CHAPTER 79 BURNS
The frequency of burn injury and its subsequent multisystem effects make the treatment of burn patients a commonly encountered management challenge for the trauma/critical care surgeon. The emergency surgery components of initial burn care include fluid resuscitation and ventilatory support, as well as preservation and restoration of remote organ function. Following appropriate resuscitation, burn patient management is focused on wound care and provision of the necessary metabolic support. The involvement of the emergency/trauma surgeon in burn wound management is dependent on the extent and depth of the wound and the rapid identification of those patients who are best cared for at a burn center.
INCIDENCE
The precise number of burns that occur in the United States each year is unknown because only 21 of 50 states mandate the reporting of burn injury. An estimated total number of burns has been obtained by extrapolation of those data. At present, 1.25 million is regarded as a realistic estimate of the annual incidence of burns in the United States, 80% of which involve less than 20% of the total body surface. Approximately 190–263 patients per million population are estimated to require admission to a hospital for burn care each year. In the population of burn patients requiring hospital care, there is a smaller subset of approximately 20,000 burn patients who, as defined by the American Burn Association (Table 1), are best cared for in a burn center each year. This subset consists of 42 patients per million population with major burns, and 40 patients per million population having lesser burns but a complicating cofactor.
Table 1 Burn Center Referral Criteria
a If the mechanical trauma poses the greater immediate risk, the patient may be stabilized and receive initial care at a trauma center before transfer to a burn center.
Adapted with permission from Stabilization, Transfer and Transport, Chapter 8. In Advanced Life Burn Support Course Instructors Manual. Chicago, American Burn Association, 2001, pp. 73–78.
PATHOPHYSIOLOGY
Local Effects
Burn injury causes three zones of damage. Centrally located is the zone of coagulation. In a full-thickness burn, the zone of coagulation involves all layers of the skin, extending down through the dermis and into the subcutaneous tissue. In partial-thickness injuries, this zone extends down only into the dermis, and there are surviving epithelial elements capable of ultimately resurfacing the wound. Surrounding the zone of coagulation is an area of lesser cell injury, the zone of stasis. In this area, blood flow is altered but is restored with time as resuscitation proceeds. If patients are inadequately resuscitated, thrombosis can occur and the zone of stasis can be converted to a zone of coagulation. The most peripheral zone is an area of minimally damaged tissue, the zone of hyperemia, which abuts undamaged tissue. The zone of hyperemia is best seen in patients with superficial partial-thickness injuries as occur with severe sun exposure.
Systemic Response
Burn injury affects the hematopoietic system, resulting in the loss of balance in both leukocyte and erythrocyte production and function. Burns of greater than 20% of total body surface area are associated with both alterations in red cell production and increases in red cell destruction at the level of the cutaneous circulation, resulting in anemia. Such anemia can be further compounded by frequent phlebotomy, surgical blood loss, hemodilution due to resuscitation, and transient alterations in erythrocyte membrane integrity. Longer-term changes appear to be related to hyporesponsiveness of the erythroid progenitor cells in the bone marrow to erythropoietin. During the early stages of resuscitation, reductions in platelet number, depressed fibrinogen levels, and alterations in coagulation factors return to normal or near normal values with appropriate resuscitation. Changes in white cell number occur early, with an increase in neutrophils due to demargination and accelerated bone marrow release. With uncomplicated burn injury, bone marrow myelopoiesis is preserved.
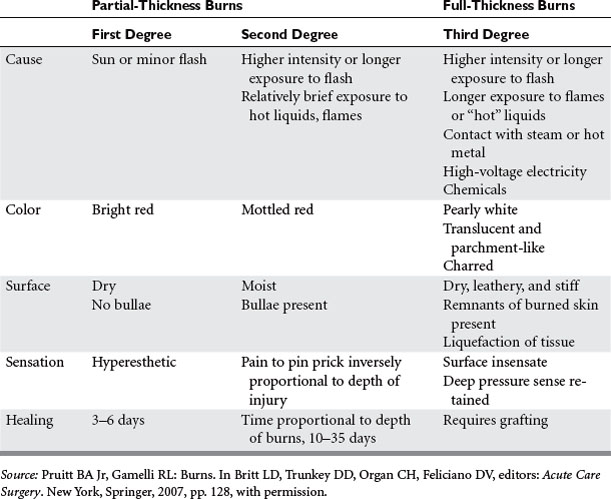
GRADING OF BURN WOUND DEPTH
The injuries that will be apparent on examination are the consequences of the level of tissue destruction. Wounds that are superficial are associated with hyperemia, fine blistering, increased sensation, and exquisite pain upon palpation. The wounds are hyperemic, warm, and readily blanch. These types of injuries represent firstdegree burns or are alternatively termed superficial partial-thickness injuries. With a second degree or deeper partial-thickness burn, the wound presents with intact or ruptured blisters or is covered by a thin coagulum termed “pseudoeschar.” The key physical finding is preservation of sensation in the burned tissue, although it is reduced (Table 2). With proper care, superficial and even deeper partial-thickness injuries are capable of spontaneous healing without grafting. The risk of infection in deep partial-thickness wounds is significant, and if an infection develops it can lead to a greater depth of skin loss. A full-thickness wound occurs when the injury penetrates all layers of the skin or extends into the subcutaneous or deeper tissues. These wounds will appear pale or waxy, be anesthetic, dry, and inelastic, and contain thrombosed vessels. Occasionally in children or young women, the initial appearance of a wound may be more that of a brick red coloration. Such wounds will have significant edema and are inelastic and insensate. Full-thickness wounds are infection-prone wounds, as they no longer provide any viable barrier to invading organisms and if left untreated become rapidly colonized and a portal for invasive burn wound sepsis.
RESUSCITATION PRIORITIES
Fluid Administration
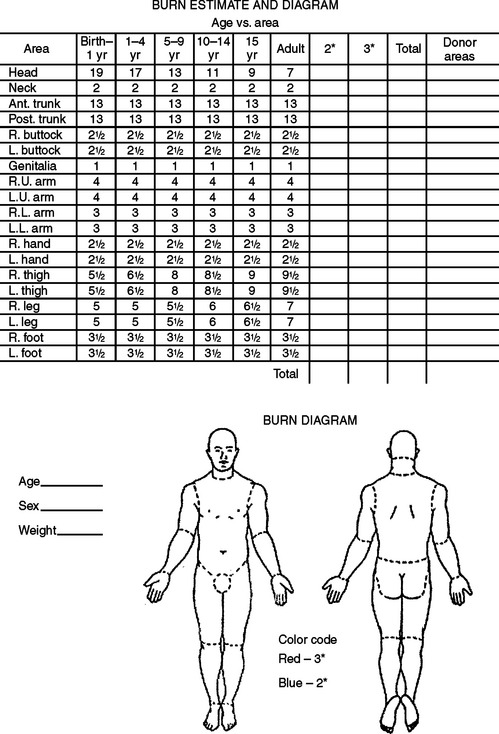
Resuscitation fluid needs are proportional to the extent of the burn (combined extent of partial- and full-thickness burns expressed as a percentage of total body surface area) and are related to body size (most readily expressed as body weight) and age (the surface area per unit of body mass is greater in children than in adults). The patient should be weighed on admission and the extent of partial- and full-thickness burns estimated according to standard nomograms (Figure 1). The fluid needs for the first 24 hours can be estimated on the basis of the Advanced Burn Life Support and Advanced Trauma Life Support consensus formula (Table 3).
Table 3 Fluid Required for the First 24 Hours Post-Burn
BW, Body weight; LR, lactated Ringer’s; TBSAB, total body surface area burned.
The limited glycogen stores in a child may be rapidly exhausted by the marked stress hormone response to burn injury. Serum glucose levels in the burned child should be monitored, and 5% dextrose in lactated Ringer’s administered if serum glucose decreases to hypoglycemic levels. In the case of small children with small burns, the resuscitation fluid volume as estimated on the basis of burn size may not meet normal daily metabolic requirements. In such patients, maintenance fluids should be added to the resuscitation regimen.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree