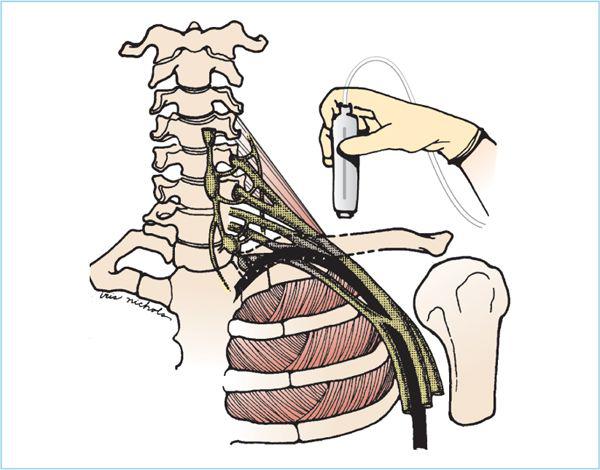
Figure 12.1. Brachial plexus overview: The ventral roots of the fifth cervical through the first thoracic spinal nerves form the brachial plexus. The upper and lower pairs of roots merge, creating three trunks, which join the subclavian artery as it crosses the first rib. The trunks then divide and recombine to form three cords and then divide into the four terminal nerves of the forearm, which surround the axillary artery—the radial, median, ulnar, and musculocutaneous.
E. Terminal nerves. Axillary block is performed at the level of the terminal nerves, where there is greater variability of anatomy (1).
1. The three main terminal nerves to the hand remain closely approximated to the axillary artery, with the median generally superior to the vessel and the others inferior and posterior, but with considerable variability in location.
2. Sensory branches to the forearm have already departed the neurovascular bundle at this level and travel in the coracobrachialis muscle (musculocutaneous) or in the subcutaneous tissues (medial brachial cutaneous, medial antebrachial cutaneous).
F. Although knowledge of these derivations is helpful, the approach to brachial plexus anesthesia is based on the reproducible landmarks of the neck—the vertebral tubercles, the first rib, the coracoid process, or the axillary artery.
G. Each injection site produces a unique pattern of distribution of anesthesia (2).
1. Interscalene anesthesia is most reliable and dense on the upper roots (C5-7) and includes sensory anesthesia of the cervical plexus (C2-4). Occasionally, anesthesia is ineffective in the C8-T1 dermatome (ulnar side of arm) distribution (Figure 12.2). This technique is therefore best suited for shoulder and upper arm surgery.
2. The supraclavicular block is performed where the trunks and divisions are most closely approximated in the fascial bundle and before branching occurs, and is therefore the most reliable in producing sensory anesthesia of the entire forearm and hand. It does not reliably provide cervical plexus (shoulder) anesthesia.
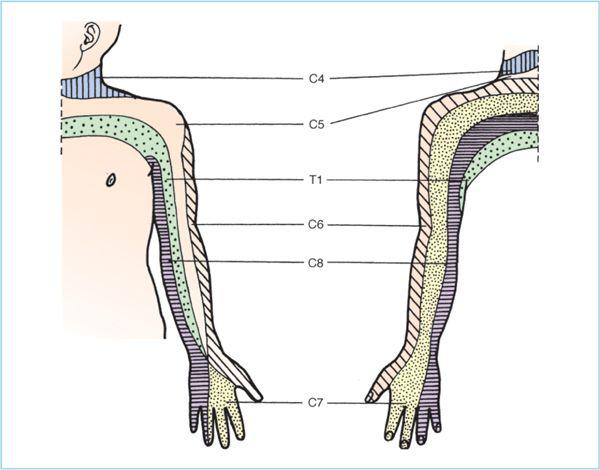
Figure 12.2. Dermatomal distribution of nerve roots in the upper extremity. Interscalene blocks, which are at the level of the roots, will anesthetize the brachial plexus along dermatomal distribution.
3. At the target of the infraclavicular block, the cords are separated from each other (into lateral, posterior, and middle cords) by the axillary artery below the fascial plane of the perimysium of the pectoralis minor muscle. The MC nerve may diverge from the lateral cord above the level of the pectoralis minor. The divergent arrangement of the cords makes complete anesthesia more difficult compared to the supraclavicular block.
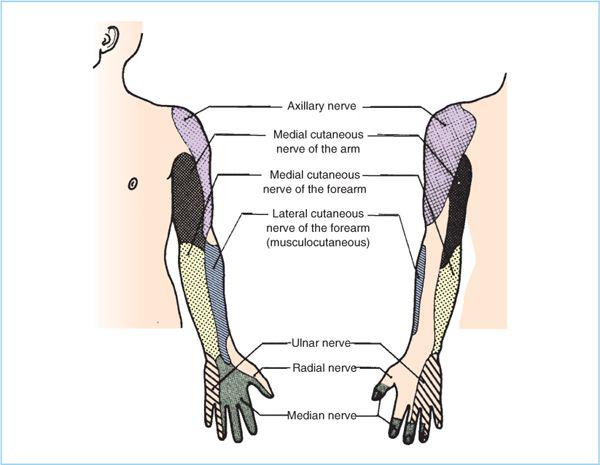
4. The axillary block is reliable in anesthetizing the three nerves of the hand (radial, median, and ulnar) (Figure 12.3). The MC and medial antebrachial cutaneous nerves and their sensory distribution in the forearm can be spared because these nerves depart from the perivascular bundle high in the axilla.
H. The concept of the “sheath”
1. Aproximal fascial envelope arises from the lateral extension of the posterior fascia of the AS and anterior fascia of the MS muscles, and extends from the transverse processes for a variable distance in the upper arm.
2. Winnie has popularized the use of this “sheath” to allow single-injection techniques for the brachial plexus at all levels in the sheath and has demonstrated extensive spread of solution from single injections (3).
Figure 12.3. Sensory dermatomes of the terminal nerves of the upper extremity. Sensation is provided by the terminal nerves as identified. This pattern is different from the classic dermatomal distribution of the nerve roots (Figure 12.2) and is seen when the brachial plexus is blocked more distally, such as with an axillary block.
3. Distally within this sheath, fascial septa may be present (4). Although they do not universally limit the spread of anesthetic solutions (5), they may defeat attempts to produce anesthesia by injection of a single bolus of solution. These septa may account for less than 100% success rate of single-injection axillary anesthesia.
II. Drugs
A. Local anesthetics (LAs) are chosen primarily for the duration of the anesthetic block.
1. Lidocaine 1% or 1.5% may provide 3 to 4 hours of anesthesia.
2. Mepivacaine 1.5% may provide 4 to 5 hours of anesthesia.
3. Bupivacaine, levobupivacaine, or ropivacaine (0.5%) will provide 12 to 14 hours of analgesia.
4. There is no need for higher concentrations in brachial plexus anesthesia, and there is a risk of exceeding maximum recommended doses if they are employed.
B. The volume to be injected has been subject to debate. A 25 mL of solution injected directly in the neighborhood of a nerve stimulation or paresthesia will provide anesthesia for most patients.
1. The upper limit is generally recognized as 50 mL because this quantity represents the maximum milligram dose of most of the LAs employed.
2. A 30 to 40 mL dose is more commonly used.
3. Although larger volumes may give slightly earlier onset and further spread and are advocated by some (2), studies have demonstrated adequate spread with 40-mL volumes in all areas of injection. Because many of the techniques require an additional 5 or 10 mL of supplemental anesthetic solution for intercostobrachial branches or peripheral block of the ulnar nerve, it seems appropriate to limit injection into the neurovascular bundle to 40 mL.
C. Continuous catheter techniques employ dilute concentrations of long-acting amide LAs such as 0.2% ropivacaine or 0.125% bupivacaine at rates of 6 to 8 mL/h.
D. Adjuncts
1. Epinephrine
a. In 1:400,000 dilution, epinephrine helps to detect intravascular injection and does not prolong duration (may slightly decrease duration).
b. In 1:200,000 dilution, epinephrine:
(1) Prolongs duration of block, especially with lidocaine and mepivacaine
(2) May reduce peak systemic blood levels
(3) May increase risk of nerve damage in patients with underlying neuropathy or with intraneural injection (6)
2. Clonidine
a. May prolong analgesia in a dose-dependent manner.
b. Side effects are minimal if dose is limited to 150 μg.
c. When added to mepivacaine, an additional 4 hours of analgesia can be provided (7).
3. Sodium bicarbonate
a. Hastens onset of block by raising the pH of the solution closer to the pKa of the LA (more molecules in nonionized form to cross the nerve sheath and membrane).
b. This faster onset is more evident when added to commercially prepared LAs with epinephrine because these solutions are marketed with a lower pH.
c. In plain LAs (with or without freshly added epinephrine), it may not significantly speed onset and may decrease duration.
d. Precipitation of solution can occur if too much bicarbonate is added, especially with ropivacaine and bupivacaine.
e. For lidocaine and mepivacaine, 1 mL of 8.4% sodium bicarbonate is added to every 10 mL of LA.
III. Techniques
A. Interscalene block
This approach is ideal for upper arm and shoulder (acromioplasty, etc.) operations. Although the incidental cervical plexus (C2-4) anesthesia may be advantageous, “ulnar” (C8-T1) sparing may occur, such that this block may require supplementation in the axilla or above the elbow if used for hand surgery. US guidance is effective for this block, although traditional peripheral nerve stimulator or paresthesia techniques work well.
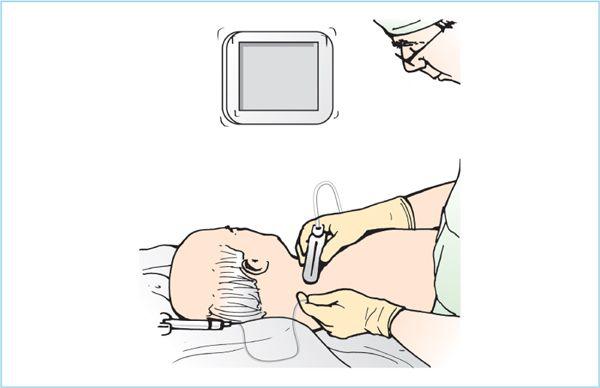
1. US-guided interscalene block. With US, real-time imaging of the needle may allow a more effective and efficient method to place the needle tip in close proximity to brachial plexus within the interscalene space. Additionally, US allows for real-time observation of LA distribution around the brachial plexus and can potentially guide more purposeful needle tip redirections if necessary (8).
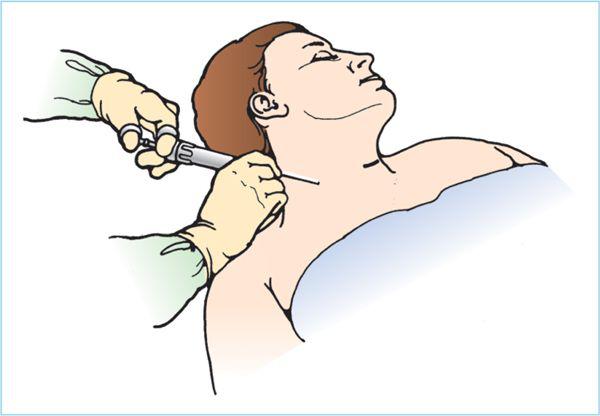
a. The patient is positioned supine, with the head turned slightly to the side opposite the surgical site. A small folded towel is placed under the head, and the ipsilateral hand is held at the side and extended toward the feet.
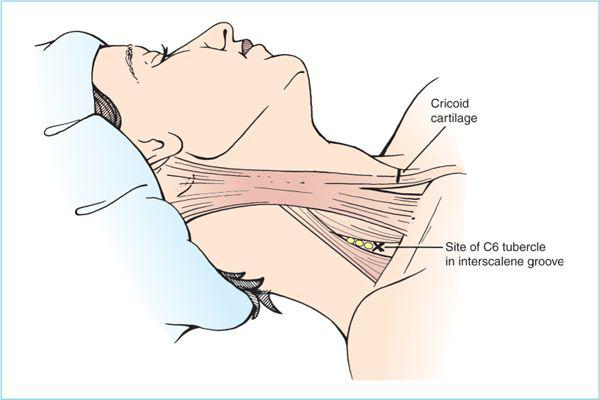
b. The surface anatomy is identified and marked—the cricoid cartilage, the lateral border of the sternocleidomastoid (SCM) muscle, and the interscalene groove. The latter can be located by asking the patient to raise the head slightly into a “sniffing” position. Two fingers placed along the tense lateral border of the SCM and rolled posterior will drop onto the AS muscle. The scalene muscles lie more posterior than lateral to the SCM and may be harder to appreciate in the heavier patient. The groove between the scalenes can be palpated by gently rolling these fingers further posterior (Figure 12.4).
c. After sterile skin preparation and draping, the US probe is prepared. US gel is placed on the transducer and then sterile sleeve is placed over the US probe. A small amount of sterile US gel is then applied either to the probe or the skin. The probe is placed perpendicular to the interscalene grove to produce a transverse (short-axis) view of the nerves (Figure 12.5). The US probe is swept back and forth until the nerves and nearby blood vessels are identified. If the anatomy is ambiguous, it is easy to start with a view of the supraclavicular area where the rib and artery provide easily identified landmarks, with the brachial plexus typically located superior and posterior to the pulsatile and hypoechoic SA. Another alternative is to look more cephalad for the bony prominences of the transverse processes, with the nerve roots emerging between them. Nerves visualized in these areas can then be followed to the midcervical level by rotating and moving the probe to keep the nerves in the center of the field in a transverse view.
Figure 12.4. Superficial landmarks for interscalene brachial plexus block. The sternocleidomastoid muscle is identified, and the anterior scalene muscle found by moving the fingertips over the lateral border of the larger muscle while it is slightly tensed. The groove between the anterior and middle scalene muscle can usually be felt easily, along with the tubercle of the sixth cervical vertebra, which lies at the level of the cricoid cartilage.
Figure 12.5. Positioning of patient for interscalene ultrasonographic block. The patient is supine, but rolled slightly anterior by placing a blanket or pillow behind the shoulder. When the optimal level of probe placement for nerve visualization is identified, a skin wheal is placed on the posterior edge of the transducer.
d. Out-of-plane approach. The needle is introduced through a skin wheal at the superior central side of the transducer and advanced, using real-time imaging, in an out-of-plane insertion into the interscalene groove. The anticipated needle path is now in a caudad direction, but the risk if pneumothorax should be minimized if the needle tip is identified at all times.
e. When the needle appears to lie next to the nerves, a 1- to 2-mL injection should confirm spread of the anesthetic around the nerves. The needle is repositioned and incremental injection is performed until the nerve bundle is surrounded with LA.
f. Nerve-stimulating needles may be used, and stimulation may be confirmatory, but not necessary.
g. If an in-plane insertion is desired, an approach from the posterior side (through the MS) may be more desirable (to reduce the chance of phrenic nerve injury). If this approach is planned, a towel or blanket should be placed under the ipsilateral shoulder blade to rotate the patient forward and allow more room for needle placement (Figure 12.5). Alternatively, the patient can be turned to the lateral position if sufficient pillows are provided to ensure stability.
