56 Cardiac Imaging and Stress Testing
• Cardiac imaging and stress testing are key components of any comprehensive patient evaluation for possible acute coronary syndromes or coronary heart disease.
• Exercise or pharmacologic stress testing is used to risk-stratify patients and determine the presence of stress-induced ischemia.
• Rest myocardial perfusion imaging assesses for ischemia during symptoms at the time of evaluation, whereas stress testing evaluates for stress-induced (exercise or pharmacologic) ischemia.
• Rest myocardial perfusion imaging can be a useful tool for risk stratification and diagnosis in patients with active or recent chest discomfort (<2 hours).
• Echocardiography can be used to assess global cardiac function and may be performed with the patient at rest or with stress.
• Electron beam computed tomography is gaining momentum as an imaging technology that is potentially useful in the emergency department environment.
• Several chest pain unit protocols using various combinations of cardiac biomarkers, imaging modalities, stress testing, and time courses of evaluation have proved successful in many environments.
• Individual institutions and their emergency departments should develop their own custom protocols to best care for patients in that community given the resources available, personnel, and practice patterns.
Background and Scope
The diverse group of patients with symptoms of chest discomfort remains a significant challenge for the emergency physician (EP). High-risk patients with classic angina and young, low-risk patients with atypical symptoms represent only a fraction of those with chest discomfort seem in the everyday emergency department (ED) setting. Frequently, patients have one or two risk factors and some but not all of the classic ischemic symptoms, and the findings on an electrocardiogram (ECG) are nondiagnostic. These patients carry up to a 10% chance of significant cardiac disease and need appropriate risk stratification and diagnostic evaluation.1 As EPs, our goal is not to diagnose the condition of coronary heart disease but, rather, to stratify patients’ risk and identify those at risk for imminent cardiac ischemia and poor outcomes.
EPs use several methods and modalities to evaluate this very heterogenous patient group, each of which has benefits and limitations. Aside from a comprehensive history and physical examination, standard adjuncts include an ECG, serial cardiac biomarker measurements, and some choice of cardiac imaging. The ECG, though often considered the principal diagnostic tool in cardiac evaluation, is the most basic and rapid way to image the heart. Elevations in available cardiac biomarkers indicate the end result of ischemic myocardium and signify myocardial necrosis or cell death. Cardiac imaging indirectly reflects cardiac anatomy and tissue function with the goal of revealing occult cellular ischemia at risk for cell death. Cardiac imaging can be performed with the patient at rest or under physical or pharmacologic stress. Some of the factors to be considered for the appropriate choice of imaging modality include patient selection, exposure to radiation (Table 56.1), and availability of reagents, technology, and personnel to perform the study and interpret the results.2 The goal of this chapter is to familiarize the reader with common cardiac imaging modalities used in the ED for the evaluation of this difficult and high-risk population.
Table 56.1 Approximate Radiation Exposure with Common Imaging Studies as Part of Cardiac Evaluation
| STUDY | MEAN EFFECTIVE DOSE (MILLISIEVERTS) |
|---|---|
| Chest radiograph | 0.02 |
| Echocardiogram | 0 |
| Myocardial perfusion imaging | 15 |
Ventilation-perfusion ( ) scan ) scan | 1.2-2 |
| Computed tomographic (CT) angiography of the chest (noncoronary) | 15 |
| CT angiography (coronary) | 8-15 |
| Percutaneous coronary intervention | 7-15 |
Adapted from Fazel R, Krumholz HM, Wang Y, et al. Exposure to low-dose ionizing radiation from medical imaging procedures. N Engl J Med 2009;361:849–57.
Electrocardiogram
An ECG should be obtained within 10 minutes of a patient’s arrival at the ED.3 Though often considered to be the most important diagnostic and prognostic tool available, ECGs rather primitively indicate only gross electrical derangements caused by dead or dying muscle tissue. Serial ECGs during progression or regression of a patient’s symptoms can be helpful, similar to procuring prior ECGs from a previous medical visit.
Chest Roentgenogram
Though not usually considered to be a cardiac imaging modality, the chest radiograph is an important diagnostic tool in the evaluation of patients with chest pain. Probably the most useful function of the chest radiograph lies in identifying or suggesting alternative diagnoses for the patient’s symptoms. Chest radiographs are safe and result in relatively low radiation exposure (0.02 millisievert) when compared with the cardiac-specific modalities (see Table 56.1). Pneumothorax or pneumonia can be identified on a chest radiograph. Mediastinal widening, apical capping of pleural fluid, tracheal deviation, or displacement of intimal calcium from the outer vessel wall may indicate aortic dissection. An enlarged cardiac silhouette may signify the presence of a pericardial effusion or, if seen together with pulmonary congestion, congestive heart failure. Pulmonary emboli may be accompanied by focal oligemia, wedge-based densities, or enlarged pulmonary arteries on chest radiographs. Every patient with chest discomfort should have a chest radiograph taken before additional evaluation.
Exercise Treadmill Testing
Graded exercise testing is a popular method of cardiac stress testing in both the inpatient and outpatient settings. Many of the early ED accelerated diagnostic protocols used this test after initial risk stratification via cardiac biomarkers and the ECG.4–8 This was the beginning of chest pain unit protocols and the ability to appropriately risk-stratify ED patients with chest pain within 6 to 12 hours. Outcomes at 6 to 12 months have been found to be similar with very few adverse events between patients admitted to the hospital and those cared for in an ED chest pain unit setting. Although exercise treadmill testing has a lower positive predictive value (great proportion of false-positive results) than some other more contemporary myocardial perfusion imaging (MPI) modalities, its use still diminishes unnecessary admissions.9
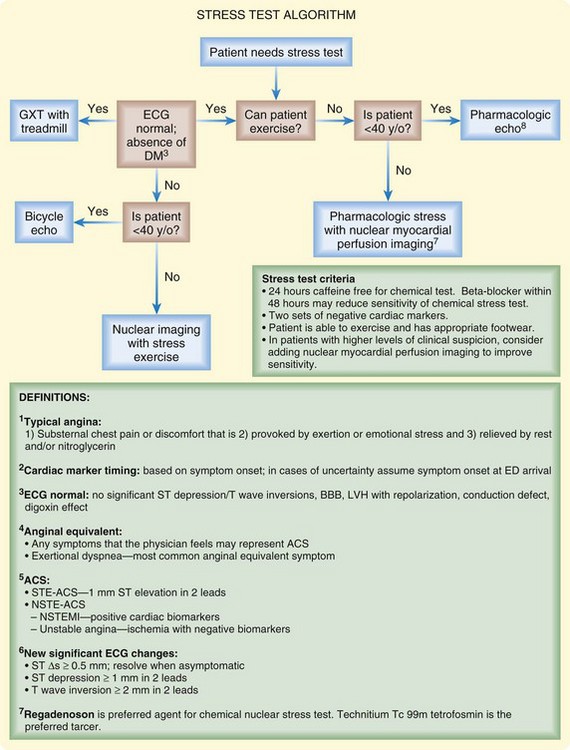
Selection criteria for exercise testing are more restrictive than those for other imaging modalities. Patients must be able to walk on a treadmill, and findings on the ECG should be normal or show no new changes. Agents such as dobutamine, dipyridamole, adenosine, or regadenoson can be used in lieu of exercise. Although exercise testing is slowly being supplanted by studies offering more detailed functional information, it is still a major tool in many centers (Fig. 56.1).