
Blunt Chest Trauma
Richard L. Byyny
Blunt chest trauma (BCT) is a common emergency department (ED) presentation. The trauma can range from the most minor chest wall contusion to catastrophic and fatal intrathoracic injury. BCT is involved in nearly one-third of admissions to trauma centers and accounts for about 25% of all trauma-related deaths in the United States (1). Most of these injuries are the result of motor vehicle collisions or pedestrians who are stuck by automobiles. Unlike penetrating injuries, BCT usually occurs when a large force is applied to a relatively larger area. Injury kinetics include acceleration and deceleration forces as well as transmission of blunt force to internal structures. BCT is often associated with multiple system trauma; including injury to the abdomen, head, spine, and extremities. Therefore, BCT must be evaluated in the context of these other injuries and, at times, more imminent life threats.
CLINICAL PRESENTATION
Chest Wall Injuries
Chest wall contusions and rib fractures account for the majority of blunt chest wall trauma (2). Rib fractures make breathing painful and can increase the patient’s morbidity and mortality by adversely affecting ventilation. Fractures typically occur at the site of the impact or the posterior angle where the rib is structurally the weakest. Fractures are more common in adults than children because of the relative inelasticity of the mature thorax. In fact the presence of rib fracture in children should raise the suspicion of child abuse and heighten the concern for coexisting intrathoracic injury (3). Elderly patients have a higher morbidity and mortality associated with rib fractures than younger patients with each additional fracture increasing the risk of death by 19% and increasing the risk of developing pneumonia by 27% (3). Although the fourth through the ninth ribs are most commonly involved, there is a fourfold increase in splenic injuries with left-sided rib fractures 9 to 11 and a threefold increase risk of liver injuries in right-sided rib fracture 9 to 11 (4). Multiple rib fractures or the presence of a flail chest wall segment may be associated with intrathoracic injury, usually a pulmonary contusion.
Clinical findings typically include pleuritic pain, tachypnea, splinting, and point tenderness intensified by deep breathing or coughing. Bony crepitus may be palpable. Anteroposterior compression of the thorax produces referred pain to the fracture site; if fracture is absent, there should not be referred pain to the localized area of tenderness.
Sternal Fractures
Sternal fractures usually result from high-energy forces to the midanterior chest wall. This force most commonly occurs from motor vehicle collisions in which the chest strikes the steering wheel, dashboard, or shoulder belt at high velocity. This force may result in a sternal fracture or costochondral separation and, in rare instances, an anterior flail chest when the sternum is disarticulated from the ribs. Patient may have point tenderness on their sternum, hematoma, or deformity.
Flail Chest
Flail chest occurs when three or more ribs are fractured in two or more places. In a patient who is breathing spontaneously, the negative intrathoracic pressure with inspiratory effort results in a paradoxical movement of the chest wall (the flail segment moves in during inspiration and out during expiration). There is usually no significant ventilatory compromise caused by the flail segment per se. In these patients, respiratory compromise is related to the degree of pulmonary contusion, which almost inevitably occurs when force is significant enough to cause a flail chest. However, in patients with large flail segments, the normal thoracic physiology is disrupted, causing respiratory failure requiring mechanical ventilation. All patients experience significant pain secondary to the respiratory movement of multiple rib fracture fragments and will often have tenderness, crepitus, and paradoxical movement of the chest wall. In some patients who are splinting or in those on positive-pressure ventilation, the flail segment may not be readily apparent. Palpation of the chest can help detect the injury. It is notable that in patients with flail segments the morbidity and mortality are increased when compared to patients with a similar numbers of fractures without a flail segment (5).
Pulmonary and Pleural Injuries
Blunt trauma may result in pneumothorax, hemothorax, or hemopneumothorax, usually secondary to a rib fracture penetrating the visceral pleura and lung parenchyma. Hemothorax usually results from disruption of an intercostal artery (see Chapter 32).
Pulmonary Contusion
The most common injury to the pulmonary parenchyma in BCT is pulmonary contusion. Among severely injured (ISS >15) blunt trauma patients approximately 27% had pulmonary contusion (6) and in children pulmonary contusion represents a large proportion of thoracic injuries (7). This injury results from transthoracic transmission of kinetic injury to the pulmonary parenchyma causing an alveolar–capillary membrane disruption and subsequent pulmonary edema. This injury results in areas of the lung that are perfused but not ventilated (i.e., a ventilation perfusion mismatch), resulting in hypoxia, hypercarbia, and acidosis.
Depending upon the extent, this injury results in minimal to life-threatening symptoms. A patient with a pulmonary contusion usually presents with dyspnea and tachypnea. There may be tenderness or obvious ecchymosis and deformity over the injured chest wall. Large pulmonary contusions are associated with tachycardia, hypotension, cyanosis, and low oxygen saturation. Patients with multiple rib fractures or flail segments of the chest wall are more likely to have associated pulmonary contusion.
Tracheal and Bronchial Injuries
Tracheal and bronchial injuries are rare accounting for only between 0.1% and 2% of patients who present to the ED (8). The majority of these injuries occur within 2 cm of the carina or at the origin of the lobar bronchi (9). Symptoms are usually related to the size of the defect in the airways and whether there is communication with the pleural space. Occasionally minimal symptoms may occur, even with severe tracheal or bronchial injury. Hemoptysis may occur in up to 25% of cases and subcutaneous emphysema or pneumomediastinum is present in 35% to 85% of cases (8). Patients can also present with dyspnea, hoarseness, or aphonia. This injury should be considered if there is a persistent air leak from a properly positioned chest tube and difficulty in fully reexpanding the lung.
Blunt Cardiac Injuries
By virtue of its location in the chest, the heart is susceptible to injury from compression of the chest wall and upper abdomen and from deceleration forces. It is the cause of death in up to 20% of automobile collisions. There is no gold standard to make the diagnosis of blunt cardiac injury; therefore, the true incidence is unknown and evaluating literature on the topic is difficult with different authors using different diagnostic standards. Therefore, there is a wide range of reported incidence from 20% to 76% of blunt thoracic trauma patients.
The right ventricle is the most commonly injured portion of the heart because of its relatively vulnerable position immediately behind the sternum; however, injuries to multiple chambers occur in 50% of cases (10). Blunt cardiac injury encompasses a spectrum of injuries including myocardial concussion, myocardial contusion, myocardial infarction, and myocardial rupture.
Myocardial concussion (commotio cordis) is a ventricular dysrhythmia or asystole secondary to a direct blow to the myocardium without pathologic evidence of cardiac injury. Myocardial concussion is the most common cause of sudden death in young athletes (11). Those patients who survive a myocardial concussion usually have little or no long-term sequelae from their blunt cardiac injury.
Myocardial contusion is characterized by localized edema and hemorrhage into cardiac muscle. This trauma may involve segments of the cardiac conduction system, most commonly the right bundle branches.
Traumatic myocardial infarction is rare but can occur from disruption of the coronary artery intima and subsequent thrombosis. The most severe form of blunt cardiac injury is cardiac rupture, which is a rare injury. These patients will present with hypotension or in extremis and usually have a right atrial or ventricular injury.
Physical findings in blunt cardiac injury may be nonspecific. Chest pain from either chest wall trauma or ischemia may be present. Seventy percent to 80% of patients with blunt cardiac injury have external signs of chest trauma including contusions, abrasions, palpable crepitus, and flail segments. The presence of a fractured sternum, once thought to be a marker for blunt cardiac injury, has not been shown to reliably correlate with the presence of a blunt cardiac injury (12). The most common vital sign abnormality is persistent sinus tachycardia after other causes have been treated. Hypotension is a serious sign and should raise the possibility of pericardial tamponade, myocardial rupture, or rupture of an internal cardiac structure such as a chordae tendineae or valve.
Great Vessel Injuries
Blunt aortic injury accounts for approximately 8,000 deaths per year in the United States, and up to 15% of automobile fatalities are caused by traumatic disruption of the aorta (13). Eighty percent of patients with aortic injuries die in the field. The tear of the aorta is usually a circumferential transverse laceration that disrupts the physical integrity of the intima and muscularis layers of the aorta. If the tear is complete, involving all three layers, this results in death caused by immediate exsanguination. In survivors, the adventitia remains intact, and blood is contained by a false aneurysm formed by the adventitia and surrounding mediastinal structures. If this injury is unrecognized, there is a significant risk of a free rupture and sudden death in the hours to days following this injury.
Disruption of the great vessels usually results from high-speed motor vehicle collisions, falls from a height, or ejection from motorcycles or other vehicles (13). The classic mechanism is a head-on motor vehicle collision, although the injury can occur after side or rear impacts. In seat-belted motor vehicle victims, descending thoracic tears are more common. Ascending aortic disruption is seen more often in unrestrained drivers or those who are ejected or fall from a height and experience vertical deceleration forces (14). Most often, these injuries involve the aorta but can involve the brachiocephalic artery and inferior vena cava. Patients with rupture of the vena cava have a poorer outcome because of continued, ongoing, significant blood loss and difficulty in controlling the bleeding and repairing the defect at surgery.
Several mechanisms have been postulated to explain aortic injuries. First, rapid horizontal deceleration produces shearing forces at the aortic isthmus just distal to the origin of the left subclavian artery. Ninety percent of traumatic aortic tears originate at this site. Anatomically, this frequency can be explained by the fact that the descending aorta is tethered by the ligamentum arteriosum and the intercostal arteries. The ascending aorta is relatively mobile and, during deceleration, continues to move forward while the descending aorta is held in place, resulting in shearing forces that cause a rent in the aorta (eFig. 31.1). The second proposed mechanism is that of the “water hammer” effect where a propagated wave of blood causes a surge in intraluminal pressure. Although the aorta may withstand intraluminal pressures of up to 350 mm Hg, this pressure may be surpassed leading to aortic injury (15). The final, and most likely, proposed mechanism is the “osseous pinch” model in which the aorta is pinched between the sternum and the vertebral column, resulting in shearing forces that cause injury to the aorta (16).
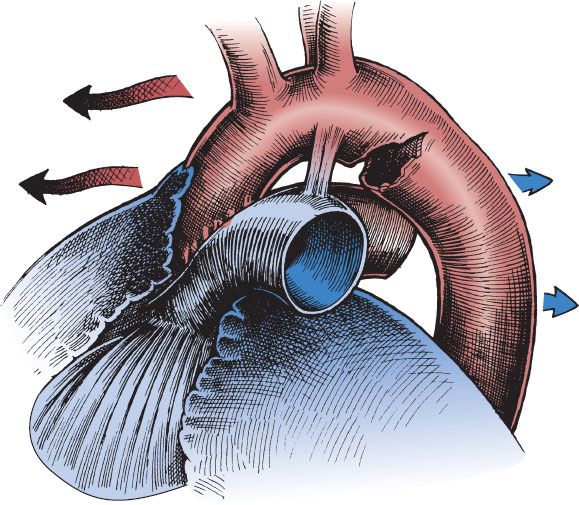
eFIGURE 31.1 Rapid deceleration injury causing a tear in the thoracic aorta. The ascending (anterior) aorta tends to continue moving forward, while the more fixed descending aorta is held stationary. The rupture occurs just distal to the ligamentum arteriosum at the level of the isthmus.
The symptoms and signs of traumatic great vessel disruption are often absent or missed because of coexisting, significant injuries to the head, spine, abdomen, pelvis, and extremities. The most frequently recorded complaints are chest pain, dyspnea, and back pain. However, it is of note that only 25% of patients present with retrosternal pain or pain radiating to the upper back which is considered typical of nontraumatic aortic dissection. Other symptoms include dysphagia, hoarseness, and ischemic pain of the extremities. Physical examination may reveal ecchymosis, abrasion, or tenderness of the anterior chest wall consistent with the impact of this area on a steering wheel. Thirty-one percent of patients with an aortic disruption present with the pseudocoarctation syndrome. In these cases, upper-extremity hypertension is present with decreased or absent femoral pulses because of compression of the aortic lumen by surrounding periaortic hematoma. Reflex stretching of the cardiac sympathetic fibers at the aortic isthmus may account for the observation that 72% of patients with aortic rupture manifest a relative hypertension (average blood pressure 152/98 mm Hg) (17). A harsh systolic murmur over the precordium or interscapular area (thought to be because of turbulent flow across the area of transection) has been reported to be present in 26% of cases (18). Unfortunately, the presence of great vessel injury cannot be confirmed or ruled out based on physical examination or history.
In confirmed cases of traumatic aortic injury, one-third to one-half of the patients have no external evidence of chest injury on initial presentation to the ED. Therefore, this injury should be suspected, even in the absence of these signs or symptoms, whenever there has been major acceleration–deceleration forces involving the chest (i.e., significant ejection mechanisms, falls from heights >10 ft, and motor vehicle collisions with speeds >30 mph, and a lack of proper vehicle restraints).
Diaphragmatic Injuries
Blunt traumatic diaphragmatic injury results from violent compression of the lower chest and upper abdomen and has an incidence between 0.5% and 8% of blunt trauma victims (15). Sixty percent to 90% of traumatic rupture of the diaphragm from blunt trauma occurs on the left side (19). Blunt trauma typically produces diaphragmatic defects of >10 cm on average and has a higher mortality rate than penetrating injury to the diaphragm because of the higher incidence of serious associated injuries to abdominal and chest structures.
Signs and symptoms of diaphragmatic rupture are highly variable depending upon the size of the defect, the mechanism, the abdominal viscus that herniates through the defect, and the degree of cardiopulmonary compromise. Common symptoms include cough, dyspnea, nonspecific chest or abdominal pain radiating to the shoulder, and the perception of peristalsis in the chest. Signs include an immobile left hemithorax, decreased breath sounds, and tympany or borborygmi in the left chest. Significant herniation of abdominal viscera into the thoracic cavity usually results in severe respiratory distress and may be clinically confused with a tension pneumothorax. A tension viscerothorax (gastrothorax) occurs when the resulting increase in intrapleural pressure causes shift of the mediastinum and hemodynamic collapse. Therefore, great care should be taken when performing a thoracostomy to verify a free pleural space before inserting the chest tube.
Esophageal Injuries
Esophageal injuries secondary to blunt trauma are rare occurrences yet critical to diagnose secondary to the high morbidity and mortality when treatment is delayed. They have been reported from sharp blows or when force is applied to the upper abdomen in which air and gastric contents are violently forced into the esophagus causing a perforation in the distal esophagus similar to those that results from retching and vomiting (i.e., Boerhaave syndrome). Injuries to the esophagus can also occur with compression of the esophagus against the spine, producing longitudinal tears in the upper thoracic esophagus and can be associated with laceration in the membranous (i.e., posterior) portion of the trachea, resulting in traumatic tracheoesophageal fistulas. Injuries to the esophagus can also occur from barotrauma, because the esophagus is a hollow, air-containing organ. An example of this is forceful insufflation of the esophagus from inhalation of aerosol cans, air compressors, or inflation devices or in children from the biting of inner tubes, and eruption of bottled carbonated beverages into the esophagus. Perforations of the esophagus can result from alkali ingestion, button batteries, foreign bodies, and iatrogenic misplaced tubes or endoscopes.
Signs and symptoms of esophageal injury are subcutaneous emphysema (especially in the neck or supraclavicular fossa), unexplained tachycardia, dyspnea, dysphagia, odynophagia, cyanosis, pneumomediastinum, pneumothorax, pleural effusion (particularly on the left), and hematemesis.
Traumatic Asphyxia
Traumatic asphyxia occurs when the thorax is squeezed between two objects for a prolonged period of time. This results in compression of the vena cava with resultant prolonged increased venous pressure to the neck and head. This prolonged squeeze and compromised venous return results in intense cyanosis of the upper chest, neck, and face as well as petechiae and subconjunctional hemorrhage. Some patients may have retinal hemorrhage and loss of consciousness because of cerebral hypoxia. Sometimes there are associated chest wall and pulmonary parenchymal injuries such as pulmonary contusion and hemopneumothorax.
DIFFERENTIAL DIAGNOSIS
The differential diagnosis of chest wall injuries includes rib fractures, flail chest, sternal fracture, costochondral separation, and chest wall contusion.
After blunt trauma, the differential diagnosis for pulmonary and pleural injuries includes pulmonary contusion, pneumothorax, hemothorax, hemopneumothorax, pulmonary contusion, tension pneumothorax, and acute pericardial tamponade. Tension pneumothorax must be differentiated from acute pericardial tamponade because both cause tachycardia, hypotension, and an elevated central venous pressure (CVP). In patients with tension pneumothorax breath sounds are absent or markedly diminished and pericardial ultrasound is normal.
The differential diagnosis of tracheal and bronchial injuries includes other traumatic causes of pneumomediastinum, such as a ruptured esophagus or an iatrogenic perforation of the esophagus, posterior pharynx, or pyriform sinus during attempts at endotracheal intubation.
In patients with blunt cardiac injury, rupture of the valves or chordae tendineae may result in acute cardiac failure. In rare instances, blunt cardiac injury may cause acute pericardial tamponade. This injury can be differentiated from tension pneumothorax by the presence of a pericardial effusion on ultrasound, as well as by bilaterally equal breath sounds on physical examination.
The majority of patients who suffer from blunt thoracic aortic injury have coexisting serious injuries. These include fractures of the sternum and ribs, hemothorax, pneumothorax, hemopneumothorax, tracheobronchial disruption, diaphragmatic rupture, esophageal perforation, acute pericardial tamponade, and blunt trauma to the myocardium.
Traumatic rupture of the diaphragm can be confused with a pneumothorax or a tension pneumothorax when abdominal viscera have herniated into the thoracic cavity resulting in respiratory distress and diminished or absent breath sounds, usually on the left side.
ED EVALUATION
Chest Wall Injuries
After a history and physical examination including pulse oximetry, chest wall trauma can be evaluated with chest radiography. However, chest radiographs may not be necessary in isolated, localized chest wall trauma when there are no physical findings and no respiratory distress manifested by tachypnea or decreased oxygen saturations. Up to 50% of rib fractures are missed on the initial chest radiographs; 10% do not visualize radiographically for 1 to 2 weeks after the injury regardless of the views taken. Specific rib views are unnecessary and much of the time the presumptive diagnosis can be made without radiography. A chest radiograph is valuable when looking for complications of rib fractures such as hemothorax, pneumothorax, pulmonary contusion, atelectasis, and pneumonia. Because elderly patients have a greater morbidity and mortality from complications of rib fractures, there should be a lower threshold for evaluating these patients with a chest x-ray and rib films (15).
Consideration should be given to observation, performance of the focused assessment with sonography in trauma (FAST) examination, or abdominal computed tomography (CT) in the presence of 9th through 11th rib fractures given the heightened risk for spleen or liver injury. Pain referred to either shoulder may indicate the presence of either hemothorax or pneumothorax or subdiaphragmatic hemorrhage from injury to the spleen or liver. Patients who present several days after their initial trauma with increasing pain, dyspnea, or fever following chest wall trauma should have a chest x-ray to ascertain if there are any late complications such as atelectasis or pneumonia.
Flail Chest
Patients with evidence of a flail chest on physical examination should be evaluated with oxygen saturation monitoring and a radiograph of the chest to detect the presence of underlying pulmonary contusion, pneumothorax, or hemothorax. Parenteral analgesics or regional nerve blocks are necessary for adequate analgesia.
Pulmonary and Pleural Injuries
Clinical signs of tension pneumothorax or massive hemothorax (decreased breath sounds or subcutaneous emphysema in association with hypotension, tachycardia, and respiratory distress) mandate initial placement of a needle or tube thoracostomy prior to obtaining chest radiography. Tension pneumothorax should be a clinical diagnosis and should not be captured on a chest x-ray. The extended focused abdominal ultrasound in trauma (E-FAST) has been more widely utilized to assist in the diagnosis of pneumothorax. In addition to usual components of the FAST examination (evaluation of the right upper quadrant, left upper quadrant, pericardium, and retrovesicular space) the E-FAST also includes ultrasonography of the pleural surface using the high-frequency linear probe. It has been shown to have superior sensitivity to the supine chest x-ray and can expedite the diagnosis of pneumothorax (20). If the patient is hemodynamically stable, a portable chest radiograph is the initial study of choice; this will demonstrate hemothorax, pneumothorax, and pneumomediastinum.
Pulmonary Contusion
Radiographic evidence of pulmonary contusion may not be evident initially on the chest x-ray because these injuries tend to get worse over the ensuing hours following injury with the peak not being present until 72 hours after injury (6). Radiographic findings usually lag behind the clinical findings. A contrast-enhanced helical CT scan of the chest will detect the presence of pulmonary contusions before they become visible on standard chest radiographs. CT scans may be used to measure the extent of the pulmonary contusion and to determine the prognosis (6). All patients should be placed on oxygen and have continuous oxygen saturation monitoring. If the oxygen saturation is low, an arterial blood gas can be obtained to calculate an alveolar–arterial gradient and followed serially to determine subsequent therapy.
Tracheal and Bronchial Injuries
These injuries should be suspected when there is a persistent air leak despite the proper placement of a tube thoracostomy on the involved side. All patients should have a chest x-ray to rule out associated pneumothorax and to confirm that all the holes on the chest tube are within the thoracic cavity. Consideration should also be given to diagnostic studies that rule out the presence of an esophageal disruption (discussed later in this chapter). Surgical consultation should be obtained so that bronchoscopy can be performed for definitive diagnosis.
Blunt Cardiac Injuries
All patients in whom this injury is suspected should have cardiac rhythm and oxygen saturation continuously monitored. An electrocardiogram (ECG) should be obtained to ascertain the presence of any dysrhythmia, bundle-branch block, or new changes on the ECG (15). An initial ED ultrasound of the pericardium to detect the presence of pericardial effusion and to determine, if possible, the quality of cardiac wall motion should be performed. New murmurs or acute congestive failure after chest trauma should raise the suspicion of a ruptured interventricular septum, valve leaflet, or chordae tendineae. Traumatic ventricular septal rupture presents with a pansystolic murmur heard throughout the entire precordium, especially at the left sternal border. This murmur may not be appreciated until the patient has been resuscitated to a euvolemic state. In patients exhibiting hemodynamic instability and clinical signs of cardiac failure, a formal echocardiogram should be obtained to look for the presence of pericardial tamponade, valvular or chordae tendineae disruption, and to determine cardiac output.
Chest radiographs are not helpful in diagnosing cardiac trauma per se but may be helpful in identifying other thoracic injuries. Although nondiagnostic, multiple ECG abnormalities have been described that range from persistent sinus tachycardia to ST- and T-wave changes and bundle-branch blocks (the most common being right bundle-branch block). If ECG abnormalities are present, the patient should be admitted for 24 to 48 hours of continuous cardiac monitoring. The presence of a normal ECG confers a negative predictive value of 95% in ruling out myocardial contusion (12). Troponin I is helpful in making the diagnosis and in the stratification of those at risk for life-threatening conditions. If the troponin is not elevated at 4 to 6 hours post injury and the ECG is normal, the patient may be discharged from the ED conferring a negative predictive value of 100% (12). Neither nuclear testing nor echocardiogram is useful in diagnosing myocardial contusion.
Great Vessel Injuries
In patients with a major traumatic mechanism, a chest x-ray is a helpful screening tool in detecting not only great vessel injuries but also other associated thoracic abnormalities. There are multiple radiographic features of great vessel injury (Fig. 31.1). The most sensitive finding in patients with aortic injury is a wide mediastinum (>6 cm upright and >8 cm supine anteroposterior view) (13). However, only 10% of patients with a wide mediastinum will end up having an aortic injury; other causes include sternal, rib, or spine fractures, and the supine radiography. Sitting the patient up after the cervical spine has been cleared will decrease the incidence of a wide mediastinum. Despite the many radiographic signs of traumatic aortic injury that have been described, in 7% to 28% of cases of aortic injury the chest radiograph is normal (eTable 31.1) (14). Therefore, it is prudent to consider further diagnostic studies, if there is a significant mechanism, even in the presence of a completely normal upright chest x-ray (13,21).
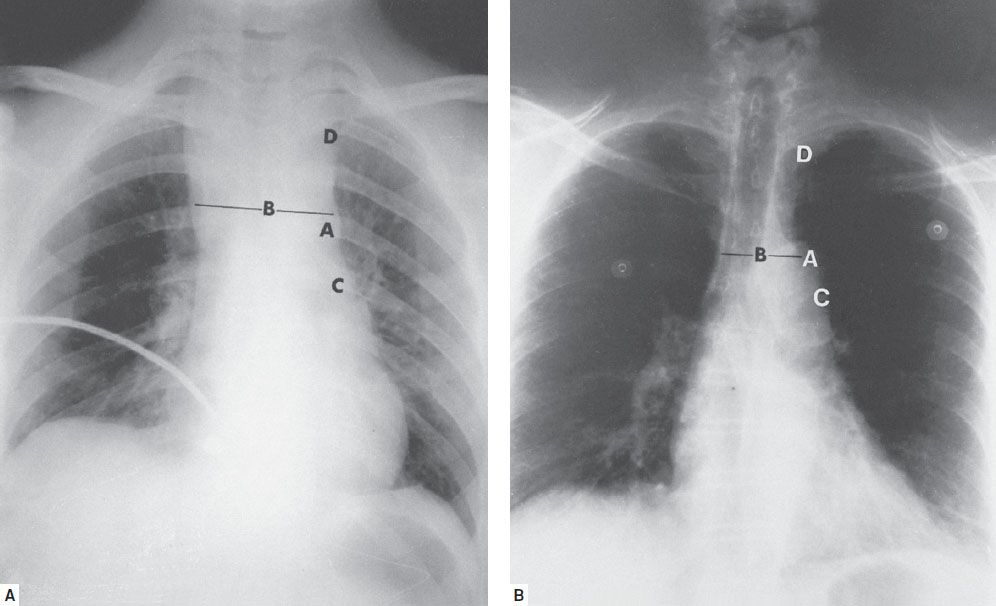
FIGURE 31.1 Upright posteroanterior chest radiographs of a 20-year-old man involved as a driver in a head-on motor vehicle collision (A) compared with that of a normal person (B). The first radiograph has several abnormalities suggestive of a great vessel disruption. A: Loss of detail of aortic knob with blurring of the aortic outline. B: Widened mediastinum (mediastinal width to chest width ratio >0.28). C: Opacification of the clear space between the aorta and pulmonary artery (aortopulmonary window). D: Obliteration of the medial aspect of the left upper field. The aortogram revealed rupture of the aortic arch. (Radiographs courtesy of the Department of Radiology, St. Luke’s Hospital, Milwaukee, WI.)









