Cardiac Anatomy and Physiology
The heart is a phasic, variable speed, muscular pump that is electrically self-sustaining and provides its own blood supply (Pagel PS, Kampine JP, Stowe DF. Cardiac anatomy and physiology. In: Barash PG, Cullen BF, Stoelting RK, Cahalan MK, Ortega R, Stock MC, eds. Clinical Anesthesia. Philadelphia: Lippincott Williams & Wilkins; 2013: 237–262). The two pair of atria and ventricles of the heart are elastic chambers that are arranged to supply equal amounts of blood to the pulmonary and systemic vasculature. The contractile function of the atria and ventricles and the ability of these chambers to adequately fill without excessive pressure determine overall cardiac performance. Thus, abnormalities in systolic or diastolic function may lead to heart failure. Comprehensive knowledge of cardiac anatomy and physiology is crucial for modern anesthesia practice.
I. Gross Anatomy
Architecture
A flexible, cartilaginous structure forms the heart’s skeleton and is composed of the annuli of the cardiac valves, the aortic and pulmonary arterial (PA) roots, the central fibrous body, and the left and right fibrous trig ones. This foundation of cartilage creates support for the valves and maintains the heart’s structural integrity in the presence of developed internal pressures.
Subendocardial and subepicardial muscle fibers of the left ventricle (LV) are oriented in perpendicular, oblique, and helical planes (“figure of eight”) that allows a LV “twisting” motion thus enhancing LV systolic force. Loss of this helical-rotational action contributes to a decrease in ejection fraction (EF) during the development of congestive heart failure (CHF).
The crescent-shaped right ventricle (RV) is anatomically anterior and to the right of the LV. This chamber propels deoxygenated venous blood into the relatively compliant, low-pressure PA tree.
Valve Structure
Two pairs of translucent, macroscopically avascular valves guarantee unidirectional movement of blood through the heart.
The pulmonic and aortic valves separate the RV and LV from the PA and aorta, respectively. These valves open and close and operate passively with changes in pressure resulting from RV and LV contraction and relaxation.
The sinuses of Valsalva are dilated segments in the proximal aortic root that are located immediately superior to each aortic leaflet.
The mitral valve, located between the left atrium (LA) and the LV, opens in response to a positive pressure gradient between the LA and LV. Closure of the leaflets occurs as retrograde blood flow moves toward the valve during early systole.
The chordae tendineae act as “cable stays” to prevent leaflet prolapse and inversion during LV contraction.
The mitral valve apparatus is critical for overall LV function (guarantees that blood flow from the LA to the LV is unidirectional).
Ischemia or infarction of a papillary muscle may cause dysfunction of the mitral apparatus and is often accompanied by acute mitral regurgitation.
The tricuspid valve is composed of anterior, posterior, and septal leaflets, and assures unidirectional movement of blood from the right atrium (RA) and RV. In contrast to the mitral valve, the tricuspid valve does not have a collagenous annulus but originates from the atrioventricular (AV) groove (also contains the right coronary artery that must be carefully avoided during tricuspid valve surgery) that separates the RA from the RV.
Coronary Blood Supply
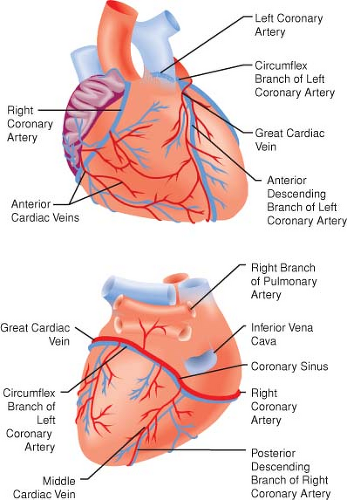
The left anterior descending (LAD), left circumflex (LCCA), and right coronary (RCA) arteries supply blood to the LV (Fig. 10-1).
Most coronary blood flow to the LV myocardium occurs during diastole because aortic blood pressure is greater than LV pressure. A critical stenosis or acute occlusion of
one of these three vessels may produce myocardial ischemia or infarction accompanied by abnormal regional contractile function based on the known distribution of each coronary artery’s blood supply (Table 10-1).
The “dominance” of the coronary circulation is determined on the basis of which major coronary artery feeds the posterior descending coronary artery (PDA). A “right-dominant” circulation occurs when the RCA supplies blood to the PDA and is observed in approximately 80% of patients. A “left-dominant” circulation in which the PDA is supplied by the LCCA is observed in the remaining 20% of patients.
RA, LA, and RV coronary perfusion occurs during both systole and diastole because aortic blood pressure always exceeds the pressure within each of these chambers (Fig. 10-2).
The extent of development of the coronary collateral circulation may determine whether myocardial ischemia or infarction is likely in patients with coronary artery disease.
The coronary veins converge and terminate in the coronary sinus, which empties into the posterior aspect of the RA above the tricuspid valve (accounts for about 85% of the total coronary blood flow to the LV. The remaining blood flow empties directly into the atrial and ventricular
cavities via the thebesian veins. The RV veins drain into the anterior cardiac veins; these empty individually into the RA.
Impulse Conduction
How the heart is electrically activated is essential to its mechanical performance. The primary cardiac pacemaker is the sinoatrial node, although declines in firing rate and delays or blockade of normal conduction may result in the appearance of secondary pacemakers.
The atria are electrically isolated from the ventricles by the heart’s cartilaginous skeleton. As a result, atrial depolarization is directed solely to the RV and the LV through the AV node. Because AV node conduction is relatively slow compared with the pathways proximal and distal to it, the AV node is responsible for the sequential contraction pattern of the atria and the ventricles.
Accessory pathways that bypass the AV node and establish abnormal conduction between the atria and ventricles may produce supraventricular tachyarrhythmias.
Table 10-1 Areas at Risk for Myocardial Ischemia Based on Coronary Artery Distribution | ||
|---|---|---|
|