Figure 19.1. Anatomy of deep cervical plexus block. The transverse processes lie under the lateral border of the sternocleidomastoid muscle, each with a distal trough or sulcus that defines the path of nerve exit.
III. Drugs
For surgery, any of the intermediate- or long-acting aminoamides are appropriate. Lower concentrations are sufficient for the superficial (sensory) block, but higher concentrations such as 1.5% lidocaine or 0.5% bupivacaine (or ropivacaine) will give better motor anesthesia with deep plexus block. All of the drugs will demonstrate a slightly shortened duration in the neck compared to other peripheral areas because of the generous blood supply of the region.
IV. Techniques
For both deep and superficial blocks, the patient is placed supine with a small towel under the occiput and the head turned to the side opposite the one to be blocked.
A. Deep cervical plexus anesthesia
1. The mastoid process is identified and marked, as is the transverse process of the sixth cervical vertebra. This is the most prominent tubercle in the neck, and it lies at the level of the cricoid cartilage.
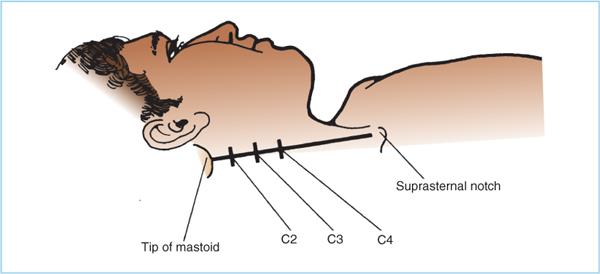
2. A line is drawn between these two points, indicating the plane of the transverse processes of the cervical vertebrae (Figure 19.2). The lateral border of the SCM muscle is also marked.
3. Starting 1.5 cm below the mastoid, gentle palpation is used to identify the tubercle of the second vertebra just posterior (approximately 0.5 cm) to the first line. An “X” is placed over this process.
Figure 19.2. Superficial landmarks for cervical plexus block. A line is drawn from the mastoid process to the prominent tubercle of the sixth cervical vertebra. The transverse processes of the second, third, and fourth cervical vertebrae lie 0.5 cm posterior to this line, and at 1.5-cm intervals below the mastoid.
4. The third and fourth processes are identified and marked in the same manner by moving 1.5 cm caudad for each level. The third mark should fall approximately at the level of the junction of the external jugular vein and the SCM muscle.
5. After aseptic preparation, a skin wheal is raised at each of the three “X” marks.
6. A 3.5-cm (1.5-in.) 22-gauge needle is introduced perpendicular to the skin and is directed posterior and slightly caudad at each “X” until it rests on the transverse process. A palpating finger of the opposite hand helps in guiding the placement.
7. Placement on the transverse process is confirmed by “walking” the needle caudad and cephalad; it should slip off the bone of the process rather than continuing to contact bone, as it would if on the vertebral body (Figure 19.1). The latter situation is undesirable because the needle is not near the nerve, but is more likely to produce intravascular or subarachnoid injection.
8. A syringe is attached to each needle in turn while it is securely held in place just above the transverse process. Then 3 to 5 mL of anesthetic solution is injected in small increments with frequent aspiration and assessment of the patient’s mental status.
9. Onset of anesthesia should occur within 5 minutes.
10. An alternative is to use a variation of the interscalene technique with a peripheral nerve stimulator. A single stimulating needle is introduced into the groove between the muscles at the C4-5 level (at the upper border of the thyroid cartilage). Stimulation of the levator scapulae muscle produces elevation and internal rotation of the scapula, and injection of a single bolus of 40 mL of anesthetic produces plexus blockade. Local anesthetic can be shown to spread in a hemicylindrical column from approximately the C1 to the C7 level (3,4).
B. Superficial cervical plexus anesthesia is performed with the patient in the same position as for deep plexus anesthesia.
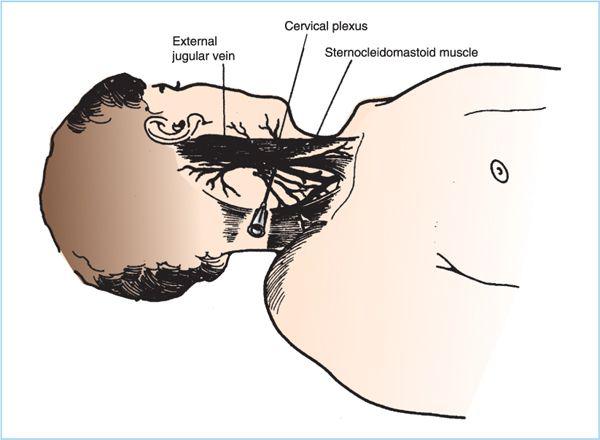
Figure 19.3. Superficial cervical plexus block. The sensory fibers of the plexus all emerge from behind the lateral border of the sternocleidomastoid muscle. A needle inserted at its midpoint, usually where the external jugular vein crosses the muscle, can be directed superiorly and inferiorly to block all of these terminal branches.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree