Aspiration Pneumonitis
Raymond R. Schultetus
CASE SUMMARY
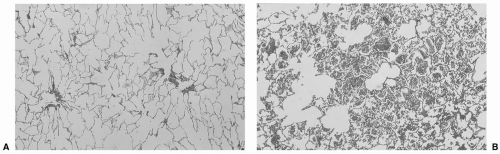
A 25-year-old, 110 kg, 64”, term pregnant woman undergoes cesarean section for a suspected uterine rupture. General anesthesia is induced and during a difficult, although successful, intubation, gastric contents are observed in her posterior pharynx. Her endotracheal tube is quickly suctioned; however, gastric contents are not recovered. The patient is ventilated with 50% oxygen, 50% nitrous oxide, and 0.75% isoflurane. Her oxygen saturation by pulse oximetry is 90%. The nitrous oxide is discontinued with little increase in oxygen saturation. An arterial blood gas is obtained and sent for analysis. After the administration of 10.0 cm H2O positive end-expiratory pressure (PEEP), her saturation increases to 98%. At the completion of the surgery, her FIO2 is 0.5, and she is maintained on mechanical ventilation and PEEP. In the postanesthesia care unit, a chest radiograph is obtained, which does not reveal acute changes. The arterial blood gas sample taken during surgery, where the FIO2 is 0.5, reveals a pH of 7.45, a PACO2 of 34 mm Hg, and a PaO2 of 60 mm Hg. During the next several hours, her inspired oxygen is reduced to 30%, and her saturation remains above 95%. A chest radiograph now reveals a right lower lobe infiltrate (see Fig. 10.1). In stepwise fashion, PEEP is reduced to 5 cm H2O, and a subsequent arterial blood gas reveals a pH of 7.43, PACO2 of 33 mm Hg, and PaO2 of 110 mm Hg. She is extubated without incident and administered 40% oxygen by mask. Her oxygen saturation remains above 97%. She is discharged after the third postoperative day.
What Baseline Knowledge Is Relevant?
▪ DEFINITIONS
Aspiration pneumonitis is the lung’s reaction to the pulmonary aspiration of gastric contents. For aspiration pneumonitis to occur, certain conditions (Table 10.1) must be present. Typically, aspirated gastric contents are a mixture of liquids, particulate matter, digestive enzymes, and acid. On occasion, large particles of food are present. Generally, it is accepted that the aspirated gastric contents must exceed 25 mL in volume (0.4 mL per kg) and have a pH <2.5 to produce clinically significant lung pathology.1 However, gastric contents at a neutral pH, especially if they include particulate matter, can also produce significant and long-lasting lung pathology.2
HISTORIC CONSIDERATIONS
The syndrome, now known as aspiration pneumonitis, was originally called Mendelson syndrome in recognition of the clinician, C. L. Mendelson, who described pulmonary aspiration of gastric contents in an obstetric population. In his study, Mendelson reviewed the records of 44,016 deliveries where, over a 13-year period (1932 to 1945), ether analgesia was administered to laboring women.3 During this period, the administration of ether (ether, nitrous oxide, oxygen) by mask for delivery analgesia and surgical anesthesia was de rigueur. From his review, he identified 66 cases of aspiration of gastric contents (0.15%). Forty-five cases of aspiration were recognized at the time of occurrence; however, 21 cases were noted retrospectively on the basis of maternal postdelivery signs and symptoms. Of the 45 cases identified at delivery, 5 women aspirated solids. Of these, three women had complete airway obstruction and two died of suffocation, whereas one coughed out a piece of meat and survived. The remaining two had incomplete airway obstruction, which cleared upon coughing. Forty cases of liquid aspiration remained. From these cases, Mendelson described a syndrome of tachycardia, cyanosis and dyspnea, and a chest radiograph showing scattered, soft, mottled, confluent densities. Over half of the patients who had aspirated were not treated with antibiotics (3 received penicillin, 14 were administered sulfonamides, and 2 received both penicillin and
sulfonamides). None of the patients had a bronchoscopic examination, nor received steroids or were administered PEEP. All but the two women who suffocated immediately because of the aspiration of large food particles survived.
sulfonamides). None of the patients had a bronchoscopic examination, nor received steroids or were administered PEEP. All but the two women who suffocated immediately because of the aspiration of large food particles survived.
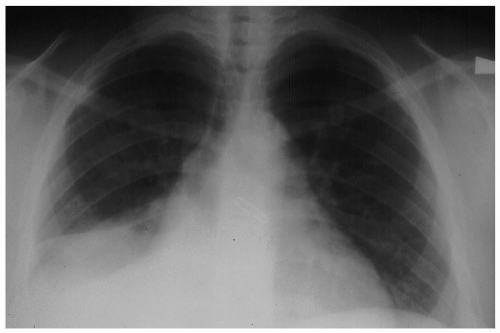 FIGURE 10.1 Aspiration pneumonitis occurring during an unexpected difficult intubation for an elective cesarean section. A right lower lobe infiltrate is apparent on this chest radiograph. |
Because studies contemporary to Mendelson suggested a true incidence of aspiration in a surgical population of 15% to 20% at a time when mask anesthesia prevailed, conservatively one can estimate that many hundreds of Mendelson’s study population must have aspirated but were not identified because the aspirations did not produce clinically apparent symptoms.4,5
In the same study in which he reported the cases of aspiration, Mendelson also included results of a study in which he caused rabbits to aspirate various liquids, ranging from vomitus to acid solutions (10% hydrochloric acid in saline), and determined that the main causative agent in the production of aspiration pneumonitis was acid.
Shortly after the publication of Mendelson’s study, Teabeaut et al. reported results of a study, also in rabbits, wherein an aspirate of 0.4 mL per kg of fluid at a pH <2.5 was necessary to produce the signs and symptoms of pulmonary aspiration.6 These results were supported in the Rhesus monkey.1 On the basis of these studies, the authors recommended that to reduce the risk of aspiration pneumonia during childbirth, the mothers not be fed, and antacids be administered every 3 hours during labor. The administration of particulate antacids during labor became standard practice until 1979 when it was demonstrated in dogs that the aspiration of particulate antacids produced a lung reaction at least as severe as the aspiration of acids (see Fig. 10.2).7
TABLE 10.1 Conditions Required for Pulmonary Aspiration of Gastric Contents to Occur | ||||||||
|---|---|---|---|---|---|---|---|---|
|
How Is the Diagnosis of Aspiration Pneumonitis Made?
Generally, patients who aspirate gastric contents have a decreased sensorium, with consciousness depressed by drugs or a head injury. On occasion, patients aspirate because neuromuscular disease has rendered their protective reflexes incompetent. Uncommonly, intubated patients may aspirate although cuffed endotracheal tubes supposedly protect their airways.8
The classic symptom complex associated with pulmonary aspiration is sudden in onset, with wheezing, shortness of breath, cyanosis, and tachycardia. Frequently gastric contents are noted in the oropharynx. The clinical response to aspiration is variable, and “silent” aspiration occurs as well. In such cases, a fever, low oxygen saturation, or abnormal findings on a chest radiograph may be the only presenting findings.3
A chest radiograph can be useful in diagnosing aspiration pneumonitis; however, in patients who aspirate and have an uncomplicated clinical course, 8% may have normal chest radiographs throughout their hospitalization. In almost one third of aspiration cases, the initial chest radiograph does not represent the full extent of lung involvement, and the findings on the chest film will worsen before improvement is seen.8
No particular distribution of lung injury on the chest radiograph is diagnostic of aspiration pneumonitis. Both the right and left lungs may be affected, and any lobe of the lungs may be involved (see Table 10.2). Likewise, the characteristics of the infiltrates noted on the chest film are not diagnostic (see Table 10.3). Small, irregular lung infiltrates are generally observed; however, mixed infiltrates are seen and may be misinterpreted as acute processes superimposed upon chronic processes, or even as two distinct disease processes.
The earliest clinical findings reflective of the pulmonary aspiration of gastric contents are those of altered pulmonary function. Following aspiration, reflex laryngospasm and bronchospasm result because of chemical and physical irritation of the airways. Surfactant activity decreases with the ensuing rapid development of airway and alveolar injury and fluid exudation. Intrapulmonary shunting develops, and hypoxemia results.9 With increasing damage to lung tissue, lung compliance decreases.
Perhaps in many cases, the diagnosis is never made. Clinically insignificant aspiration pneumonitis may produce no apparent signs or symptoms.3 However, most often the diagnosis is first suspected following the
observation of gastric contents in the posterior pharynx at the time of intubation or because of an unexpectedly low arterial saturation measured by pulse oximetry in a situation where aspiration of gastric contents is likely.10
observation of gastric contents in the posterior pharynx at the time of intubation or because of an unexpectedly low arterial saturation measured by pulse oximetry in a situation where aspiration of gastric contents is likely.10
Not all patients who aspirate gastric contents need extended hospitalization or ventilatory support. In a study of 66 cases of aspiration, none of the 42 patients classified as American Society of Anesthesiologists'(ASA) I or II patients who aspirated and were asymptomatic for cough, wheeze, radiographic pathology, or hypoxemia by pulse oximeter during the first 2 postoperative hours required treatment other than, in some cases, an increase in FIO2. After 2 symptom-free hours and with a saturation of more than 90% while breathing room air, the patients were discharged home or to the ward according to the preoperative plan. In contrast, of the 24 patients with signs or symptoms of pneumonitis, two thirds required ventilation for longer than 6 hours. Increased symptom severity, prolonged ventilation, and extended hospitalization correlated strongly with comorbidities.10 Initially, if the patient manifests symptoms, then the diagnosis is confirmed by a low arterial partial pressure of oxygen determined from an arterial blood gas, and later, diagnosis is confirmed by chest radiographic changes.
TABLE 10.2 Frequency with Which Lung Zones Demonstrate Infiltrates on Initial Chest Radiograph Following Aspiration of Gastric Contents (Seldom is Only One Lung Zone Involved) | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||
▪ PHYSIOLOGIC CHANGES
When aspiration of gastric contents occurs, the fluid spreads rapidly into the lungs. Hammelberg and Bosomworth found that it took the aspirate <20 seconds to reach its maximum distal point of spread in the lung.11 The acid in the aspirate produces chemical burns of the airways and alveoli. Capillary permeability increases, and surfactant is removed. Surfactant production is reduced by injury to type II alveolar cells. With the loss of surfactant, alveolar collapse occurs, and intrapulmonary shunting and hypoxemia develop.
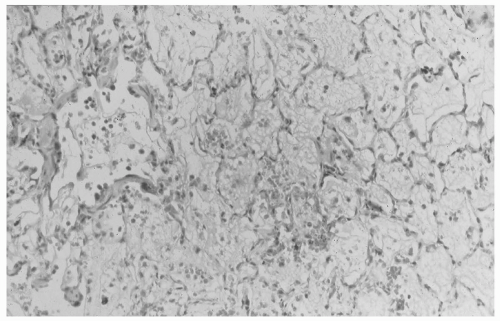
An acid aspirate produces hemorrhagic pulmonary edema, with the edema fluid containing blood, fibrin, and polymorphonuclear leukocytes. Acid aspiration also produces necrosis of the alveolar septa (see Fig. 10.3). A particulate aspiration (at neutral pH) causes a peribronchiolar reaction centering on the food particles, small airway obstruction with distal atelectasis, and a shunt, leading to hypoxemia (see Fig. 10.4). An acid aspirate containing food particles results in pathology combining the deleterious effects of each. Even the aspiration of saline solution produces a transient intrapulmonary shunt and hypoxemia.7
TABLE 10.3 Character of Infiltrate Identified on Initial Chest Radiograph, and Frequency of Finding This Pattern in 60 Patients Presenting to the Emergency Department with a Diagnosis of Pulmonary Aspiration of Gastric Contents | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||
What Is the Treatment for Suspected Aspiration?
If regurgitation is noticed on induction, the patient is placed in a head-down position, and the oropharynx is suctioned before intubation. Immediately after intubation, the endotracheal tube and the bronchi are suctioned (only as long as the arterial saturation [SpO2] supports this maneuver). The patient is then ventilated. Although there are no controlled studies to confirm the utility of suctioning the tracheobronchial tree before ventilation, brief suctioning seems logical and prudent. Extensive suctioning is not indicated because, as noted earlier, it has been shown that the acid from the aspirate spreads rapidly to the most distal recesses.11 Likewise, early bronchoscopy is of little use in preventing further damage, although later, bronchoscopy may be of use if larger bits of aspirate or thick secretions are blocking large airways and producing segmental atelectasis. Bronchial lavage is of little benefit, except in combination with bronchoscopy to clear large airways of thick secretions or debris. Remember that even saline aspiration produces transient pulmonary changes that result in hypoxemia.7
Although there is a significant inflammatory response to aspirated material, steroids have not been shown to be helpful, and may be harmful by impeding normal healing.12,13
Unless the aspirate is perceived to be grossly contaminated, such as might be seen with a bowel obstruction, prophylactic antibiotics are not helpful. Because of gastric acidity, most aspirates of gastric contents are sterile and do not require antibiotics.14 Furthermore, prophylactic antibiotic use may allow secondary infection by opportunistic flora. Antibiotic use should be based on positive culture results. If patients become infected following aspiration, the infection is most likely secondary to improper sterile technique used during tracheal suctioning and will involve opportunistic, hospital-acquired organisms.15,16
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree