CHAPTER 12 CIVILIAN HOSPITAL RESPONSE TO MASS CASUALTY EVENTS
On February 20, 1993, six people were killed and more than 1000 injured when a bomb exploded at the World Trade Center in New York City. Two years later, on April 19, 1995, 168 people died and 850 were injured when a bomb destroyed the Alfred P. Murrah Building in Oklahoma City. On September 11, 2001, 2986 people lost their lives when the Twin Towers of the World Trade Center collapsed after two hijacked civilian airliners were piloted into the towers by Islamic fundamentalists. These events served as a stimulus to the medical community to better prepare for mass casualty events caused by attacks with both conventional and unconventional weapons. The tsunami that destroyed coastal areas in Southern Asia on December 26, 2004 and the flooding of New Orleans after hurricane Katrina in September 2005 demonstrated inadequate responses to loss of infrastructure caused by natural disasters. A thoughtful and well-rehearsed disaster plan is essential to an effective response.
KEY DEFINITIONS
Patients are triaged into four categories at the scene: minor, delayed, immediate, and dead. In military triage systems, a fifth category, expectant care, is used for patients with a small chance of survival who would use scarce resources to such an extent as to adversely affect the chance of survival of other more salvageable patients. This category is rarely used in civilian situations as mobilization of additional personnel resources is usually possible. Numbers, colors, or symbols may be used to denote the categories (Table 1). “Undertriage” refers to assignment of patients to a level of care inadequate for their level of injury. An under-triage rate greater than 5% is unacceptable as it may lead to unnecessary morbidity and mortality in severely injured patients. “Overtriage” refers to assignment of patients to a level of care greater than required for their level of injury. An overtriage rate of 50% is considered acceptable to minimize undertriage. Excessive overtriage at the scene threatens the response of the entire system due to expenditure of limited resources on the wrong patients.
Table 1 The Four Colors of Triage
| Minor—Green | Delayed care/can delay up to 3 hours |
| Delayed—Yellow | Urgent care/can delay up to 1 hour |
| Immediate—Red | Immediate care/life-threatening |
| Dead—Black | Victim is dead/no care required |
Adapted from Los Angeles Community Emergency Response Team.
PREHOSPITAL CARE IN MASS CASUALTY EVENT
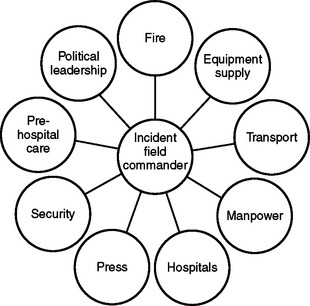
The response to a mass casualty event requires the coordinated effort of many agencies with disparate cultures, command structures, and even communications equipment (Figure 1). Appropriate agencies should submit to the authority of the incident field commander at the scene. Prior joint training can break down these barriers and improve overall response to the event.
HOSPITAL TRIAGE
If either a large number of casualties suddenly arrive without warning, or the hospital is informed of their impending arrival, the hospital should initiate its mass casualty plan. In a true mass casualty event, all area hospitals must participate in the care of victims to avoid exhaustion of the resources of any one facility. The common goal is salvaging as many lives as possible. A contingency plan for patients not involved in the mass casualty event must be in place as part of emergency preparedness. This plan permits the hospital to convert to mass casualty mode in a short period of time.
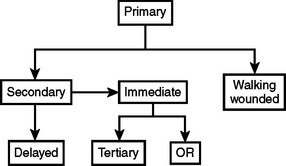
The initial hospital triage (Figure 2) should occur outside the ED as patients arrive by ambulance. Ideally, ambulances should pass through a security checkpoint prior to entrance to the hospital grounds to identify terrorists or ordinance that may be on board. Initial triage need not be done by a surgeon, but should be done by a highly experienced clinician. If possible, the walking wounded should be escorted through a separate entrance.
As soon as stretcher patients enter the ED, a senior surgeon should triage each patient to either immediate or delayed care (see Figure 2). The immediate treatment area should be reserved for salvageable patients with life-threatening problems. This area should have enough space for equipment and provide a one-way flow of traffic. The following personnel should be present at each bed in the immediate care area: a senior surgeon for decision making, an anesthesiologist to provide airway control, two ED or critical care nurses, and a junior surgeon for vascular access and tube thoracostomy as necessary.
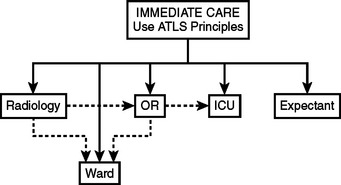
Treatment in the immediate care area is based upon the principles of advanced trauma life support. The goals of therapy in the immediate care area are airway control, ventilation, cessation of external hemorrhage, vascular access, and rapid transfer of the patient to the next appropriate treatment station, usually the intensive care unit (ICU) or the operating room (OR), for completion of the primary and secondary surveys and further diagnostic or therapeutic interventions. Factors affecting the decision as to where to perform the secondary survey and the patient’s ultimate disposition include the patient’s condition and the number of immediate care patients (Figure 3). This decision should be made by a senior surgeon.
HOSPITAL EMERGENCY INCIDENT COMMAND SYSTEM
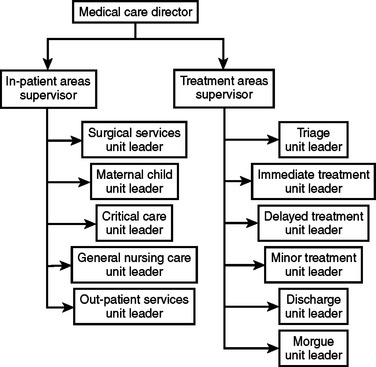
The basic principle of HEICS is that one individual supervises no more than five people and reports to only one person. A senior surgeon is the ideal incident commander. This system allows for efficient and manageable lines of communication and easy accountability. There are four main section chiefs: planning, logistics, finance, and operations. The operations chief has overall responsibility for the triage of victims and their clinical care, and potential coordination with other area hospitals (Figure 4).
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree