CHAPTER 31 BLUNT CEREBROVASCULAR INJURIES
Over the past decade, a wealth of studies has provided the scientific rationale to promote the early screening and treatment of blunt cerebrovascular injuries (BCVI). Initially, BCVI were thought to have unavoidable, devastating neurologic outcomes, but several reports suggested anticoagulation improves neurologic outcome in patients suffering ischemic neurologic events.1,2 If untreated, carotid artery injuries (CAIs) have a stroke rate up to 50% depending on injury grade, with increasing stroke rates correlating with increasing grades of injury; vertebral artery injuries (VAIs) have a stroke rate of 20%–25%.3 Screening protocols, based on patient injury patterns and mechanism of injury, have been instituted to identify these injuries in asymptomatic patients and to initiate treatment, prior to neurologic sequelae. Current studies suggest early antithrombotic therapy in patients with BCVI reduces stroke rate and prevents neurologic morbidity.3–8
SIGNS AND SYMPTOMS
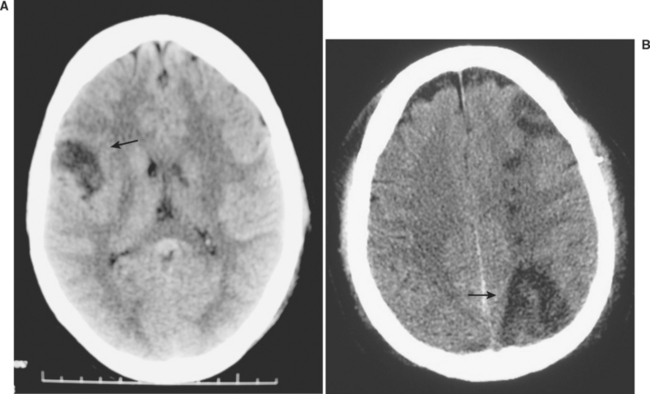
Blunt cerebrovascular injuries were first reported over 30 years ago, in patients who presented with stroke following injury.9 The patient’s symptom of cerebral ischemia or the distribution of their symptoms usually indicates the underlying cerebrovascular lesion (Figure 1). Carotid artery injuries generally result in contralateral sensorimotor deficits, which to the general practitioner is classically defined as a stroke. Aphasia occurs when the dominant hemisphere is involved, while nondominant hemisphere strokes may result in hemineglect. Vertebral artery injuries typically manifest as more vague symptomatology, namely ataxia, dizziness, vomiting, facial or body analgesia, or visual field defects. Symptoms of carotid-cavernous fistulae include orbital pain, exophthalmos, chemosis, and conjunctival hyperemia.
Although some patients may present with symptoms of BCVI-related ischemia within an hour of injury, the majority exhibit a latent period. This asymptomatic phase has been inferred based upon the time to onset of symptoms in patients with defined injuries who did not receive antithrombotic therapy. This timeframe appears to range from hours up to 14 years, but t he majority seems to develop symptoms within 10–72 hours.1,3,4,10 The goal, then, is diagnosing BCVI during this “silent period” prior to the onset stroke. After all, the theory is that if you diagnose these injuries during the asymptomatic period you can effectively treat the patient to prevent stroke. Screening for BCVI during the asymptomatic period was initially suggested in the mid-1990s after the recognition that specific patterns of injuries were associated with BCVI. Although optimal screening criteria have yet to be defined, current screening algorithms include patients considered at high risk based on their injury pattern.
MECHANISM AND PATTERNS OF INJURY
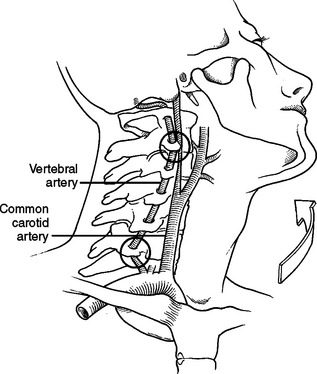
Crissey and Bernstein originally postulated three fundamental mechanisms of injury resulting in BCVI.9 The first is a direct blow to the neck. This mechanism is often seen with patients in motor vehicle collisions with inappropriately fitting seatbelts who end up with a seatbelt sign across the neck; it can also be seen in mountain bikers with a direct blow to the neck after falling during riding. The second proposed mechanism is hyperextension with contralateral rotation of the head. This is the most common mechanism causing CAI with the hyperextension resulting in a stretching of the carotid artery over the lateral articular processes of C1–C3 (Figure 2). VAI may also be due to a hyperextension-stretch injury due to the tethering of the vertebral artery within the lateral masses of the cervical spine. The third mechanism of injury is a direct laceration of the artery by adjacent fractures involving the sphenoid or petrous bones. Although originally described as the mechanism in association with CAI, this may also be the cause of VAI. With a fracture of any of the bony elements comprising the vertebral foramen, also termed the foramen transversarium, it is not surprising that the vertebral artery could be directly injured. Regardless of the type of injury mechanism, there is intimal disruption of the carotid or vertebral artery. This intimal tear becomes a nidus for platelet aggregation that may lead to emboli or vessel occlusion, and subsequent stroke.
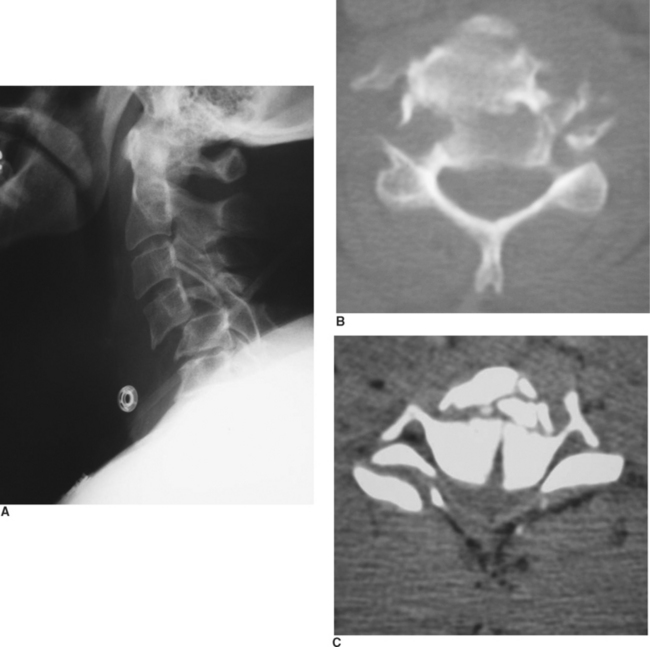
Although the mechanism of injury is important for determining patients at high risk for BCVI, the patient’s associated injuries are also critical to determine which asymptomatic patients undergo screening for BCVI. Aggressive screening for BCVI was initially suggested after recognition that specific patterns of injuries were associative. Current screening algorithms include patients with signs or symptoms, as well as those considered at high risk by injury pattern (Table 1). BCVI screening protocols have remained relatively unchanged over the past decade since their institution, aside from refinements in patients with cervical spine fractures. Initially, screening protocols included all patients with cervical spine fractures to rule out BCVI. However, there were a significant number of patients with isolated cervical spine fractures that could be managed by the local orthopedic surgeons without referral to Level I trauma facilities; therefore, we questioned the need to evaluate every patient with a cervical spine fracture.11 In our population, excluding patients who underwent screening for associated injuries or other injury patterns, only patients with three patterns of spine fracture were identified as having a BCVI, barring other symptoms of neurologic compromise: cervical spine subluxation, fractures involving the transverse foramen, and upper cervical spine fracture of C1–C3 (Figure 3). Therefore, only this subpopulation of patients with cervical spine fractures undergoes screening for BCVI.
Table 1 Denver Screening Criteria for Blunt Cerebrovascular Injuries
| Signs/Symptoms of BCVI |
| Risk Factors for BCVI |
BCVI, Blunt cerebrovascular injury; CT, computed tomography.
Courtesy of Denver Health Medical Center.
DIAGNOSTIC IMAGING
Using defined screening protocols, high-risk patients undergo imaging to identify BCVI. Historically, four-vessel arteriography has been the gold standard to diagnose BCVI. Undoubtedly, many clinicians question the need for subjecting patients to angiography. Angiography is labor intensive, costly, and not without risks; and, if not available at smaller hospitals, requires emergent transfer of a patient for definitive evaluation. Currently, CTA remains an unproven diagnostic modality for this injury. In particular, injuries that may be missed by such noninvasive studies are typically grade I and II injuries; however, pseudoaneurysms and occlusions have also been misdiagnosed.12,13 The risk of angiography in our screened trauma population is 0.1%, while the stroke risk of an undiagnosed grade I CAI is 8% and VAI is 6%.3,4 Recent preliminary studies report improved imaging and visualization of injuries with multislice CT scanners (16 or more slices). These promising advances in technology, which would allow noninvasive evaluation of patients, will clearly facilitate the screening process.
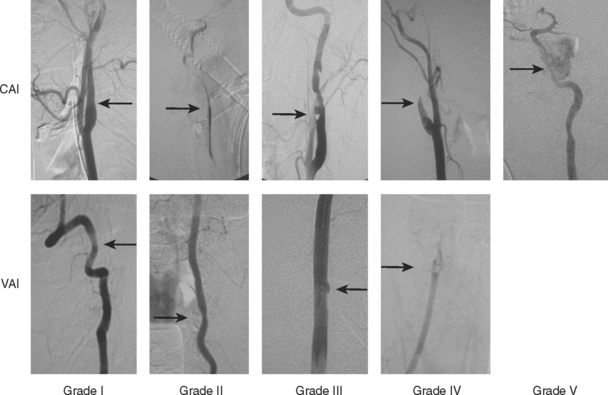
All patients with indications for screening, and no contraindications to antithrombotic therapy, undergo imaging as soon as possible. Patients with documented BCVI undergo repeat imaging 7–10 days after their initial diagnostic study. The importance of routine follow-up imaging is particularly salient in patients with grade I and II injuries; over half of grade I injuries completely heal, allowing cessation of antithrombotic therapy.3 While only 8% of grade II injuries heal, over 40% progress to grade III injuries despite therapy; in patients with CAI, this increase in injury grade also correlates with an increase in stroke risk. Patients with carotid or vertebral artery occlusions are not as important for reimaging, as over 80% display no change on follow-up imaging.
INJURY GRADING SCALE
The identification of disparate outcomes associated with varied luminal irregularities comprising BCVI (dissection, occlusion, transection, and pseudoaneurysms) prompted us to propose a grading scale.10 An injury grading scale was developed to provide not only an accurate description of the injury, but also to define stroke risk by injury grade (Figure 4 and Table 2). Untreated injuries have an overall stroke rate of approximately 20%; CAIs have increasing stroke rate by increasing grade, while VAIs tend to have a more consistent stroke rate of approximately 20% for all grades of injury (Table 3).
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree