(1)
Chennai Breast Centre, Chennai, India
The lymphatics from most of the breast drain into the axilla except for the medial quadrant which may drain into the internal mammary node as well. The presence of lymph node metastasis, tumor dimensions, and histological grade continue to be the most important prognostic indicators even in the molecular era. Axillary staging is therefore an integral part of management of breast cancer treatment. Traditionally axillary lymph node dissection involves removing all three levels of axillary lymph nodes. The procedure provides staging, prognostic information, and locoregional control but carries a significant morbidity that includes shoulder stiffness, possible damage to medial pectoral nerve, long thoracic nerve of Bell, and neurovascular pedicle of the latissimus dorsi, along with a significant risk of lymphedema. Surgical staging is still the gold standard for the axilla because none of the nonoperative imaging modalities have proven as effective as surgical staging.
Sentinel Lymph Node Biopsy
Sentinel lymph node biopsy has now become the standard technique in early breast cancer. The sentinel lymph node would be the first site of metastatic disease before proceeding to other lymph nodes. The incidence of skip metastasis (metastasis skipping the sentinel node and involving a higher level node) is less than 2 %. Therefore, if the sentinel lymph node does not contain metastatic deposits, it implies that the other lymph nodes are free of tumor.
The sentinel lymph node is identified by injecting radioisotope along with a blue dye in the subareolar region. The radioisotope and the blue dye will be concentrated by the sentinel lymph nodes which will be identified and removed during surgery with the help of a handheld gamma probe and blue staining of the lymph node (Fig. 14.1). The sentinel nodes can be assessed by several methods including touch imprint cytology and frozen section and analysis or by molecular methods to detect metastatic deposits. A complete axillary dissection is performed if the sentinel lymph nodes are positive for metastasis. Further axillary dissection can be omitted if the sentinel nodes are negative.


Fig. 14.1
The sentinel node identified using blue dye and radioisotope
Preoperative ultrasound assessment of the axillary lymph nodes helps in selecting patients for sentinel lymph node biopsy. Under ultrasound guidance suspicious lymph nodes can be sampled by fine-needle aspiration cytology or core needle biopsy and if proven metastatic will undergo axillary clearance.
Axillary ultrasound is also a useful tool to pick up regional recurrence during follow-up.
Normal Lymph Node
The lymph node consists of a cortex and a medulla. The cortex contains subcapsular and cortical sinusoids and lymphatic tissue that includes lymphoid follicles. The medulla consists of medullary cords that contain lymph tissue (Fig. 14.2). The lymph fluid enters through the afferent vessels that penetrate the capsule and enters the subcapsular sinusoids and flows through the cortical sinusoids and finally to the medullary sinusoids. It exits the lymph node through the efferent lymphatic vessels through the hilar notch. The blood supply to the node enters and exits through the hilum. Normal blood vessels do not penetrate through the capsule (Fig. 14.3).
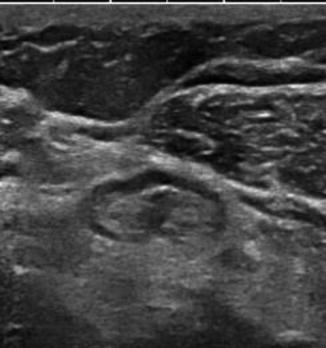
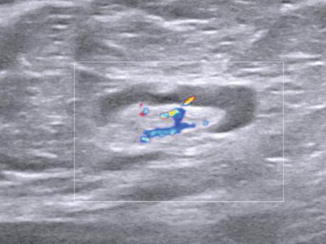
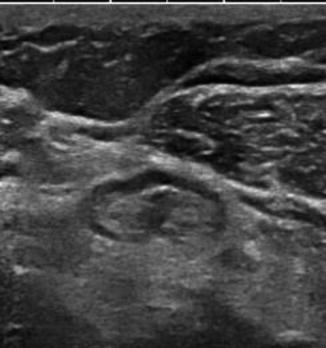
Fig. 14.2
The normal axillary lymph node with normal hypoechoic cortex
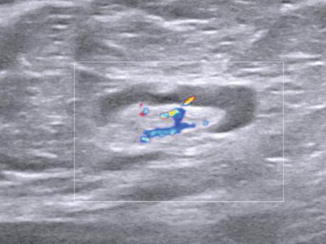
Fig. 14.3




Normal hilar blood flow
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







