48 Asthma
• Asthma is a chronic inflammatory condition that can be controlled.
• Indications of inadequate control of asthma include frequent use of short-acting β-agonist agents, wheezing, coughing, and nighttime symptoms.
• Emergency department treatment of asthma exacerbation includes a targeted history and physical examination, aerosolized β-agonist agents, and systemic steroids with objective measures of response to therapy. Anticholinergic agents should be used in the emergency department for patients with a severe exacerbation.
• At discharge, controller medications should be prescribed in addition to rescue medications for patients with chronic persistent asthma. Patients should follow up with a primary care physician or asthma specialist within several weeks.
Perspective
Asthma is a chronic inflammatory disorder characterized by increased responsiveness of the airways to multiple stimuli. Many cells and cellular elements, such as mast cells, eosinophils, T lymphocytes, macrophages, neutrophils, and epithelial cells, play a role in development of the inflammatory response.1 The inflammation causes recurrent episodes of wheezing, breathlessness, chest tightness, and coughing, particularly at night or in the early morning. These episodes are associated with airflow obstruction that is reversible either spontaneously or with treatment. Although patients appear to clinically recover completely, evidence suggests that some asthmatic patients have chronic airflow limitation. The recognition that asthma is a chronic inflammatory disorder of the airways has significant implications for the diagnosis, management, and potential prevention of acute exacerbations.
Epidemiology
Asthma affects approximately 4% to 5% of the population in the United States.2 Although it is the most common chronic disease of childhood, with a prevalence of 5% to 10%, it also affects 7% to 10% of the elderly. Epidemiologic studies suggest that asthma is underdiagnosed and undertreated in all age groups. Part of the problem is that the transient nature of asthma allows many patients to tolerate intermittent respiratory symptoms before seeking medical care. Another important factor resulting in underdiagnosis of asthma is the sometimes nonspecific nature of the symptoms.
About half of cases of asthma develop before 10 years of age and another third before 40 years. The 2 : 1 male-to-female preponderance of asthma in childhood equalizes by 30 years of age.3 The average asthmatic patient has 15 days of restricted activity each year and spends 5.8 days in bed. Approximately 2 million emergency department (ED) visits, 484,000 hospitalizations, and more than 4000 deaths per year are attributed to asthma. In the United States alone, the estimated direct and indirect cost of asthma in all age groups was $56 billion in 2007.4
Pathophysiology
Allergic asthma occurs when inhaled allergens bind to immunoglobulin E molecules bound to mast cells in the lining of the tracheobronchial tree. During the early response, various mediators are released and cause greater vascular permeability, mucosal edema, and contraction of bronchial smooth muscle. A second wave of reaction, the late response, is seen hours to days later; it involves accumulation of inflammatory cells in the bronchial mucosa, thus perpetuating the reaction. The release of mediators and regulation of the inflammatory process in asthma are complex, redundant, and self-perpetuating.5
Although several theories attempt to explain the pathophysiologic changes that occur in nonallergic asthma, none adequately explain all clinically observed phenomena. Research suggests that even patients without atopy have pathophysiology similar to that in atopic patients.5 Respiratory infections, particularly viral infections, may precipitate bronchospasm. Viruses cause mucosal inflammation and lower the firing threshold of the subendothelial vagal receptors, which results in enhanced airway reactivity that may last up to 8 weeks, even in nonasthmatic persons. Pharmacologic agents, such as aspirin and nonsteroidal antiinflammatory compounds, coloring agents, and beta-blockers, also induce acute asthma. In addition, sulfating agents, which are used widely as food preservatives and antioxidants in pharmaceutical products, can exacerbate asthma.
Most patients with asthma seem to display an exaggerated bronchoconstrictive response to a variety of exogenous and endogenous stimuli, and inflammation plays a key role. The final common pathway is as follows1:
Presenting Signs and Symptoms
Diagnostic Testing
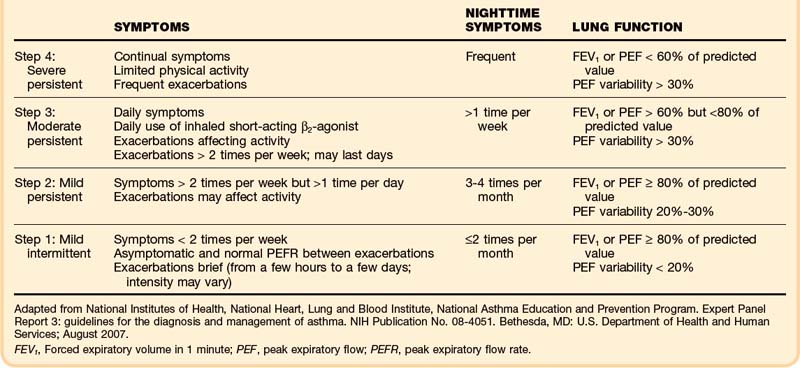
As for all patients who come to the ED for care, a directed history and physical examination should be performed. Key historical points should be elicited, such as the duration and onset of the current attack, identification of precipitating causes, type and amount of medications used before arrival at the ED, response to previous therapy, including current or previous use of corticosteroids, frequency of ED visits and hospitalizations, previous need for intubation or ventilation, history of concurrent medications and allergies, and history of concurrent medical problems. At some point during the patient’s ED stay, effort should be made to evaluate both the severity of the obstruction and the adequacy of ongoing asthma control (Table 48.1).
The physical examination should focus on observing respiratory effort and use of accessory muscles and listening for wheezing or other abnormal breath sounds and prolongation of the expiratory phase. Although wheezing results from movement of air through narrowed airways, the intensity of the wheeze may not correlate with the severity of airflow obstruction. Tachycardia and tachypnea are usually present in patients with acute asthma, but vital signs normalize very quickly as the airflow obstruction is relieved.10 Therefore, a normal heart rate and respiratory rate are not reliable indicators of the degree of relief from obstruction.
Bedside spirometry provides a rapid, objective assessment of patients and helps both indicate the effectiveness of and guide therapy. Sequential measurements assist emergency physicians in assessing the severity of the problem and determining the response to therapy. Although forced expiratory volume in 1 second (FEV1) and the peak expiratory flow (PEF) rate measure the extent of large airway obstruction, patient cooperation is essential for these tests to be reliable. When possible, management decisions should be guided by a patient’s personal best PEF rate or FEV1 value or, if unknown, a percentage of the predicted value in addition to other physiologic and historical factors.1
Pulse oximetry is a useful and convenient method for accessing oxygenation and monitoring oxygen saturation during treatment. Analysis of arterial blood gases is not indicated in the majority of patients with mild to moderate asthma exacerbation, but it is helpful if there is concern for hypoventilation with carbon dioxide retention and respiratory acidosis. Patients with the latter problems almost always have clinical evidence of severe attacks or spirometry demonstrating PEF or FEV1 less than 25% of the predicted value.11,12 Practitioners should be aware that a normal or slightly elevated PaCO2 (e.g., 42 mm Hg or higher) indicates extreme airway obstruction and fatigue and may herald the onset of acute ventilatory failure.11,12
Routine radiography is unnecessary but is indicated if the possibility of pneumothorax, pneumomediastinum, pneumonia, or other medical conditions is a concern. In up to one third of asthmatic patients requiring admission, an abnormality is demonstrated on chest radiographs.13
Use of exhaled nitric oxide measurements and other serum and urine markers for detection of the severity of the asthma exacerbation is currently under investigation.14–17