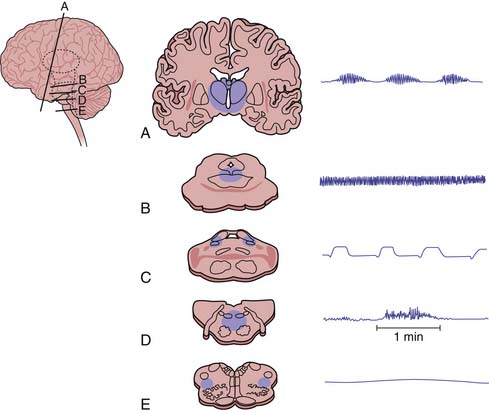
Arousal occurs by physiologic mechanisms that can be selectively impaired by toxins, anesthetics, or physical destruction of the brain stem. Neuroanatomically, the ascending reticular activating system (ARAS) and related structures responsible for arousal are primarily located in the brainstem in the paramedian tegmental grey matter immediately ventral to the pons. Three ARAS principle pathways have been identified (Figure 58-1). Communications have been identified between the ARAS and the cortex and the limbic system via the thalamic reticular nucleus, the cortex hypothalamus, the basal forebrain, and the brainstem median raphe (locus caeruleus).4 Because the ARAS receives collaterals from and is stimulated by every major somatic and sensory pathway directly or indirectly, it is best regarded as a physiological rather than an anatomic entity. This partly explains why patients with very large discreet lesions (brain tumors) may be entirely alert, whereas patients with anatomically undetectable but biochemically widespread lesions (e.g., hepatic encephalopathy) may be deeply comatose.
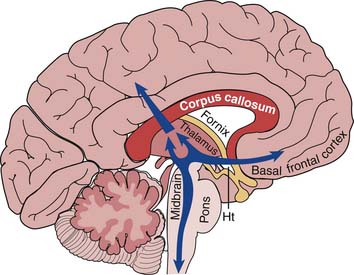
Figure 58–1 Reticular activating system.
(Modified from Hudson AJ: Consciousness: physiological dependence on rapid memory access, Frontiers Biosci 14:2779-2800, 2009.)
Primarily, two types of lesions depress the level of arousal: direct brainstem-diencephalic injury involving the reticular formation and nuclei, or bilateral cerebral dysfunction. Consequently, conscious behavior depends on the interplay between the cerebral cortex and ARAS because these neural components are required for arousal and to maintain awareness.1,4 Because the brain maintains a rich network of connections between the cortex, the ARAS, and the brainstem, patients with large discreet lesions might be alert on presentation, although localized neurological deficits are noted on physical examination. On the other hand, patients with only minimal exposure to CNS depressants present with a depressed sensorium. Changes in a patient’s level of consciousness imply significant dysfunction and can occur with variable degrees of wakefulness.
States of Impaired Sensorium
Precise definitions and descriptions of the various levels of consciousness are helpful in establishing a baseline, communicating with other health care providers, and interpreting changes in a patient’s condition. Box 58-1 describes definitions for varying levels of consciousness; however, many terms used to describe alterations in sensorium lack precision and are better avoided. Colloquial use of the terms lethargy, obtundation, somnolence, and stupor have rendered them imprecise, and health care workers are best served to avoid them when describing patients with altered consciousness. Numerous scoring systems have been developed to assess acute neurologic conditions. By far the most common is the Glasgow Coma Scale (GCS). Developed to classify the depth of coma in adults who have sustained a head injury, the use of the GCS has been expanded to evaluate patients who have sustained a variety of neurologic injuries. A GCS score of eight or less has been used as an alternative definition of coma. Although other scales are used to assess the severity of illness in coma (e.g., Liege coma scale, Apache II scale, and Reye syndrome), the GCS has gained wider acceptance because of its ease and familiarity.7 A modified GCS has been devised that is more applicable to infants.
Several states of depressed consciousness are described and deserve mention. Consciousness disorders should be distinguished from brain death, an irreversible loss of all brain and brainstem function.8–10 Coma is a state characterized by the absence of arousal and awareness. To differentiate coma from more transient causes of depressed sensorium (e.g., syncope and concussion), coma must last more than 1 hour. Comatose patients do not speak, open their eyes spontaneously, follow commands, move spontaneously, or respond meaningfully to painful stimuli. Spinally mediated stereotypical movements may be made in response to pain, but patients do not actively withdraw. Sleep-wake cycles are not preserved in patients who are in a coma. Patients in a coma are in a transitional state and can either deteriorate to a more permanent state of depressed sensorium, deteriorate to fulfill brain death criteria, or recover.
In a vegetative state, arousal mechanisms are preserved but patients completely lack an awareness of self or the environment.8, 9 Patients in a vegetative state demonstrate spontaneous eye opening without the ability to visually track or fixate. Although they may display “sleep-wake cycles,” they cannot follow commands or move in a purposeful manner. Patients in a minimally conscious state do not meet the criteria for coma or the vegetative state. They demonstrate wakefulness and sleep-wake cycles and intermittently demonstrate self or environmental awareness. These patients may intermittently follow commands, communicate, and display purposeful behavior. Although data are limited, the minimally conscious state may be associated with a greater possibility of recovery than the vegetative state. Lesions associated with this state involve the cerebral hemispheres, with possibly greater sparing of corticocortical and corticothalamic connective fibers.
Akinetic mutism is a state of wakefulness with limited evidence of awareness. Patients with akinetic mutism frequently have more diencephalic injury than injury to the motor tracts. Akinetic mutism8–10 has been associated with bilateral medial frontal lobe injury. The medial frontal lobe injury leads to a profound deficiency in motivation and an inability to plan and initiate activity. Akinetic patients generally are unable to move or speak and have sleep-wake cycles indicated by eye opening. Unlike patients in a minimally conscious state, akinetic patients have no motor responsiveness to verbal, tactile, or noxious stimuli. Further, spasticity or abnormal reflexes do not develop in these patients as a result of relative sparing of the corticospinal tract.
The locked-in syndrome is not a disorder of consciousness as much as it is an entity frequently confused with states of depressed sensorium due to the limited ability of these patients to communicate.8,9 Locked-in patients are quadriplegic and anarthric, but awareness and arousal are preserved. The locked-in syndrome is associated with injury to the ventral pons below the level of the third nerve nuclei and sparing of the ascending reticular activating system. Vertical eye movements and blinking usually are spared. More rostral injury may result in a total locked-in syndrome with loss of eye and eyelid movement that eliminates the ability of the patient to interact or communicate.
Identification of Cause
Coma may present as part of the progression of a known neurologic illness or the unpredictable consequence or complication of a known systemic disease, or it may result from a totally unexpected event or illness.10 An accurate history of the events and circumstances before the onset of the symptoms and information concerning the patient’s medical history and use of medications may be invaluable in determining the cause of coma and quickly lead to the most appropriate diagnostic testing and treatment. As in most pediatric disease, the differential diagnosis of coma is age related as described in Table 58.1. Common etiologies of coma seen in the pediatric population are described in Box 58-2.
Table 58–1 Common Considerations of Altered Mental Status at Various Ages
| Infant | Child | Adolescent |
|---|---|---|
Initial Assessment and Immediate Resuscitation
Once the patient’s airway, breathing, and hemodynamics are stabilized, a complete general examination and specific neurologic examination should be noted, along with any signs of trauma. Cervical immobilization should be maintained until trauma has been excluded or cervical spine has been cleared by radiographic and physical examinations. The patient should be completely exposed to allow a visual appraisal of swelling, lacerations, bruises, and other obvious signs of trauma. Blood or clear fluid noted in the nose or ears suggests a basilar skull fracture. Injuries with characteristic patterns (e.g., cigarette burns and glove and stocking burns), characteristic shapes, and characteristic locations (e.g., finger marks on the buttocks and bruises over ear lobes) suggest child abuse (see also Chapter 113).
Focused Neurologic Examination
A focused neurologic examination is key to documenting a baseline neurologic status and helps to locate lesions and determine prognosis in patients with diminished level of conscious (LOC).11 Because a diminished LOC requires either reticular system or bilateral hemispheric dysfunction, testing the structures immediately adjacent to the reticular system provides clues to the etiology of coma and directs subsequent investigations.2 A thorough physical examination must be systematic and is as valuable as radiographic and laboratory studies. The neurologic examination of a comatose patient differs from that of an awake, communicative subject and involves pupillary response, respiratory pattern, stimuli required to illicit a motor response, and the general character of the responses. History and presenting symptoms should be evaluated in the context of neurologic findings. Taken together, the history and presenting symptoms help determine the cause of diminished LOC. The level of neurologic dysfunction often is best defined by the respiratory pattern (Table 58-2), associated eye findings, and motor examination (Table 58-3).
Table 58–2 Respiratory Patterns in Patients with Altered Mental Consciousness
| Pattern | Description | Localization |
|---|---|---|
| Posthyperventilation apnea | Apnea for >10 seconds after 5 deep breaths | Bilateral hemispheric dysfunction |
| Cheyne-Stokes respiration | Rhythmic waxing and waning of respiratory amplitude | Bilateral hemispheric dysfunction |
| Central reflex hyperpnea | Continuous deep breathing | Bilateral hemispheric (e.g., trauma), lower midbrain, upper pons |
| Apneustic respiration | Prolonged aspiratory time (“inspiratory cramp”) | Pons |
| Ataxic respiration | Infrequent irregular breaths | Lower pons or upper medulla |
| Ondine’s curse | Failure of involuntary respiration with retained voluntary respiration | Medulla |
| Apnea | No respiration | Medulla down to C4: peripheral nerves, neuromuscular junction |
Table 58–3 Differentiating Characteristics of Structural and Metabolic Coma
| Supratentorial Lesions | Infratentorial Lesions | Toxic, Metabolic, or Infectious Processes |
|---|---|---|
Respiratory Pattern
Breathing abnormalities in rate, depth, or regularity are associated with altered LOC. These abnormalities could be signs of overdose, increased ICP, or herniation. Observance of the respiratory pattern also can assist in localizing a lesion. Anatomic correlations between areas of injury and the resultant respiratory patterns are found in Table 58.2 and Figure 58-2.
Eye Examination
Specific eye findings can help localize the level of lesions and establish prognosis. Pupillary changes are informative during the examination of coma because the brainstem areas that control consciousness are adjacent to those that control pupillary response. It is important to distinguish between pupillary dilatation caused by disease or injury and that caused by medication. Pupillary changes due to structural lesions depend on the site of the primary lesion and secondarily on the effects of increased ICP as described in Table 58.3 and presented in Figure 58-3. Because pupillary pathways are relatively resistant to metabolic insults, the presence or absence of a light reflex is the single most important physical finding that distinguishes structural from metabolic disease. Any reactivity is indicative of intact pathways and would rule out brain death.
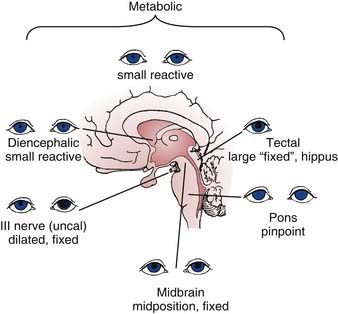
Figure 58–3 Pupils in comatose patients.
(Modified from Posner JB, Saper CB, Schiff ND, et al, editors: The diagnosis of stupor and coma, ed 4, New York, 2007, Oxford University Press.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree