Autonomic Nervous System: Physiology and Pharmacology
Anesthesiology is the practice of autonomic nervous system (ANS) medicine (Grecu L. Autonomic nervous system: physiology and pharmacology. In: Barash PG, Cullen BF, Stoelting RK, Cahalan MK, Ortega R, Stock MC, eds. Clinical Anesthesia. Philadelphia: Lippincott Williams & Wilkins; 2013: 362–407). Data recorded on the anesthesia record often reflect ANS function and homeostasis. Drugs used during anesthesia as well as painful stimulation and disease states frequently produce ANS-related side effects.
I. Functional Anatomy
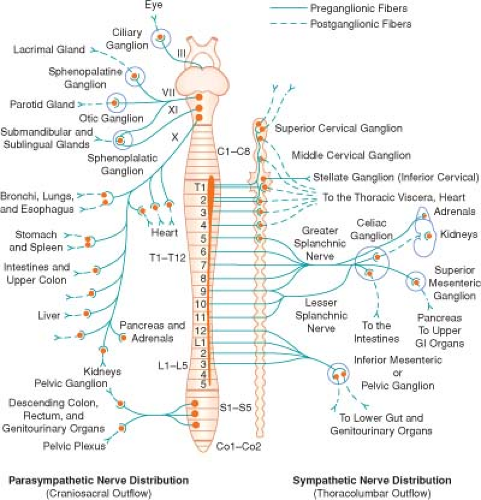
The ANS is divided into the sympathetic nervous system (SNS; adrenergic system) and the parasympathetic nervous system (PNS; cholinergic system) (Fig. 15-1). The SNS and PNS produce complementary effects on the activity of various organ systems (Table 15-1).
Central Autonomic Organization. The principal site of ANS integration (blood pressure control, temperature regulation, stress responses) is the hypothalamus. Vital centers for hemodynamic and ventilatory control are located in the medulla oblongata and pons. ANS hyperreflexia is an example of spinal cord mediation of ANS reflexes without integration of function from higher inhibitory centers.
Peripheral Autonomic Nervous System Organization (Fig. 15-2)
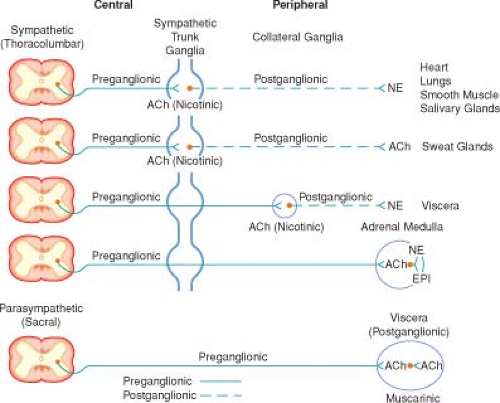
The cell body of the preganglionic neuron originates in the central nervous system (CNS) and synapses in an autonomic ganglion. The adrenal medulla is an exception. Preganglionic fibers are myelinated (rapid conducting).
Postganglionic neurons arise from the autonomic ganglia and are distributed to effector organs. Postganglionic fibers are unmyelinated (slow conducting).
The 22 pairs of SNS (paravertebral) ganglia are located closer to the spinal cord than to the innervated organ.
The PNS ganglia are located in or near the innervated organ.
Whereas activation of the SNS produces a diffuse physiologic response (mass reflex), activation of the PNS produces more discrete responses. For example, vagal stimulation may produce bradycardia with no effect on intestinal motility.
Autonomic Innervation
Heart. SNS and PNS innervation of the heart (via the stellate ganglion) influences heart rate (chronotropism), the strength of contraction (inotropism), and coronary blood flow.
The PNS cardiac vagal fibers are distributed mainly to the sinoatrial (SA) and atrioventricular (AV) nodes,
such that the main effect of cardiac vagal stimulation is chronotropic. Strong vagal stimulation can arrest SA node firing and block impulse conduction to the ventricles.
The SNS has the same supraventricular distribution as the PNS but with stronger distribution to the ventricles. Normal SNS tone maintains contractility about 20% above that in the absence of SNS stimulation.
Peripheral circulation. The SNS is the most important regulator of the peripheral circulation. Basal ANS tone maintains arteriolar diameter at about 50% of maximum, thus permitting the potential for further vasoconstriction or vasodilation. By functioning as a reservoir for about 80% of the blood volume, small changes in venous capacitance produced by SNS-mediated venoconstriction produce large changes in venous return.
Table 15-1 Homeostatic Balance Between Divisions of the Autonomic Nervous System | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
II. Autonomic Nervous System Transmission
Transmission of impulses across the nerve terminal junctional sites (synaptic cleft) of the peripheral ANS occurs through the
mediation of liberated chemicals (neurotransmitters). These neurotransmitters interact with a receptor on the end organ to evoke a biologic response.
Parasympathetic Nervous System Neurotransmission
Acetylcholine (ACh) is the neurotransmitter at preganglionic nerve endings of the SNS and PNS and at postganglionic nerve endings of the PNS.
The ability of a receptor to modulate the function of an effector organ depends on rapid recovery to its baseline state after stimulation. ACh removal occurs by rapid hydrolysis by acetylcholinesterase (true cholinesterase). Pseudocholinesterase (plasma cholinesterase) is not physiologically significant in the termination (hydrolysis) of ACh action.
Sympathetic Nervous System Neurotransmission
Norepinephrine is the neurotransmitter at postganglionic nerve endings of the SNS (except in the sweat glands, where ACh is the neurotransmitter).
Adenosine triphosphate (ATP) is released with norepinephrine and thus functions as a co-neurotransmitter.
Epinephrine is the principal hormone released by chromaffin cells (which function as postganglionic SNS neurons) into the circulation to function as a neurotransmitter hormone.
Catecholamines: The First Messenger
Endogenous catecholamines are dopamine (neurotransmitter in the CNS), norepinephrine, and epinephrine. A catecholamine (including synthetic catecholamines) is any compound with a catechol nucleus (benzene ring with two adjacent hydroxyl groups) and an amine-containing side chain (Fig. 15-3).
The effects of endogenous or synthetic catecholamines on adrenergic receptors can be indirect (little intrinsic activity but stimulate release of stored neurotransmitter) and direct.
Inactivation of catecholamines is by reuptake back into presynaptic nerve terminals by extraneuronal uptake, diffusion, and metabolism.
III. Receptors
Receptors appear to be protein macromolecules on cell membranes, which when activated by an agonist (ACh or norepinephrine) lead to a response by an effector cell. An antagonist is a substance that attaches to the receptor (prevents access of an agonist) but does not elicit a response by the effector cell.
Cholinergic receptors are subdivided into muscarinic (postganglionic nerve endings) and nicotinic (autonomic ganglia, neuromuscular junction) receptors. ACh is the neurotransmitter at cholinergic receptors. Atropine is a specific antagonist at muscarinic receptors.
Adrenergic receptors are subdivided into α, β, and dopaminergic, with subtypes for each category (Table 15-2).
α-Adrenergic Receptors in the Cardiovascular System
Coronary arteries. Postsynaptic α2 receptors predominate in the large epicardial conductance vessels.
They contribute about 5% to total coronary artery resistance, which is why phenylephrine has little influence on resistance to blood flow in coronary arteries. Postsynaptic α2 receptors predominate in small coronary artery resistance vessels. The density of α2 receptors in the coronary arteries increases in response to myocardial ischemia.
Peripheral Vessels. Presynaptic α2-vascular receptors mediate vasodilation, and postsynaptic α1– and α2-vascular receptors mediate vasoconstriction. Postsynaptic α2-vascular receptors predominate on the venous side of the circulation. Actions attributed to postsynaptic α2 receptors include arterial and venous vasoconstriction, platelet aggregation, inhibition of insulin release, inhibition of bowel motility, and inhibition of antidiuretic hormone release.
α Receptors in the Kidneys. The α1 receptors dominate in the renal vasculature (vasoconstriction modulates renal blood flow), and the α2 receptors predominate in the renal tubules, especially the loops of Henle (which stimulate water and sodium excretion).
β Receptors in the Cardiovascular System
Myocardium. Postsynaptic β1 receptors and presynaptic β2 receptors probably play similar roles in the regulation of heart rate and myocardial contractility. Increased circulating catecholamine levels associated with congestive heart failure result in downregulation of β1 receptors with relative sparing of β2 and α1 receptors. (β2 and α1 receptors increasingly mediate the inotropic response to catecholamines during cardiac failure.)
Peripheral Vessels. Postsynaptic vascular β receptors are predominantly β2.
β Receptors in the Kidneys. β1 receptors are more prominent than β receptors in the kidneys, and their activation results in renin release.
Adrenergic Receptor Numbers and Sensitivity
Receptors are dynamically regulated by a variety of conditions (ambient concentrations of catecholamines and drugs and genetic factors), resulting in altered responses to catecholamines and ANS stimulation.
Alteration in the number or density of receptors is referred to as upregulation or downregulation. Chronic treatment with clonidine or propranolol results in upregulation and a withdrawal syndrome if the drug is acutely discontinued.
Table 15-2 Adrenergic Receptors and Order of Potency of Agonists and Antagonists | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|