17 Child with a Fever
• A fever is defined as a temperature of 38.0° C (100.4° F) or higher measured rectally.
• Response to antipyretics is not a predictor of the presence of bacterial illness and therefore should not influence clinical decision making.
• The diagnostic evaluation of a febrile child is based on clinical findings, immunization status, and age of the child.
• The peripheral white blood cell count is unreliable in determining the presence or absence of bacterial illness and should not guide diagnostic and treatment decisions.
Perspective
Fever is the most common chief complaint in children younger than 3 years seen in the emergency department (ED) (see Facts and Formulas box). Fever is defined as an elevation in temperature to 38.0° C (100.4° F) or higher. In young children, particularly those younger than 2 years, the temperature should be taken rectally because other methods such as tympanic and axillary are not as reliable or accurate.1 Parental report of fever determined by touch is likely to be accurate regarding the presence of a fever.2 A common misconception is that bundling a baby can account for an elevation in core temperature, but it cannot.3 More than 20% of fevers seen in the ED will be fevers without a source and require risk stratification based on the child’s age, appearance, and immunization status.
Infants are at particularly high risk for serious bacterial illnesses because of their minimal signs and symptoms, lack of immunity, maternal birth canal exposure, and difficulty in mounting a response to infections. To deal with this increased risk for infection, multiple protocols to evaluate a febrile infant have been developed (Box 17.1). As a general consensus, infants younger than 28 days with a temperature of 38.0° C should undergo a full sepsis evaluation, parenteral administration of antibiotics, and admission to the hospital.4 A full sepsis evaluation includes a complete blood count (CBC) with differential, blood culture, and a catheterized urine sample sent for urinalysis, Gram stain, and culture. If symptoms are present, stool studies or a chest radiograph should be performed. A lumbar puncture with cell count and differential, Gram stain, and culture should be obtained. Antibiotics recommended are ampicillin, 50 mg/kg, and cefotaxime, 50 mg/kg. Ceftriaxone is not used in the neonatal period because of possible disconjugation of bilirubin. Neonatal herpes should also be considered as a cause of the fever, particularly in infants younger than 2 weeks. Frequently, the mother’s history of maternal herpes is not known, nor does the child have any physical findings. If there is any concern, herpes polymerase chain reaction should be performed on cerebrospinal fluid and the child should be administered acyclovir (20 mg/kg). Overall, well-appearing febrile neonates have a 7% likelihood of having a serious bacterial infection, with the most common being a urinary tract infection.5–7
Box 17.1 Criteria Historically Used for Risk Stratification in Pediatric Fever
Rochester Criteria
Previously healthy term infants without perinatal complications, younger than 3 months, and no soft tissue, ear, or skeletal infections
No previous use of antimicrobials
Lack of a focus of infection on examination
Peripheral white blood cell (WBC) count: 5000-15,000/µL
Stool WBC count: up to 5 WBCs per high-power field in infants with diarrhea
Philadelphia Criteria
Observation Score
Quality of cry (strong, whimpering, weak, high pitched)
Reaction to parent stimulation (cries briefly then stops, intermittent cry, continual cry)
State variation (awake, awake with stimulation, unarousable)
Color (pink, acrocyanotic, cyanotic)
Hydration (mucosal membranes: moist, slightly dry, dry)
Infants 28 days to 2 to 3 months of age may be risk-stratified with the febrile infant protocol to help guide the evaluation of fever (Figs. 17.1 and 17.2). Many physicians use an age cutoff of 60 days or less to perform a full sepsis evaluation, although some physicians still perform a full sepsis evaluation in children up to 90 days of age.8 These practice variations are seen in different settings: ED-based evaluation versus office-based evaluation and academic settings versus those in private practice.9 If a young infant meets the low-risk criteria outlined in Box 17.1, the physician may send the infant home with no antibiotics and follow-up the next day (note that the Boston criteria do recommend antibiotic administration). If the physician has any reservation about the ability of the caregivers to follow-up or any social concerns, one should err on the side of caution and admit the child to the hospital. If the infant does not fall into the low-risk criteria outlined, parenteral antibiotics should be administered and the child admitted to the hospital. Parenteral antibiotics should be given only if a lumbar puncture has been performed. Antibiotics used in this age group are ceftriaxone, 50 mg/kg intravenously or intramuscularly, or cefotaxime, 50 mg/kg intravenously.
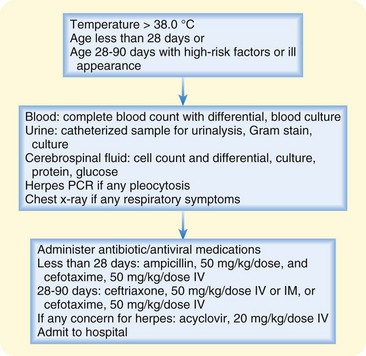
Fig. 17.1 Approach to febrile infants 0 to 28 days of age or ill-appearing children 29 to 90 days of age.
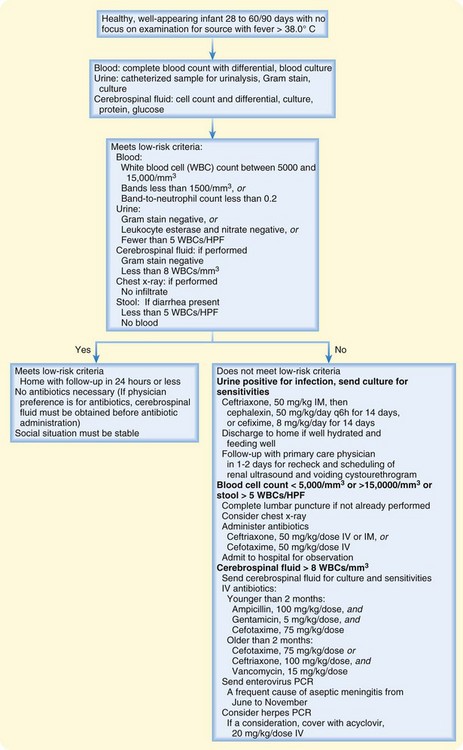
Fig. 17.2 Approach to children 28 to 90 days old with fever and no source on initial evaluation.
HPF, High-power field; PCR, polymerase chain reaction.
(Adapted from Baraff LJ. Management of fever without source in infants and children. Ann Emerg Med 2000;36:605; and Hoberman A, Wald ER, Hickey RW, et al. Oral versus initial intravenous therapy for urinary tract infections in young febrile children. Pediatrics 1999;104:79-86.)
The approach to fever evaluation in a 2- to 3-month-old to 3-year-old has changed dramatically over the past 10 years because of vaccine development and an increasing rate of vaccination.10 An algorithm using an updated approach based on risk stratification is outlined in Figure 17.3. Before availability of the conjugated pneumococcal vaccine, a well-appearing child with a temperature of 39° C and no focus of infection would have blood drawn for a CBC and blood culture. The patient would have been administered a parenteral antibiotic if the white blood cell count was greater than 15,000/mm3.11 The concern was for occult bacteremia (OB) and possible progression of OB to meningitis. In 1987, the Haemophilus influenzae type B (Hib) vaccine was introduced and dramatically reduced the prevalence of OB secondary to Hib to the point of no longer being clinically pertinent.12 The heptavalent pneumococcal conjugated vaccine (PCV-7) was introduced in the United States in 2000 and has recently been expanded to thirteen valent (PCV-13). PCV-13 is aimed at the most invasive strains of S. pneumoniae and is administered at 2, 4, 6, and 12 to 15 months. After one dose, the vaccine has 90% efficacy against vaccine serotypes. Although the recommended vaccination schedule for the pneumococcal vaccine includes four immunizations, it has been reported that two vaccinations induce satisfactory antibody responses and may therefore be protective.13 It is thought that herd immunity may provide protection for older adults and unimmunized children.14–16
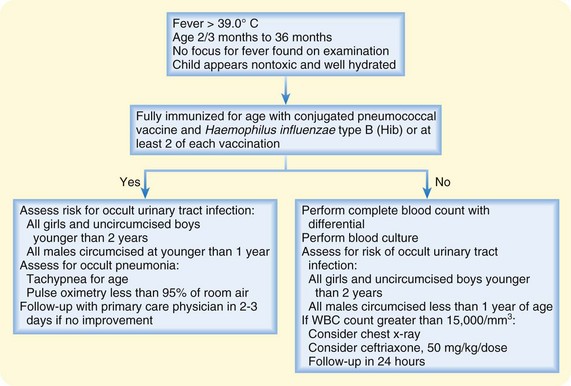
Fig. 17.3 Approach to children 3 to 36 months of age with fever and no obvious source.
(Adapted from Baraff LJ. Management of fever without source in infants and children. Ann Emerg Med 2000;36:605.)
Lee et al. determined that at rates of pneumococcal bacteremia greater than 1.5%, obtaining a CBC, performing blood cultures, and administering antibiotics empirically was cost-effective.17 Conversely, if the rate of pneumococcal bacteremia was less than 0.5%, strategies using empiric testing and antibiotics would no longer be cost-effective. Since the work of Lee et al. several investigations have determined the overall frequency of pneumococcal bacteremia to be well below 1%.14,18,19 The rate of bacteremia may be low enough to support the evolving practice of not drawing blood for routine CBC and blood cultures in previously healthy febrile children between 2 and 36 months of age who have received at least one PCV-7 vaccination.20 Evidence is mounting that the bacteremia rate and particularly the pneumococcal bacteremia rate have declined to the extent that empiric testing and treatment may no longer be necessary.
![]() Facts and Formulas
Facts and Formulas
Fever: for ages 0 to 2 months, a temperature of 38.0° C or higher measured rectally; for ages 2 to 36 months, a temperature of 39° C or higher measured rectally
Fever without a source: acute febrile illness without localizing signs or symptoms despite a careful history and physical examination
Bacteremia: presence of bacteria in the bloodstream
Occult bacteremia: presence of bacteria in the bloodstream of a febrile child who may not appear particularly sick and has no apparent other source of infection
Serious bacterial illness: accounts for 2% to 4% of fevers. Examples include pneumonia, cellulitis, septic arthritis, osteomyelitis, urinary tract infection, meningitis, and sepsis21,22
Pathophysiology
Fever is the host’s adaptive response to an invading microorganism. The microorganism comes in contact with cells of the immune system, including macrophages and leukocytes, and such contact leads to the release of various cytokines, most notably interleukin-1, tumor necrosis factor, and interleukin-6. These cytokines circulate and come in contact with neuronal cell groups around the edges of the brain’s ventricular system. Prostaglandin E2 is then released and binds to receptors on neurons in the hypothalamus and brainstem, which leads to upregulation of the hypothalamic thermostatic set-point.23,24 Once the thermoregulatory center is reset, a higher body temperature is maintained through various mechanisms such as cutaneous vasoconstriction and shivering. The febrile response is not fully developed in young infants, and fever or even hypothermia may occur in response to infection. The physiologic limit of thermoregulation is estimated to be 41.1° C (106° F). According to McCarthy, children with a fever of this degree have a high rate of central nervous system insult.1
Presenting Signs and Symptoms
When evaluating a febrile child, the clinician must obtain key information from the history and physical examination (Box 17.2 and see the Documentation box). According to McCarthy et al., the sensitivity of clinical evaluation in an infant younger than 3 months and between 3 and 36 months of age is 78% and 89% to 92%, respectively.1,25 After the history and physical examination, the source of fever remains inapparent in 20% of febrile children.26,27







