Fig. 5.1
Placenta previa. Ultrasound image showing placenta covering cervical os (arrowheads). Image courtesy of Ian Suchet
Management of placenta previa depends on gestational age and stability of the mother. Unstable patients require aggressive resuscitation with blood products and emergent cesarean section. For stable patients, the main goal is to prolong pregnancy until fetal lung maturity is adequate for delivery. Patients between 24 and 34 weeks gestation should be given corticosteroids to accelerate fetal lung maturity if delivery within 7 days is anticipated [25]. Forty-four percent of women with placenta previa deliver before 37 weeks [26]. An obstetrician should evaluate all patients with placenta previa. For the majority of patients, admission to an obstetric unit is required.
Placental Abruption
Placental abruption, also known as abruptio placentae, is defined as separation of the placenta from the uterine wall before delivery. This condition occurs in about 1% of all pregnancies, and about 50% of these occur prior to 36 weeks’ gestation [27–29]. The presentation of placenta abruption can vary widely, making the diagnosis difficult. Placental abruption is the most common cause of intrapartum fetal death, with neonatal mortality ranging 10–30% of all abruption cases [29, 30]. Risk factors for abruptio placentae include maternal trauma, previous abruption, hypertension, cocaine use, multiparity, and advanced maternal age [29–34].
The classic presentation of placental abruption is the acute onset of abdominal pain with or without dark red vaginal bleeding. The hallmark of placental abruption is pain and tenderness, which is found in 70% of patients [33, 35]. The pain may be abdominal, pelvic, or back pain. Contractions in placental abruption are usually high frequency and low amplitude and result in pain worse between contractions [36]. The uterus tends to be firm and rigid, and hypertonia develops as the abruption expands.
Vaginal bleeding occurs in approximately 80–70% of patients with placental abruption [33, 35]. Bleeding can be light to hemorrhagic and may be bright red to dark burgundy. In abruption, maternal spiral arteries rupture, causing blood to accumulate and split the decidua from the uterine wall. A hematoma can develop without vaginal bleeding in 10–20% of abruptions [33]. These “concealed abruptions” are either early in the vessel bleeding phase or there is partial placental separation between the fetal membranes and decidua; hence, these patients present with preterm labor and abdominal pain. However, if bleeding continues, complete dissection of the uterine-placental interface can occur as the hematoma grows. Importantly, the amount of vaginal bleeding does not correlate with the severity of the abruption.
Placental abruption can quickly progress to hemorrhagic shock in the mother, and the lack of gas exchange and nutrients to the fetus causes fetal distress. Indeed, fetal distress is noted in 60% of patients with placenta abruption and may be the only sign that an abruption has occured [35]. When placental separation exceeds 50%, acute disseminated intravascular coagulation (DIC) is common and fetal death is almost certain [37].
Placental abruption is a largely clinical diagnosis. Ultrasound may be used, as a hyperechoic clot or sign of bleeding posterior to the placenta, if visualized, is highly suggestive of placental abruption (Fig. 5.2). Unfortunately, these findings are only present in about 25% of cases [38]. While ultrasound cannot reliably exclude abruption, it can be used to exclude placenta previa.


Fig. 5.2
Ultrasound image showing acute placental abruption with a retroplacental hematoma (arrow) lifting part of the placenta. Meguerdichian, D. “Complications in late pregnancy” Emergency Medicine Clinics of North America. Philadelphia, Elsevier. 2011. Courtesy of Carol Benson, MD, Brigham and Women’s Hospital Department of Radiology, with permission
Management of patients with abruptio placentae should begin with placement of two large bore IVs, resuscitation with intravenous fluids or blood products, reversal of any coagulopathies, and immediate obstetric consultation. Since DIC occurs in about 10% of placenta abruption cases, fibrinogen, PT, and PTT should be sent with standard labs [39]. Blood type and screen should also be sent if this diagnosis is suspected. In most cases of placental abruption, immediate delivery is necessary and tocolytics are contraindicated. One case-control study found that decision to deliver interval of 20 min or less resulted in better neonatal outcomes [40].
Vasa Previa
Vasa previa, from the Latin “vessels before the road,” is the presence of fetal vessels between the cervix and the presenting fetal part. This is a very serious cause of vaginal bleeding in late pregnancy, with greater than 50% perinatal mortality [41]. Rupture of only 100 ml of exposed fetal vessels can cause fetal exsanguination or death [42]. Obstetric consultation should be obtained immediately. The condition is usually diagnosed in the second or third trimester by ultrasound (Fig. 5.3). The incidence of vasa previa is about 1 in 2500 births, yet may be even higher in pregnancies resulting from assisted reproductive technologies [41]. The risk factors for vasa previa include placenta previa, in vitro fertilization, multiple gestations, and velamentous cord insertion (i.e., when the placental end of the umbilical cord consists of divergent umbilical vessels that are not protected by Wharton’s jelly and are at risk for rupture) [41, 43, 44].
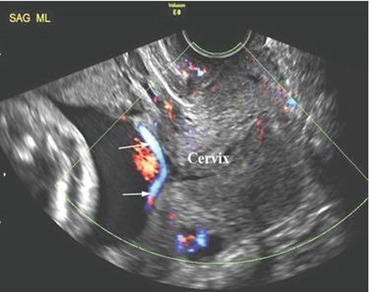
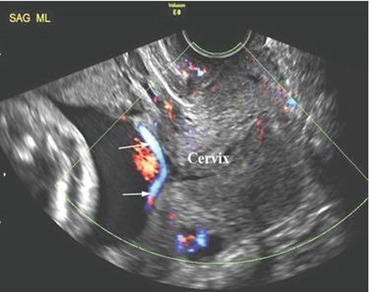
Fig. 5.3
Vasa previa. Arrows pointing to fetal vessels between the cervix and presenting fetal part. Image courtesy of Ian Suchet
Patients with vasa previa tend to present with vaginal bleeding immediately after spontaneous rupture of membranes or amniotomy; it is rare for fetal vessels to rupture without rupture of membranes. Without a history of vasa previa on a prior ultrasound, this diagnosis should be suspected if there are fetal heart abnormalities accompanied with sudden vaginal bleeding after rupture of membranes. Fetal heart monitoring in this condition tends to present as sinusoidal or bradycardic pattern [43, 45]. Any non-reassuring fetal monitoring or unstable maternal vital signs is an indication for operative delivery. Upon delivery, focus should be placed on neonatal resuscitation due to the high mortality rate. If there is a reassuring fetal heart rate, stable maternal vital signs, and nonhemorrhagic vaginal bleeding, an Apt test (a qualitative test of vaginal bleeding to determine the absence or presence of fetal blood) may be performed to diagnose vasa previa [46].
Uterine Rupture
Uterine rupture is a life-threatening cause of vaginal bleeding in late pregnancy. The incidence depends on cause of rupture and is difficult to estimate. It is much more common in patients with history of previous cesarean sections, but is still possible in an unscarred uterus. In fact, 13% of uterine ruptures occur in unscarred uteruses, and this group has a higher morbidity and mortality compared to uterine rupture with a previously scarred uterus [47, 48]. One study found a perinatal mortality of 65% in the unscarred uterus [47]. In addition to history of previous cesarean section, risk factors for uterine rupture include trauma, high parity, advanced maternal age, and congenital disorders (e.g., Ehlers-Danlos) [47–54].
The classic presentation of uterine rupture is the sudden onset of abdominal pain, loss of uterine tone, change in uterine shape or contour, vaginal bleeding, and shock. A scarred uterus rupture may have a less severe onset presentation than that of an unscarred uterus due to previously altered vasculature [47]. Vaginal bleeding may be modest to hemorrhagic depending on the site of uterine rupture. These patients have a tender, boggy uterus on exam, and abdominal girth may quickly expand as blood accumulates. Fetal monitoring is more reliable than abdominal pain in diagnosing uterine rupture [53, 55–58]. Bradycardia is the most common finding on fetal monitoring, but no fetal heart rate pattern is pathognomonic [53, 55–58].
In any suspicion of uterine rupture, immediate resuscitation and surgical intervention are crucial. In the rare situations where there is only mild abdominal pain, stable fetal heart tracings, and light vaginal bleeding, an ultrasound exam may be performed. An abdomen or focused assessment with sonography for trauma (FAST) ultrasound exam with significant blood or defect in uterine wall can help reach the uterine rupture diagnosis. Studies have noted that a physician has about 10–37 min from frank uterine rupture to intervention before there is significant fetal and maternal morbidity [54, 56, 59]. Therefore, this is a diagnosis that should be immediately considered in antepartum hemorrhage.
Other Causes of Antepartum Hemorrhage
The previously discussed topics are some of the more concerning diagnoses of late-trimester vaginal bleeding, but there are numerous causes and degrees of vaginal bleeding in pregnancy. Vaginal and cervical sources of bleeding include vaginitis, cervicitis, warts, polyps, fissures, and trauma. Fibroids and circumvallate placenta are intrauterine causes of vaginal bleeding. Patients may have mild vaginal bleeding following cervical exams, sexual intercourse, or stripping of membranes by obstetricians near term. Most of these cases presents with spotting or minimal vaginal bleeding. Regardless, all patients with vaginal bleeding in late pregnancy should be evaluated with serious concern, and care should be managed in close consultation with an obstetrician.
Summary
Bleeding in late pregnancy can herald potentially life-threatening conditions such as placenta previa, placental abruption, vasa previa, or uterine rupture. These emergencies are infrequently managed in the ED and can be challenging for the entire team. It is incumbent on the emergency physician to make a swift, accurate diagnosis and to lead resuscitative efforts. Obstetric consultation should be obtained as early as possible. Prompt, coordinated interdisciplinary care can be lifesaving for both the mother and fetus. Ultimately, management depends on maternal stability and gestational age; many patients will require emergent cesarean delivery.
Key Points
A pregnant woman past 20 weeks gestation with sudden onset painless vaginal bleeding has placenta previa until proven otherwise.
Digital cervical exams are contraindicated until placenta previa has been excluded.
Placental abruption may present with or without vaginal bleeding; the amount of bleeding does not correlate with the severity of the abruption.
Ultrasound is used to diagnose placenta previa; it cannot reliably exclude placental abruption.
Obstetric consultation should be obtained early in the ED course of all patients with late pregnancy bleeding.
References
1.
Hull AD, Resnick R. Placenta previa, placenta accreta, abruptio placentae, and vasa previa. In: Creasy RK, Resnick R, Iams JD, et al editors. Maternal-fetal medicine: Priniciple and practice. 7th ed. Philadelphia, PA: Elsevier Saunders, p. 732–42.
2.
3.
Silver RM. Abnormal placentation: placenta previa, vasa previa, and placenta accreta. Obstet Gynecol. 2015;126(3):654–68.CrossRefPubMed
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