h. A 50-mm (2-in.) 20- to 22-gauge needle with sterile connection tubing is advanced while injecting 0.5 to 1.0 mL increments of LA to anesthetize the needle tract and optimize needle tip visualization. The needle should be visualized traversing through the levator scapulae and then through the posterior border of the MS muscle (Figure 12.6). As the needle approaches and pushes on the anterior fascia of the MS, the resistance provided by the fascia is seen and felt. Once the needle penetrates the anterior fascia of the MS, the needle tip is within the interscalene space, located on the posterior aspect of the nerve roots. At this point, 1 to 3 mL of LA is injected and the distribution of LA around the brachial plexus elements is observed in real time. After the initial injection, 3 to 5 mL of LA is injected incrementally observing for distension of the interscalene space and more complete LA distribution around the desired components of the brachial plexus.
2. Continuous interscalene blockade allows for prolonged postoperative analgesia for procedures such as total shoulder replacement or rotator cuff repair. There are a number of approaches described (9–11). The authors use an in-plane transverse-MS approach, which allows constant real-time guidance of the needle tip traversing through the posterior aspect of the MS muscle and the anterior fascial plane of the MS muscle located directly posterior to the brachial plexus roots
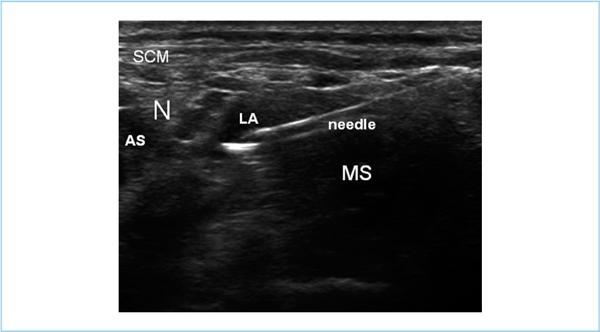
Figure 12.6. Ultrasonographic interscalene block, in-plane. The nerves are identified as hypoechoic circles (N) lying between the bodies of the anterior (AS) and middle scalene (MS) muscles, below the sternocleidomastoid (SCM). The needle is introduced from the posterior side through the body of the MS and local anesthetic solution (LA) injected to surround the roots/trunks at this level.
a. Position. The patient is placed supine and a small towel or bump may be placed under the ipsilateral shoulder blade to elevate the shoulder and neck off the bed to facilitate exposure of the posterior aspect of the neck, as in the single-injection in-plane approach.
b. A preliminary US view is obtained by placing the US probe just above the clavicle (in the supraclavicular fossa) initially in a coronal plane to the patient. The US probe is then manipulated (rocked back and forth) in a coronal oblique plane to obtain a short-axis view of the SA lying on top of the first rib. Keeping the brachial plexus in the middle of the screen, the US probe is slowly slid superior along the interscalene space until the brachial plexus appears in the form of the hypoechoic roots sandwiched in between the AS and MS muscles. At this point, the probe is typically in an oblique-axial plane to the patient’s neck. Finer manipulations of the probe (rotation and tilting/angulation) are performed until an optimal view is obtained. At this point, a footprint of the final probe on the skin surface should be drawn to minimize rescanning after sterile skin preparation and draping have been performed.
c. After sterile skin preparation and draping, the transducer is repositioned over the previously drawn footprint and the US view of the brachial plexus is then reacquired. At this point, a small skin wheal of LA is placed 1 cm lateral to the probe (typically over the levator scapulae or the posterior scalene). A 38-mm (1.5-in.) 22-gauge needle with a 3-mL syringe attached is advanced through the skin and into the MS muscle in a posterior to anterior direction toward the brachial plexus with real-time US observation of the entire needle. This allows for anesthesia of the deeper tissues, as well as observation of the correct needle trajectory toward the brachial plexus.
d. A 17-gauge Tuohy needle (with the bevel pointed laterally) is introduced along the same track with US guidance (real-time imaging). This approach has the needle advanced through the MS muscle and avoids the more superficial cervical fascial layers that often make advancement of a blunt Tuohy needle more challenging. When the needle tip is in the interscalene groove, a 5 to 10 mL of LA solution is injected to “open up” the space and allow easier passage of the catheter (Figure 12.7). This spread of LA is visualized with the US probe. Before the block, preparation can include placing the catheter into the needle to the level of the orifice and attaching the syringe of LA to the catheter; this preblock preparation may be helpful to the practitioner placing the block without extra hands available.
e. Once the initial bolus of LA has been injected, the catheter is threaded approximately 1 to 3 cm (1 in.) and the placement of tip is confirmed by US with the injection of an additional 5 mL of LA solution to confirm that the injection remains within the interscalene space.
f. When securing the catheter to the skin, tunneling is not necessary with this approach in most patients. A single clear adhesive dressing (Tagaderm) is usually sufficient. For shoulder surgery, the catheter can be taped posteriorly around the back of the neck to avoid the surgical field.
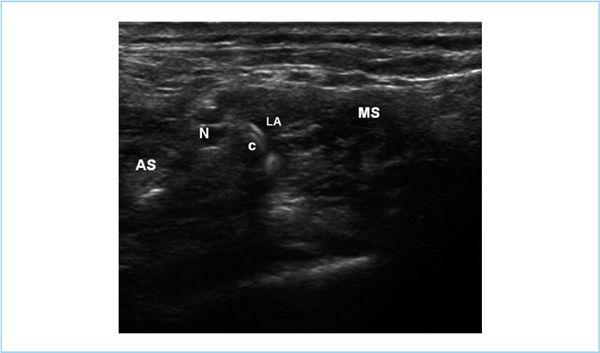
Figure 12.7. Placement of continuous catheter by ultrasonography of interscalene block. The approach is similar to the single injection technique (Figure 12.6), but a larger Tuohy needle is used with a catheter in place as it is advanced. When injection of a small amount of local anesthetic (LA) indicates location of the needle tip in the interscalene groove between the anterior scalene (AS) and middle scalene (MS) near the nerves (N), the catheter (C) is advanced 1 to 2 cm beyond the needle tip.
3. Paresthesia or peripheral nerve stimulator approach
a. The patient is positioned supine, as for the single-injection US approach.
b. The surface anatomy is identified and marked as above, but the exact location is more critical for locating the nerves. In addition to the scalene groove, the tubercle of the transverse process of the sixth vertebral body (Chassaignac tubercle) should be identified in the base of this groove at the level of the cricoid cartilage, which is commonly also the level at which the external jugular vein crosses the posterior border of the SCM. In virtually all patients, the tubercle can be identified directly, and is a more reliable landmark to identify the location of the nerves. This is not uncomfortable for the patient if done gently. The location of the tubercle should also be marked with an X (Figure 12.4).
c. After aseptic skin preparation and draping, a skin wheal of LA is raised in the interscalene groove at the level of the “X.” A 38-mm (1.5-in.) 22-gauge needle is inserted in a caudad and posterior direction, angling toward the tubercle. This requires that the needle be perpendicular to the skin in all planes. A caudal angulation of at least 50 degrees will reduce the potential for spinal canal entry (12). The hub of the needle is held between the thumb and forefinger of the dominant hand, the heel of which rests solidly on the clavicle or neck (Figure 12.8). This fixation of the needle reduces the chance of accidental movement of the needle when a peripheral nerve stimulator evoked motor response or paresthesia is encountered.
Figure 12.8. Hand position for interscalene block. The needle is introduced into the skin over the interscalene groove at the level of the cricoid cartilage (or the sixth vertebral tubercle, if palpable). It is then directed in a caudad and posterior direction into the interscalene groove with one hand resting on the clavicle exerts constant control of the depth of insertion.
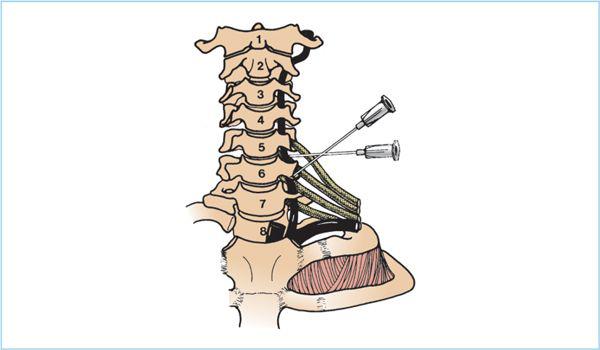
d. The needle is advanced until a stimulator response or paresthesia is obtained or the bone is contacted. If the tubercle is reached before identifying the nerve, the needle is withdrawn almost to the skin and redirected. The path of search for the nerve is in 1-mm steps along a line perpendicular to the presumed course of the nerve (i.e., anterior to posterior); the needle tip should never be directed cephalad or medially. This would allow entry into the intervertebral foramen, with the possibility of puncture of the vertebral artery or dura itself. A more caudad direction will increase the potential for pneumothorax (Figure 12.9).
e. On obtaining a stimulation or paresthesia in the arm (usually thumb or forearm), gentle aspiration is performed, followed by injection of a 1 mL “test dose.” If no cramping or discomfort is produced with this test, a 30 to 40 mL of anesthetic solution is injected incrementally. The needle is held in position with the dominant hand, whereas the 10-mL syringe is detached and refilled. Alternatively, a single 50-mL syringe or a stopcock with an additional 20-mL syringe of LA solution is connected to the needle by a short length of intravenous extension tubing. Aspiration is performed after each 3- to 5-mL injection, and the patient is observed carefully for signs of intravascular injection.
Figure 12.9. Needle direction for interscalene block. The needle is kept in a 45-degree caudad direction; a more caudad direction will contact the pleura, although a medial insertion will allow the point to pass into the intervertebral foramen and produce epidural, spinal, or intra-arterial injection of anesthetic. Note the relation of the vertebral artery and the nerve roots to the transverse processes.
f. A Horner syndrome occasionally may develop, as well as ipsilateral phrenic nerve paralysis (which occurs in 100% of patients with this block) (13) as the solution spreads anterior to the scalene muscles or cephalad in the interscalene groove to the cervical roots (see Section IV).
B. Supraclavicular block. This approach relies on the predictable anatomy of the three major trunks of the plexus as they cross over the first rib between the insertion of the AS and MS muscles just posterior to the SA. This intersection of nerves with rib occurs behind the midpoint of the clavicle and lies relatively superficially (Figure 12.10). This block provides the best anesthesia of the arm with a single injection, but has been avoided by some because of the risk of pneumothorax. US guidance simplifies the block, and may reduce this risk.
1. US guidance for the supraclavicular block has generated a renewed interest in this approach because the pleura can be directly visualized and, therefore, avoided (14,15) (Figure 12.11). Theoretically, this should significantly decrease the risk of pneumothorax (assuming the needle’s approach is visualized with real-time imaging) because not only can the brachial plexus and SA be visualized but also the first rib and the underlying pleura may be directly visualized in real time.
a. The patient is placed in the supine position, with the ipsilateral arm held along the side and extended caudally (as if reaching for the knee) so as to facilitate palpation of the clavicle and scalene muscles.
b. The probe is placed directly behind the midpoint of the clavicle in a coronal oblique plane and angled to obtain a short-axis view of the SA lying on the first rib (Figure 12.10). At this point, the brachial plexus is superior and posterior to the pulsatile SA. The brachial plexus may often appear as a cluster of grapes at this level and may either be the trunks or divisions of the brachial plexus.
Figure 12.10. Pertinent anatomy of supraclavicular block. The trunks/divisions cross the rib just posterior to the subclavian artery, and can be visualized easily with an ultrasonographic probe placed just behind the clavicle.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree