44 Biliary Tract Disorders
• Risk factors for the development of gallstone disease include female gender, increasing age, obesity, rapid weight loss, and underlying liver disease.
• The majority of patients with gallstone disease are asymptomatic. Symptomatic complications include biliary colic, acute cholecystitis, choledocholithiasis, cholangitis, and acute pancreatitis.
• A high index of suspicion should be maintained for acute cholangitis in the chronically ill, elderly, or diabetic patients with sepsis of unknown source.
• Ultrasound is the initial diagnostic study of choice in patients with suspected gallstone disease. Cholecystoscintigraphy is the most sensitive test for cholecystitis, and magnetic resonance cholangiopancreatography is the most sensitive test for bile duct stones.
Cholelithiasis and Acute Cholecystitis
Epidemiology
Cholelithiasis affects 20 to 25 million Americans, which represents 10% to 15% of the adult population. Although most gallstones are clinically silent, 20% of people harboring stones experience biliary symptoms at some time; 1% to 2% of patients each year experience complications and require surgical removal of the gallbladder. In the United States, cholecystectomy is the most common elective abdominal surgery, with approximately 750,000 procedures performed per year. Complications of cholelithiasis include acute cholecystitis, ascending cholangitis, acute pancreatitis, and adenocarcinoma of the gallbladder, which result in a combined mortality of 5000 to 10,000 deaths per year (Box 44.1).
Box 44.1 Risk Factors for the Development of Cholelithiasis
Gender
Women have twice the incidence and prevalence of gallstones.
Estrogen stimulates low-density lipoprotein receptors and increases the uptake of cholesterol; higher cholesterol content in bile is associated with greater risk for gallstone formation.1
After menopause, the incidence of gallstone disease in women and men is comparable.
Total Parenteral Nutrition
Loss of enteric stimulation of the gallbladder in the absence of eating leads to gallbladder stasis.
Total parental nutrition (TPN) increases the risk for biliary sludge, gallstone disease, and acalculous cholecystitis.
After 4 weeks of TPN, gallbladder sludge develops in half of patients and after 6 weeks in all. The sludge resolves within 4 weeks of resuming oral intake.4
Family History
Occurrence of gallstone disease within families can be a product of genetic and shared environmental factors.5
The frequency is increased in monozygotic (12%) as opposed to dizygotic twins (6%).6
Genetic effects account for 25%, shared environmental effects for 13%, and unique environmental effects for 62% of the phenotypic variance in gallstone production.7
Chronic Diseases
The overall prevalence of gallstones in patients with cirrhosis is 25% to 30% (double that in the general population).8
Crohn disease causes ileal malabsorption of bile acids. These acids normally solubilize cholesterol and bilirubin to be excreted. An inadequate amount of bile acid means that increased cholesterol and bilirubin are available to form stones.9
Cystic fibrosis is also associated with bile acid malabsorption and gallstones.
Medications
Octreotide is used for the treatment of acromegaly and carcinoid syndrome; it affects biliary motility and sphincter of Oddi function. Cholelithiasis develops in more than 50% of patients receiving octreotide. The majority are asymptomatic.10
Ceftriaxone is secreted unmetabolized into bile, where it reaches high concentrations and produces biliary sludge.11
Pathophysiology
Bile is primarily composed of cholesterol, lecithin, bile salts, bilirubin, and electrolytes (i.e., calcium, carbonate, phosphate). Once these solutes exceed their solubility, they form crystals. Crystals trapped in biliary mucus produce sludge and aggregate to form stones. Cholesterol is the primary constituent in 60% to 80% of all gallstones. Calcium bilirubinate salts predominate in another 10% to 20% of stones; cholesterol and calcium bilirubinate are present in relatively equal quantities in the remainder of calculi. Biliary stasis is thought to play a significant role in stone formation.12
Although bile itself is normally sterile, any alterations in biliary motility lead to an increased risk for bacterial infection. The organisms implicated in cholecystitis are generally bowel flora and include Escherichia coli, Klebsiella, enterococci, and anaerobes.13
Presenting Signs and Symptoms
Gallstones can be manifested as a spectrum of disease and may be divided into asymptomatic, symptomatic, and complicated gallstone disease. Only 15% to 20% of stones become symptomatic, between 1% and 3% per year. Approximately 66% of patients have a recurrent episode of biliary colic within 2 years, and about one in six have a complication of gallstone disease13 (Table 44.1).
Table 44.1 Symptoms of Gallstone Disease and Its Complications
| DISEASE | PATHOPHYSIOLOGY | SYMPTOMS |
|---|---|---|
| Biliary colic | Transient gallstone impaction at the cystic duct or ampulla of Vater | Intermittent RUQ pain associated with nausea or vomiting. Pain in the epigastrium or radiating to the right scapular tip. Episodes last 30 min to several hours with days or months between episodes. |
| Acute cholecystitis | Inflammation of the gallbladder caused by obstruction of the cystic duct May occur in the presence or absence of bacterial superinfection | Patients appear ill and cannot take deep breaths. They have constant pain that lasts 30-60 min and worsens with movement. Persistent common bile duct impaction usually promotes vomiting. Physical examination demonstrates RUQ tenderness with voluntary guarding and a positive Murphy sign (arrest of inspiration during deep palpation over the gallbladder). |
| Emphysematous cholecystitis | Infection with gas-producing bacteria such as Escherichia coli, Clostridium perfringens, and anaerobic streptococci | Symptoms are similar to those with acute cholecystitis. Gas may be seen on abdominal plain films or CT. Male diabetics are most commonly affected. |
| Chronic cholecystitis | Persistent inflammation and fibrosis of the gallbladder with poor motor and absorptive function | Patients are usually asymptomatic but may report multiple previous attacks of colic. Porcelain gallbladder develops from chronic inflammation and may progress to carcinoma. |
| Acalculous cholecystitis | Probably related to biliary stasis in the setting of critical illness and altered gastrointestinal motility | Seen in patients with traumatic injuries, burns, and critical illness, as well as in those receiving total parenteral nutrition. The mortality for this disorder is twice as high as that for acute calculous cholecystitis.14 |
| Gallbladder perforation | Stones erode through an inflamed and necrotic gallbladder wall Stones may travel into the peritoneal cavity or cause adhesions between nearby structures. Bile peritonitis may develop | More than half of patients with gallbladder perforation have fever and a palpable RUQ mass.15 Mortality in these patients is 30%.16 |
CT, Computed tomography; RUQ, right upper quadrant.
Diagnostic Imaging for Cholelithiasis and Cholecystitis
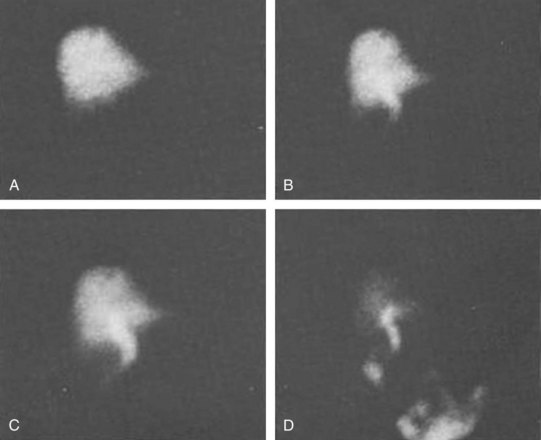
Ultrasonography is the preferred first-line modality for evaluating potential biliary stones (Fig. 44.1). A metaanalysis of studies demonstrated that ultrasound has a sensitivity of 97% and specificity of 95% for the diagnosis of cholelithiasis.17 Common findings on ultrasonography are hyperechoic stones with hypoechoic shadowing, biliary sludge, and stone mobility with changes in patient positioning (Fig. 44.2). Pericholecystic fluid (Fig. 44.3), gallbladder wall thickening (>3 mm), common bile duct dilation (>6 mm), and intrahepatic and extrahepatic biliary ductal dilation are highly suggestive of acute cholecystitis.
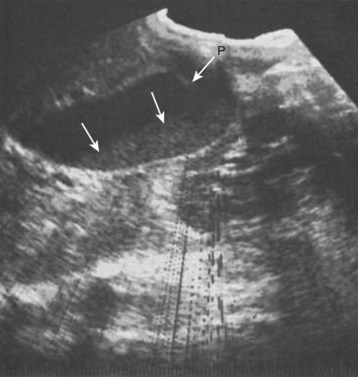
Fig. 44.1 Ultrasonogram demonstrating biliary sludge (arrows).
(From Berk RN, Ferrucci Jr JT, Leopold GR. Radiology of the gallbladder and bile ducts: diagnosis and intervention. Philadelphia: Saunders; 1983. p. 206.)
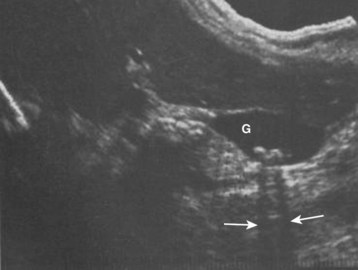
Fig. 44.2 Cholelithiasis shown by ultrasonography (arrows).
(From Berk RN, Ferrucci Jr JT, Leopold GR. Radiology of the gallbladder and bile ducts: diagnosis and intervention. Philadelphia: Saunders; 1983. p. 255.)

Fig. 44.3 Ultrasonogram demonstrating pericholecystic fluid (arrow).
(From Berk RN, Ferrucci Jr JT, Leopold GR. Radiology of the gallbladder and bile ducts: diagnosis and intervention. Philadelphia: Saunders; 1983. p. 213.)
Cholecystoscintigraphy or hepatobiliary iminodiacetic acid (HIDA) scanning is a more sensitive test for diagnosing acute cholecystitis. In this nuclear medicine study, a radioactive tracer is injected peripherally and allowed to circulate to the liver, where it is excreted in bile. In the absence of disease, the gallbladder is visualized within 1 hour of injection (Fig. 44.4). Nonvisualization of the gallbladder within 4 hours after injection indicates either cholecystitis or cystic duct obstruction (Fig. 44.5). In a retrospective review of 170 patients evaluated in the emergency department (ED) because of right upper quadrant (RUQ) pain, cholecystoscintigraphy had a diagnostic sensitivity of 86% for acute cholecystitis as compared with 48% for ultrasonography. In another study, the results of cholecystoscintigraphy were positive in 87% of patients in whom the initial ultrasonographic findings were negative.18
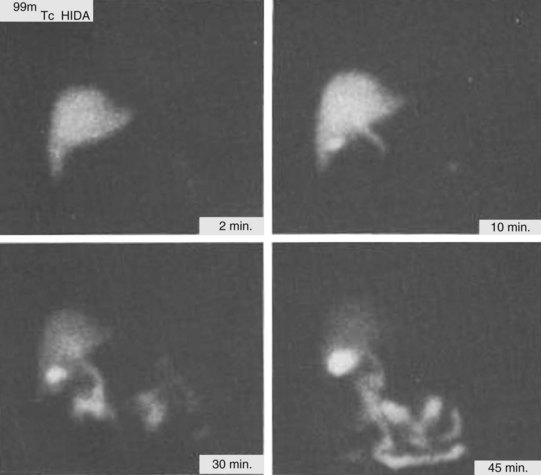
Fig. 44.4 Normal cholecystoscintigrams.
(From Berk RN, Ferrucci Jr JT, Leopold GR. Radiology of the gallbladder and bile ducts: diagnosis and intervention. Philadelphia: Saunders; 1983. p. 265.)