103 Calculous and Acalculous Cholecystitis
Acute cholecystitis has long been recognized as a complication of surgery or acute critical illness. The first reported case of acute postoperative cholecystitis, described in 1844, was a lethal complication that occurred in a patient who had been treated for a strangulated femoral hernia.1 In 1902, Kocher and Matti described successful operation for gangrenous cholecystitis complicating a ventral herniorrhaphy.2 In 1962, Thompson et al. reported a series of 98 patients who developed acute cholecystitis in the postoperative period.3 Seventy-six percent were men, and 47% did not have gallstones. Twelve percent of the patients developed perforation of the gallbladder. It is noteworthy that Glenn and Becker showed that the incidence of acalculous and postoperative cholecystitis increased between 1955 and 1979.4
The pathophysiology of cholecystitis in critically ill patients is different from that in the general population. At least half of the cases are acalculous.5 Understanding this disease process can help increase the index of suspicion and lead to early diagnosis and treatment, which is necessary for good outcomes in the already critically ill patient.
 Risk Factors and Pathophysiology
Risk Factors and Pathophysiology
Acalculous cholecystitis also can spontaneously occur under certain circumstances. In outpatients, risk factors for acalculous cholecystitis include diabetes mellitus, vasculitis, older age, and male sex.6 Acalculous cholecystitis also has been reported in cancer patients and patients with systemic infections and the acquired immunodeficiency syndrome (AIDS). Indeed, acute cholecystitis is the most common indication for exploratory laparotomy or laparoscopy in AIDS patients.7 Most have acalculous disease. Not surprisingly, the mortality rate is high. In children, the majority of cases of acute cholecystitis are acalculous.8 The etiology appears to be dehydration or lymphadenopathy secondary to viral infections. Congenital biliary tract anomalies also need to be considered.
Acute cholecystitis has been described in multiple reports as a complication of a variety of surgical procedures,9–14 trauma,15–20 burns,21 sepsis,22 cardiovascular diseases, and malignancy.23,24 There also has been an association with total parenteral nutrition and biliary stasis.25–28 The pathophysiology, however, remains unclear.
Theories regarding the pathogenesis of acalculous cholecystitis in critically ill and postoperative patients have evolved over the years. Sparkman was the first to suggest that gastrointestinal hypomotility and biliary stasis were causative factors.29 Glenn and Wantz added that the lack of enteral feeding in the postoperative period increased the concentration of bile salts and cholesterol in bile.30 They further noted acute onset of cholecystitis with refeeding, suggesting impaction of stones or viscous bile in the cystic duct, with gallbladder contractions. Thompson et al., having noted gallbladder mucosal necrosis, arterial thrombosis, gangrene, and perforation, suggested that hypoperfusion may be the critical mechanism for acalculous cholecystitis.3 A recent histopathologic study found that two-thirds of surgical and trauma patients who developed acute cholecystitis had ischemic cholecystitis histologically.31 Hakala et al. performed ex vivo microangiography of gallbladders immediately after cholecystectomy.32 Patients with stones had normal vasculature, whereas those with acalculous disease had poor and irregular capillary filling, suggesting that microvascular disturbances may play a role in the pathogenesis of this disease. Hypoperfusion, particularly of the splanchnic circulation, is common in critically ill patients. Etiologic factors include hemorrhage, dehydration, heart failure, and/or sepsis. The use of vasopressors can exacerbate the situation. Mechanical ventilation with positive end-expiratory pressure (PEEP) can increase hepatic venous pressure and thereby decrease portal perfusion.34
Orlando et al. suggested that in addition to hypoperfusion, increased intraluminal pressure may be a critical factor.33 Biliary stasis secondary to fasting and narcotics may play a critical role in increasing intraluminal pressure in the gallbladder. The combination of hypoperfusion and increased luminal pressure leads to a decrease in gallbladder perfusion pressure. Bacterial invasion can subsequently occur in the ischemic tissue.
The use of parenteral nutrition has been implicated in the pathogenesis of acalculous cholecystitis. In addition to the effects of fasting, parenteral nutrition can decrease bile production, worsening biliary stasis. Biliary sludge can be found in almost all patients on long-term parenteral nutrition.25–28 Many go on to form gallstones. Trauma patients also develop sludge over time, and this factor may play a role in the development of cholecystitis, as well as pancreatitis.35
Eosinophilic infiltration of the inflamed gallbladder has been seen in patients developing acute acalculous cholecystitis after administration of antibiotics for other reasons, suggesting the possibility that a hypersensitivity reaction to the antibiotic played an etiologic role.36 This theory has not been substantiated.
It has been suggested that the pigment load from massive transfusions can lead to changes in the relative concentrations of bile pigments compared to cholesterol and lecithin in bile, increasing risk of acalculous cholecystitis. Long et al., however, found no relationship between transfusion requirements and risk of cholecystitis.34
 Incidence
Incidence
The incidence of acute cholecystitis in the ICU is difficult to determine given the great diversity of ICU patient populations and illness severity. Among cardiac surgical patients, acute cholecystitis is second only to upper gastrointestinal hemorrhage as an indication for abdominal operation.37 About half the cases of acute cholecystitis in this population are due to acalculous disease. Visceral hypoperfusion related to left ventricular dysfunction has been implicated as an etiologic factor. Rady et al. found that early predictors of acute cholecystitis included arterial occlusive disease, low preoperative oxygen delivery, longer cardiopulmonary bypass times, need for surgical re-exploration, cardiac arrhythmias, mechanical ventilation for ≥ 3 days, bacteremia, and nosocomial infections.13 The common threads of these factors are decreased tissue perfusion and oxygenation, significant surgical trauma (which would be expected to lead to production of inflammatory mediators), and perhaps bacterial translocation from the gut lumen. These authors went so far as to suggest that patients who have had a complicated postoperative course should be followed by serial ultrasonography of the gallbladder. Hagino et al. found that 6 of 7 patients who developed cholecystitis after aortic reconstruction had prolonged hypotension and developed multiple organ dysfunction; 5 died.14
In the general population of postoperative patients, acute cholecystitis appears to occur with or without gallstones. Mortality is about 30%. Among trauma patients, about 90% of cases of acute cholecystitis are acalculous.15–20 The percentage of cases of acute cholecystitis that are acalculous has increased significantly over time.4 Because the incidence of the disease is low, but the many risk factors for the disease are common, it is difficult to identify specific groups of ICU patients who might benefit from selective screening for acute cholecystitis.
 Clinical Presentation
Clinical Presentation
The most consistent laboratory finding is a leukocytosis. Elevated circulating levels of liver enzymes and bilirubin are common, but not necessarily present. Clinical findings and laboratory studies are not very sensitive or specific for cholecystitis even in the general population38,39 and are less so in critically ill patients. Consequently, radiologic studies are necessary.
 Imaging Studies
Imaging Studies
Ultrasonography has proven to be an accurate radiologic test for acute cholecystitis in the general population. In the ICU, the presence or absence of gallstones does not help with the diagnosis. The most useful ultrasonographic findings indicative of acute cholecystitis are thickening of the gallbladder wall and pericholecystic fluid (Figure 103-1). Ultrasonographic findings correlate well with operative findings. False-positive findings may occur with sludge, non-shadowing stones, cholesterolosis, ascites, hypoalbuminemia, and portal hypertension. Other ultrasonographic findings indicative of acute cholecystitis include the “double wall sign,” representing edema of the gallbladder wall; the “halo sign,” representing sloughed gallbladder mucosa; intramural gas; distention of the gallbladder; and the “sonographic Murphy’s sign,” demonstrating point tenderness over the gallbladder. The sensitivity of ultrasound for detecting acalculous cholecystitis is 81% to 92%. The specificity is 60% to 96%.38–42,47,48 One problem is that the typical ultrasonographic findings of cholecystitis can be seen in ICU patients without other evidence of cholecystitis. For example, Boland et al. performed ultrasound examinations of the gallbladder twice a week in a variety of ICU patients.40 Half of the patients without calculi developed at least one ultrasonographic finding of acute cholecystitis. Helbich et al.41 attempted to apply a scoring system to the ultrasonographic findings characteristic of acute cholecystitis, suggesting that patients with several findings should undergo more aggressive diagnostic evaluation and perhaps therapeutic interventions.40 In equivocal cases, serial examinations may demonstrate increasing wall thickness which should increase the suspicion for cholecystitis.42

Figure 103-1 Ultrasound of gallbladder, demonstrating wall thickening (double arrows) and sludge (black arrow).
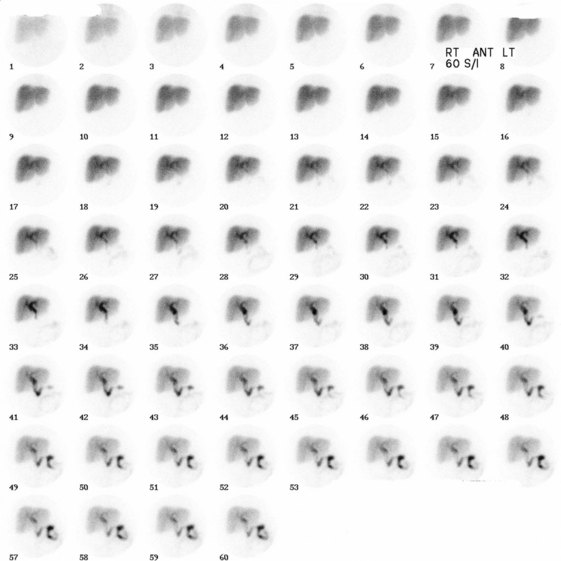
Scintigraphy of the gallbladder frequently has been used when acute cholecystitis is suspected, but the findings from other tests such as ultrasound are inconclusive or contradictory. Gallbladder scintigraphy is performed by administering technetium-labeled iminodiacetic acid (IDA). Cholecystitis is diagnosed if the radioactive tracer is visualized in the small bowel without visualization of the gallbladder within 4 hours, suggesting occlusion of the cystic duct (Figure 103-2). Delayed visualization of the gallbladder may represent chronic cholecystitis. The rate of false-positive tests is significant in fasting patients, particularly those receiving parenteral nutrition. The use of intravenous morphine to increase tone in the sphincter of Oddi and thereby increase pressure within the biliary system can decrease the risk of a falsely positive test.43 The sensitivity of scintigraphy is 91% to 97%. The specificity is 38% to 99%.43,44,48 Scintigraphy is a useful complement to ultrasonography when ultrasonography alone does not provide enough information to permit a sufficiently early decision regarding intervention.44
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree