CHAPTER 52 Cardiocerebral Resuscitation, Defibrillation, and Cardioversion
SUDDEN DEATH is a leading cause of mortality in developed countries and accordingly an important public health problem.1,2 Although out-of-hospital cardiac arrest is the major cause of sudden death, in-hospital cardiac arrest is also a significant concern. Fortunately, the incidence of ventricular fibrillation (VF) occurring in hospitalized patients with and after an acute coronary syndrome is decreasing because of more aggressive revascularization that decreases ischemia and limits infarct size, the use of β-adrenergic blockers that reduce ischemia, and the correction of hypomagnesemia and hypokalemia—electrolyte abnormalities that predispose to ventricular arrhythmias.2 Despite this trend, ventricular fibrillation is still one of the many medical emergencies that the physician must be able to manage.
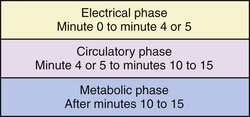
The approach to the therapy of ventricular fibrillation both in and out of hospital depends upon its duration. Therefore this chapter begins by reviewing this important and relatively new concept, delineating the electrical, circulatory, and metabolic phases of untreated ventricular fibrillation.3
A major portion of this chapter will deal with cardiocerebral resuscitation (CCR), a more effective approach to the therapy of unexpected or primary cardiac arrest that is so new that many of its tenets have yet to be incorporated into national and international guidelines.4–8 A review of national and international guidelines for cardiopulmonary resuscitation (CPR) and advanced cardiac life support (ACLS) for primary cardiac arrest is not appropriate because significant portions of even the 2005 guidelines are currently out of date.9 Traditional CPR should be reserved for respiratory arrest—a review of which is beyond the scope of this chapter.
Etiology of Ventricular Arrhythmias
The most common causes of ventricular tachycardia and fibrillation are acute myocardial infarction, chronic ischemic heart disease with decreased ventricular function, valvular heart disease that results in significant myocardial dysfunction, and cardiomyopathies (dilated, hypertrophic, arrhythmogenic right ventricular dysplasia [ARVD], and neuromuscular disorders).2 Other causes include myocarditis, infiltrative cardiomyopathies, end-stage chronic kidney disease, and congenital heart disease in adults who had postoperative correction of their defect(s). Normal ventricular function does not rule out a cardiac cause of near syncope, frank syncope, or cardiac arrest because there are a number of arrhythmias that can produce such symptoms. Genetic identification is now possible for some conditions that predispose to serious cardiac arrhythmias, such as long QT syndrome, short QT syndrome, Brugada syndrome, and idiopathic ventricular tachycardia. Other conditions such as electrolyte disturbances and toxic agents that can cause ventricular tachycardia, VF, and sudden death must be identified clinically. Stress cardiomyopathy is a newly recognized entity of myocardial dysfunction that occurs predominantly in women following severe emotional stress that may result in ventricular dysfunction, hypotension, shock, and even ventricular fibrillation—an explanation for emotionally induced sudden death.
Three Phases of Ventricular Fibrillation
Some of the recent changes in the approach to the therapy of ventricular fibrillation (VF) are based on the three-phase, time-sensitive model of untreated VF articulated by Weisfeldt and Becker.3 This model helps to explain why some of the previous approaches to and recommendations for the therapy of VF are ineffective.
The first, or electrical phase (Fig. 52-1) of untreated VF, lasts for 4 or 5 minutes. During this time the most important therapeutic intervention is prompt defibrillation. Although the heart is fibrillating, the myocardium has neither used up all of its energy stores nor undergone serious cellular damage and is therefore able to respond to the electrical defibrillation and generate a perfusing rhythm. This is why implantable cardioverter-defibrillators (ICDs) are so effective and why automated external defibrillators (AEDs) have been employed successfully in patients with out-of-hospital cardiac arrest in airplanes and airports, casinos, and in communities where prompt defibrillation was possible.10–12 However, even in the electrical phase of VF, the earlier the defibrillation, the greater the chance that it will result in a perfusing rhythm and therefore survival.
The second or circulatory phase (see Fig. 52-1) of untreated VF lasts for a variable period of time, originally estimated to be from about minute 5 to about minute 10 of untreated VF (but probably extends from minute 5 to about minute 15). During this circulatory phase of ventricular fibrillation, the continued lack of myocardial perfusion during the continued uncoordinated myocyte contractions of untreated VF results in declining amplitude and frequency spectrum of the electrocardiographic fibrillation waveforms, declining myocardial energy stores, and the accumulation of toxic metabolites.13,14 Defibrillating during this circulatory phase without first improving myocardial perfusion by chest compressions usually results in pulseless electrical activity (PEA) or asystole. A critical intervention during this second or circulatory phase of VF cardiac arrest is restoring myocardial blood flow by the generation of adequate coronary perfusion pressure with chest compressions not only before but also immediately after direct current shocks.4 Chest compressions during the circulatory phase of VF increase the amplitude and the frequency spectrum of the fibrillation waveforms and improve the chances of restoring a perfusing rhythm following defibrillation. Chest compression immediately after the electrical shock provides perfusion to the energy-starved poorly contracting myocardium, increasing its chance of recovery and allowing it to develop enough strength or force of contraction to generate a perfusing rhythm. The third or metabolic phase (see Fig. 52-1) of VF follows the circulatory phase. Survival in this phase, in the absence of hypothermia, is unusual.
Defibrillation
Mechanical Defibrillation (Precordial Thump)
A blow to the chest with a clenched fist, referred to as a “precordial thump,” was first reported in the 1960s.15 Precordial thump delivered soon after the onset of VF was found to be capable of defibrillating ventricular fibrillation and converting ventricular tachycardia to normal sinus rhythm. A precordial thump is the easiest, though least effective form of defibrillation. A precordial thump defibrillates less than 2% of patients with VF and does so only in those with a very recent onset of ventricular fibrillation.15 The response of ventricular tachycardia to a precordial thump is more effective but is less predictable. A blow to the chest has been estimated to convert about one third of patients with ventricular tachycardia (VT) into sinus rhythm. In another third, a precordial thump has no effect, and in the final third VT is converted to VF. Because of this observation, monitored VT in a patient without cardiac arrest should not be treated with precordial thump unless a defibrillator is present.16 Nevertheless one might consider a precordial thump as the initial therapeutic approach in an unresponsive patient with witnessed collapse and abnormal breathing because of its rapidity and ease of delivery.
Electrical Defibrillation
During the first 4 to 5 minutes or the electrical phase of ventricular fibrillation, the most important intervention is prompt electrical defibrillation. There are rare instances of spontaneous reversion of ventricular fibrillation, but many of these are in fact instances of polymorphic ventricular tachycardia incorrectly assumed to be VF. The shorter the duration of VF before electrical defibrillation, the more likely it will result in successful resuscitation. Experience with modern implantable cardioverter-defibrillators (ICDs) is that if the electrical shock is applied within seconds, nearly 100% can be defibrillated.17 Kouwenhoven’s experimental studies of over a half century ago found that if the defibrillation shock was delivered within 30 seconds of the onset of ventricular fibrillation, 98% of the animals survived; if the shock was delayed just 2 minutes, only 27% lived. More recent reviews estimate that the chances of successful defibrillation decrease about 10% for each minute of untreated VF.
The technique, physics, and hemodynamics of defibrillation in cardiac arrest are addressed later in this chapter.
Ventricular Tachycardia or Fibrillation Storm
Frequently recurring episodes of ventricular tachycardia (VT) degenerating into VF requiring multiple defibrillations has been termed “VT storm.”2 In such patients, in addition to appropriate defibrillations, intravenous β-blockade and/or urgent cardiac catheterization should be considered, for if ischemia is the initiating factor and it is still present, every effort needs to be directed at decreasing the ischemic burden.2 Amiodarone, often in combination with β-blockers, can be useful for patients with left ventricular (LV) dysfunction because of prior myocardial infarction (MI) and recurrent VT.2 If the VT storm is from polymorphic VT, intravenous β-blockage is the single most effective therapy.2 All too often VT storm is secondary to the administration of multiple antiarrhythmic drugs.
Cardiocerebral Resuscitation for Cardiac Arrest
Why CCR for cardiac arrest? Although CPR has been in existence for almost a half century, in the absence of early defibrillation in patients with primary cardiac arrest, the survival rates are poor and have remained essentially unchanged for decades.4,5 It is now apparent that a major reason for the heretofore abysmal survival rates of patients with out-of-hospital cardiac arrest (OHCA) is that the previous guidelines were far from optimal and the current (2005) guidelines, while improved, leave much to be desired.
One reason for the poor survival is the lack of bystander-initiated CPR. This is in part due to the recommendation for mouth-to-mouth ventilation or so called “rescue breathing.”4 It is well known that this recommendation is a major reason individuals are not willing to perform bystander CPR on a stranger. And with the current universal precautions in hospitals, mouth-to-mouth ventilations are rarely performed in hospitals anymore. And for OHCA, if one calls 911 and does nothing until the paramedics arrive, the patient is not likely to survive. Or in large hospitals, if the cardiac arrest team is activated but bystander resuscitation efforts are not initiated until the team arrives, the chance of survival is greatly diminished. Any chain is only as strong as its weakest link, the weakest link in the chain of survival for cardiac arrest is the first link—bystander CPR. The solution to this problem is bystander continuous chest compressions or chest-compression-only CPR.
This approach is called “cardiocerebral resuscitation” or CCR.4,5 The major tenets of CCR are based on the fact that during resuscitation for cardiac arrest, the cardiac output or forward blood flow is so marginal that any interruption in continuous chest compressions is deleterious, and that during out-of-hospital cardiac arrest, the paramedics arrive not during the first or electrical phase of VF arrest but during the circulatory phase. And during this phase chest compression before and after defibrillation is necessary for optimal survival.4
Circulatory Phase of Untreated Ventricular Fibrillation
Although prompt defibrillation is often effective in the electrical phase of VF, direct current shocks, especially sequential or so-called stacked shocks are not only not effective, but are harmful during the circulatory phase of untreated VF because they interrupt or delay chest compressions during the critical circulatory phase of ventricular fibrillation.4,18 This concept led to an important change in the 2005 guidelines for ACLS.9 These guidelines no longer recommend stacked shocks but a single shock followed by the immediate application of 200 continuous chest compressions before rhythm and pulse analysis. These recommendations have been a part of CCR since 2003.4,19,20
Cardiocerebral Resuscitation—A New Approach for Cardiac Arrest
If a monitored patient develops ventricular fibrillation, the optimal approach is rapid defibrillation—a major advantage of the coronary and intensive care units. However, the majority of OHCAs and some in-hospital cardiac arrests occur in a location that takes the emergency response services (EMS) several minutes to arrive. In this situation, CCR, a new approach to patients with OHCA that dramatically improves survival, is recommended.4,5 Why a new approach to cardiac arrest? Despite standards published in 1974, standards and guidelines published in 1980, guidelines in 1992, and updates of guidelines in 2000,21–24 the survival rate of patients with OHCA has not improved, and in the absence of early defibrillation is so poor it is near that described as medical futility.25 Accordingly in 2003, our University of Arizona Sarver Heart Center Resuscitation Research Group, based on more than 3 decades of defibrillation and resuscitation research and our interpretation of the literature, could no longer in good conscience follow the guidelines, and developed the CCR approach.4,5,19,26 This approach has now been shown to dramatically improve survival over the previous approach for patients with OHCA.5,26
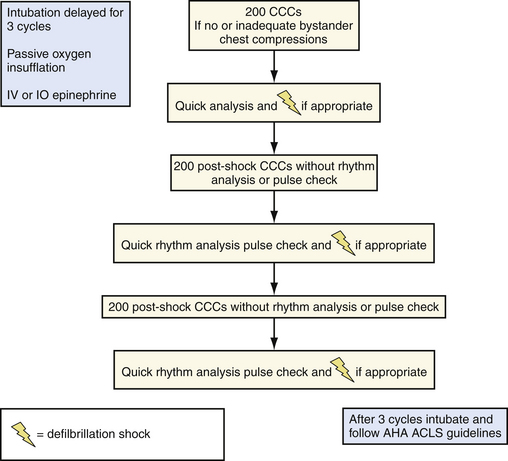
CCR has three components (Fig. 52-2). For bystanders, continuous chest compression (CCC-CPR) or chest-compression-only is recommended because it has been shown that patients with cardiac arrest are more likely to be in VF when the EMS arrives if a bystander initiates resuscitation efforts (or bystander CPR) and bystanders are more likely to initiate bystander resuscitation efforts if mouth-to-mouth or so called “rescue breathing” is not required.27 Chest compression only, as will be described later, also results in better survival because it does not result in excessive interruptions of the marginal forward blood flow existent during traditional resuscitation efforts for cardiac arrest.28,29
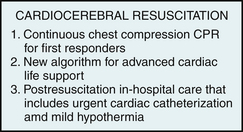
Figure 52-2 Three components of cardiocerebral resuscitation. The first component is continuous chest compressions (CCC) without assisted ventilation for bystanders and first responders (CCC-CPR). The second component is a new approach to advanced cardiac life support (the details of which are shown in Fig. 52-3). The third component includes an aggressive approach to cardiac catheterization and intervention when appropriate and therapeutic hypothermia for patients who are comatose after resuscitation. CPR, cardiopulmonary resuscitation.
The second and major component of CCR is a new approach to advanced cardiac life support (e.g., the approach of medical personnel who arrive with a defibrillator, but who did not witness the arrest, and thus arrive most often after the electrical phase of the patient’s cardiac arrest [Fig. 52-3]). If adequate continuous chest compressions are not being done by the bystander, CCR advocates an initial 200 continuous chest compressions with special attention to appropriate technique.4 The appropriate technique of chest compressions for cardiac arrest includes forceful chest compressions of adequate depth (1½ to 2 inches) at a rate of 100 compressions a minute, each followed by removal of the heel of the hand from the sternum to allow full chest wall recoil. This compression technique is essential during the circulatory phase of VF arrest, both before and after a single defibrillation shock.
CCR eliminates any intervention that delays or interrupts continuous chest compressions, or provides positive pressure ventilation. The reason for limiting interruptions of chest compressions is that during compressions for cardiac arrest, the forward blood flow is so marginal that any delay or interruption of chest compression significantly decreases cerebral blood flow and decreases the chance for neurologically intact survival.4 The use of automated external defibrillators (AEDs) while effective during the electrical phase of VF arrest is detrimental during the circulatory phase of cardiac arrest if they significantly delay and interrupt chest compressions.4 Thus after the shock is delivered by an AED, the verbal instructions of AED presently must be ignored. Two hundred postshock chest compressions are to be immediately instituted (see Fig. 52-3). The reason for this recommendation is that in our experimental laboratory model of OHCA, defibrillation during the circulatory phase of VF arrest usually results in very low pressure pulses that increase with assistance of continuous chest compressions.4,30
Another important component of CCR is the elimination of positive pressure ventilations (see Fig. 52-3). The reasons for the elimination of positive pressure ventilations are twofold: First, intubation results in a significant delay in chest compressions during the circulatory phase of VF arrest. Secondly, during chest compressions for cardiac arrest, the forward blood flow is so marginal that any increase in intrathoracic pressure decreases venous return and subsequent cerebral blood flow.4,6,29
The prevention of positive pressure ventilations and hyperventilation (very common during the excitement of a cardiac arrest) is accomplished by using passive oxygen insufflation5,31(see Fig. 52-3). Passive oxygen insufflation is applied by a second rescuer, and is accomplished by placing an oral pharyngeal airway and nonrebreather mask and high flow oxygen. Another advantage of this approach is that this frees the second rescuer to perform other critically important functions such as starting an intravenous line for epinephrine administration.5
Cardiocerebral Resuscitation Improves Survival of Patients with Out-of-Hospital Cardiac Arrest
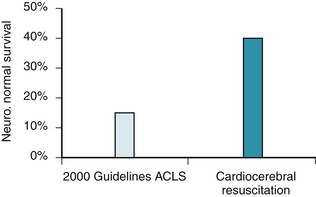
It has been shown that the application of CCR dramatically improved survival of patients with OHCA compared to that existent in the same (EMS) systems that used the Guidelines for Cardiopulmonary Resuscitation and Advanced Cardiac Life Support (ACLS) hereafter referred to as “Guidelines 2000.” The first report was from two rural counties in Wisconsin, where CCR was initiated in early 2004.5 In the 3 years (2002 to 2005) when the Guidelines 2000 approach was used, in this report, there were 93 witnessed out-of-hospital adult cardiac arrests with an initially shockable rhythm. Nineteen patients survived and 14 of 92 (15%) were neurologically normal at hospital discharge. During the first year that CCR was instituted, the neurologically normal survival was 16 of 33 (48%).5 This study clearly supported the new approach of cardiocerebral resuscitation but was not definitive because of the small number of patients treated by CCR and because of a potential Hawthorne effect—that is improved performance of individuals who knew they were being studied. Longer duration of study was needed to address these concerns. Longer follow-up has been completed. During the 3 years of CCR follow-up, from 2005-2007, there were 91 patients with witnessed cardiac arrest who had a shockable rhythm on arrival of the EMS personnel. Forty-four survived (48%) and 37 (40%) were neurologically normal at hospital discharge (P = 0.001). The institution of CCR tripled neurologically intact survival of patients with witnessed OHCA and a shockable rhythm on arrival of the emergency medical system. One could conclude that there was some Hawthorne effect in the initial report because the second report with longer follow-up found a 250% increase in survival rather than the initial report of a 300% increase in survival (Fig. 52-4).
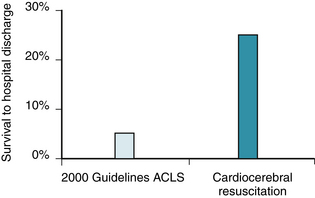
CCR was then instituted in two large municipal fire departments in the Phoenix metropolitan area in 2005. Survival to hospital discharge and other data were collected from these two large fire departments when Guidelines 2000 CPR and ACLS were used, and then following training of the emergency medical services (EMS) firefighters in CCR. Among the 713 cardiac arrests in these two fire departments, survival improved from 1.8% (n = 2/219) pretraining to 6.5% (n = 32/494) posttraining). In the subgroup with witnessed arrest and ventricular fibrillation on arrival of the EMS, survival to hospital discharge improved from 5% (n = 2/43) pretraining to 25% (n = 22/89) posttraining.26 The results of these initial observations on the application of CCR are shown in Figure 52-5. Application of CCR for witnessed OHCA worldwide would result in the saving of innumerable lives.
Guidelines 2005 did make some changes in recommendations for ACLS that have been shown to improve survival. The change from multiple or stacked defibrillator shocks to a single shock followed by 200 chest compressions before pulse check or rhythm analysis, part of the tenets of CCR that we instituted in 2003, has also resulted in improved survival of patients with out-of-hospital cardiac arrest.18
Proper Technique of Chest Compressions
As noted previously, during cardiac arrest and resuscitation efforts, the perfusion pressures and forward blood flow generated by chest compressions are marginal at best. Accordingly, any interruption of chest compressions has an adverse effect on cerebral and myocardial perfusion and dramatically decreases the chance of neurologically intact survival. The delivery of near continuous, appropriate chest compressions is therefore another fundamental tenet of CCR.4
The emphasis on limiting interruptions of chest compressions is based upon research that showed that the major determinant of neurologically intact survival from prolonged cardiac arrest because of VF is the perfusion pressures generated by chest compressions rather than the blood gas composition, acid-base balance, or the frequency or strength of defibrillation shocks.32–34 During resuscitation efforts, any interruptions of chest compressions immediately curtail blood flow to the heart and the brain and resumption of chest compressions may take several compressions to restore good perfusion pressures.32,35,36 CCR advocates near continuous chest compressions and limits assisted ventilations until after three rounds of chest compressions, shock when indicated, and chest compressions (see Fig. 52-3). There should be no interruptions of chest compressions for anything but post–chest compression defibrillation until the return of spontaneous circulation or the termination of the resuscitation effort. Pulse checks are to be done only during pauses in chest compression for rhythm analysis after the 200 postdefibrillation chest compressions.5
The third component of CCR is postresuscitation care. If the patient is unconscious postresuscitation, mild hypothermia (32° C to 34° C) has been shown to improve neurologically normal survival.37–39 Most patients should be taken to the cardiac catheterization laboratory because some will have acute coronary occlusion without ST-segment deviation on their electrocardiogram. Attention to glucose control and electrolyte balance is also an important part of postresuscitation care.
Bystander Responder Critical
Role of Continuous Chest Compressions or Chest-Compression-Only CPR
Several studies have found that survival of patients with OHCA who receive chest compression alone without mouth-to-mouth ventilations by bystanders are not statistically different from survival of such patients who receive chest compression plus so-called “rescue breathing.”40–42 Nevertheless, the technique of chest compressions without rescue breathing has not been recommended by the guidelines unless the bystander is unable or unwilling to perform mouth-to-mouth ventilation.9,24 The rational for this recommendation is that the guidelines’ authors evidently did not want lay individuals to have to decide if the patient has a cardiac arrest or a respiratory arrest. As will be noted later, this author thinks that this is not only possible but essential because many more individuals have OHCA and respiratory arrest. In Tucson, Ariz., it has been estimated that there are about 100 out-of-hospital cardiac arrests for every drowning death. In Seattle, the reported incidence of cardiac arrest to respiratory arrest is 20 to 1.42 In certain cultures, for example in those with a high incidence of drug abuse, the incidence is probably higher. In other cultures the incidence of respiratory to cardiac arrests is probably lower.
Studies by Kern and associates, in realistic swine models of OHCA, found that the provision of chest-compression-only CPR was more effective than the provision of standard 2:15 CPR, when each set of 15 chest compressions was interrupted for a realistic 16 seconds, to simulate the duration without chest compressions reported for a single rescuer to deliver the recommended “two quick breaths” and resume chest compressions.36 In 2007, similar findings were reported in humans.28 The survey of survivors (SOS) KANTO study reported that the overall survival of patients with OHCA was 2.2% for those who had not received bystander CPR when the EMS arrived, 4.2% for those who were receiving chest compressions plus mouth-to-mouth ventilation, and 6.2% for those receiving chest-compression-only by bystanders.28 More importantly, these investigators reported that in the subset of patients with the greatest chance of survival—those with witnessed arrest and a shockable ventricular arrhythmia upon arrival of the EMS personnel, the survival was nearly twice as great (11% versus 19%, P = 0.05) in those who had received bystander chest compression alone than in those who received chest compression plus mouth-to-mouth ventilation.28
Following the publication of this important study, the guidelines were not changed despite a call for urgent changes.43 The reason was that this observational study was done during a time when the recommended ventilation to chest compression ratio was still 2:15. The 2005 Guidelines of the American Heart Association (AHA), the European Resuscitation Council, and the International Liaison Committee for Resuscitation (ILCOR) changed their recommendations in the 2005 guidelines for ventilations to chest compression ratio to 2:30.9 The change in the 2005 guidelines from 2:15 to 2:30 was based in part on the findings of Abella and colleagues.44 In a prospective observational study of in-hospital cardiac arrest in three hospitals during 2000-2003, those patients who had a return of spontaneous circulation (ROSC) received a greater number of chest compressions per minute than those who did not. The average number of chest compressions per minute was 90 + 17 in those who had ROSC compared with 79 + 18 in those who did not have ROSC.44 In their analysis, it seemed that a compression rate of at least 89 compressions per minute was necessary for higher rates of ROSC. Of note is the fact that the survival of patients with in-hospital cardiac arrest in these three academic hospitals was so poor that it was not reported.44
Animal studies showed that ROSC was better with a 2:30 ventilation to compression ratio than with the previous standard of 2:15.45 Thus there was no long-term (24-hour) survival evidence that the change to the recommended 2:30 ventilation to compression ratio would improve survival. The recommendation was based on consensus.9 One could argue that observational studies in man were needed before guideline changes could be made. We argue that our swine models of OHCA, showing that continuous chest compressions were better than 2:15 when a realistic 16-second interruption was used to provide the two ventilations, predicted the results found in man.28,43
In subsequent studies using the same swine model of OHCA, Ewy and colleagues found that when simulated bystander resuscitation was initiated 4 to 6 minutes after the onset of VF arrest, and defibrillated after 12 minutes of VF, chest-compression-only CPR (CCC-CPR) resulted in a greater number of neurologically normal 24-hour survivors than did 2:30 ventilations to compressions.46 Neurologically normal survival was found in 16 of 24 (64%) of the swine who received continuous chest compression compared with 6 of 23 (26%) receiving two ventilations for every 30 chest compressions before defibrillation.46
Teaching Bystander “Chest-Compression-Only CPR”
The lay component of CCR emphasizes calling the emergency medical system (911 in the United States) followed by continuous chest compressions without mouth-to-mouth ventilation. This activity is only to be interrupted if an AED is available.4
We think it is important that bystanders be told that it is not necessary to remove any of the patient’s clothing because this act alone prevents many bystanders from initiating bystander CPR. Bystanders are to place the fallen individual on his or her back on a hard surface or on the floor, to place the heel of one hand in the center of the patient’s chest (on the sternum, usually between the nipples), with the heel of the other hand on top of the first. They are to lock the elbows so the arms are straight, and with the shoulders above the center of the patient’s chest, to fall so the weight of their upper body compresses the patient’s chest. Few if any are strong enough to do adequate chest compressions using just the muscles of their upper extremities. The compression rate should be 100/min. Lifting the hands or the heel of the bottom hand completely off the chest after each compression is necessary to allow full chest recoil and is specifically emphasized (see later discussion).47 This is an important issue and one reason that external chest compressions should not be referred to as external cardiac massage. Massage implies continuing pressure and continuing pressure or any lean on the chest during the release phase of chest compression decreases forward blood flow and survival. If more than one rescuer is present, they are to trade off doing chest compressions after each 100 or 200 compressions because, properly done, continuous chest compressions at 100/min is very tiring, especially for older individuals.
Full Chest Wall Recoil Following Chest Compressions is Essential
Full chest wall recoil during the release phase of each chest compression is extremely important.47 During the release phase of chest compression, a small negative pressure is created within the chest as the chest wall recoils back to its resting position.47 This draws venous blood back into the right heart from the systemic veins and may draw air into the airways. Incomplete chest recoil compromises perfusion because it interferes with the generation of this negative pressure in the chest, and thus decreases venous blood return to the heart. As a consequence, cardiac output and perfusion pressures are reduced. Incomplete chest recoil has been reported in 46% of simulated resuscitations performed by paramedics.47 Furthermore, when incomplete chest recoil was combined with excessive ventilations, perfusion was severely compromised.47
Dispatch-Directed Chest-Compression-Only CPR Generally Accepted
A part of the first component of CCR consists of new recommendations for dispatch-directed bystander resuscitation.42 Continuous chest compression CPR or chest-compression-only bystander resuscitation instructions are given by phone from EMS dispatch centers. This approach is now generally followed in most metropolitan cities in the United States.
What Is the Role of Gasping or Agonal Respirations?
Gasping or agonal respirations are common early on following cardiac arrest. Clark, Eisenberg, and associates reported gasping in 56% of patients with OHCA on arrival of paramedics.48 Gasping or agonal breathing is probably more common soon after cardiac arrest and is more common in individuals who receive bystander CPR. When these forms of abnormal breathing occur in patients with cardiac arrest, it is both unfortunate and fortunate. It is unfortunate because gasping or agonal breathing may be interpreted by uninformed lay individuals as an indication that the person who collapsed is still breathing and therefore delay initiating bystander resuscitation and the activation of the emergency medical services. However, gasping is fortunate because if recognized for what it is (e.g., agonal breathing), and chest compressions are promptly initiated, the subject is likely to continue to gasp and provide physiologic self-ventilations. And if continuous chest compressions are initiated, the nongasping subject is more likely to begin gasping. The longer the duration of untreated VF before the initiation of resuscitation efforts, the longer the duration of bystander CPR efforts before gasping resumes.
Clark and associates also reported that gasping or agonal breathing was highly correlated with survival.48 We have found similar results in our swine model of OHCA laboratory. Animal research laboratories that use paralysis as part of the protocol when studying CPR eliminate this physiologically important reflex. It is our opinion that results in paralyzed animals cannot be applied to humans who are not paralyzed when they have cardiac arrest.
Emergency Medical Services Components of Cardiocerebral Resuscitation
The first component of CCR is continuous chest compression CPR for bystanders.4 The second component of CCR consists of a new algorithm for ACLS (see Fig. 52-2).5 Law officers and other EMS rescuers who are equipped with AEDs are to defibrillate immediately only if they personally witness the collapse or if good continuous chest compression CPR is being provided by a bystander when they arrive.5 Otherwise, they are to bare the chest and attach the defibrillator pads if using an AED or hand-held defibrillation electrodes and promptly perform forceful uninterrupted chest compressions at 100 compressions per minute for 2 minutes (200 compressions) before quick rhythm analysis and prompt defibrillation if indicated (see Fig. 52-3).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree