Anesthesia for Ophthalmologic Surgery
Anesthesia for ophthalmic surgery presents unique anesthetic challenges and requirements (Table 48-1) (McGoldrick KE, Gayer SI. Anesthesia for ophthalmologic surgery. In: Barash PG, Cullen BF, Stoelting RK, Cahalan MK, Ortega R, Stock MC, eds. Clinical Anesthesia. Philadelphia: Lippincott Williams & Wilkins; 2013:1373–1399). Patients undergoing ophthalmic surgery may represent extremes of age (macular degeneration is the leading cause of blindness in individuals older than 65 years of age) and coexisting medical diseases.
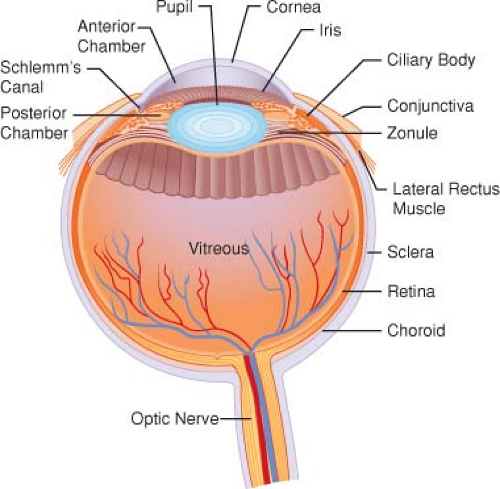
I. Ocular Anatomy
The supraorbital notch, infraorbital foramen, and lacrimal fossa are clinically palpable and function as important landmarks for performance of regional anesthesia (Fig. 48-1).
The coat of the eye is composed of three layers: the sclera, uveal tract, and retina.
Whereas the fibrous outer layer of the sclera is protective, providing sufficient rigidity to maintain the shape of the eye, the anterior portion of the sclera, the cornea, is transparent, permitting light to enter the internal ocular structures.
The uveal tract consists of the iris, ciliary body, and choroid.
The pupil is part of the iris that controls the amount of light that enters by dilation (sympathetic innervation) or constriction (parasympathetic innervation).
The ciliary body produces aqueous humor.
The retina is a neurosensory membrane that converts light impulses to neural impulses that travel via the optic nerve to the brain.
Six intraocular muscles move the eye within the orbit.
Table 48-1 Requirements for Ophthalmic Surgery
Akinesia
Profound analgesia
Minimal bleeding
Avoidance of the oculocardiac reflex
Control of intraocular pressure
Awareness of possible drug interactions
Smooth emergence (awakening without coughing, straining, or vomiting)
The conjunctiva is a mucous membrane (topical administration of ophthalmic drugs) that covers the globe and serves as a lining of the eyelids.
Blood supply to the eye is from branches of the internal and external carotid arteries.
II. Ocular Physiology
Formation and Drainage of Aqueous Humor
Aqueous humor is formed in the posterior chamber by the ciliary body in an active secretory process involving carbonic anhydrase as well as by passive filtration from the vessels on the anterior surface of the iris.
Drainage of aqueous humor is via a network of connecting venous channels (includes Schlemm’s canal) that empty into the superior vena cava. (Any obstruction between the eye and right atrium impedes aqueous drainage and increases intraocular pressure [IOP].)
Maintenance of Intraocular Pressure
IOP normally varies between 10 and 21.7 mm Hg but becomes atmospheric when the globe is opened. The major determinant of IOP is the volume of aqueous humor.
Any sudden increase in IOP when the globe is open may lead to prolapse of the iris and lens, extrusion of the vitreous, and blindness.
Straining, vomiting, or coughing (as during laryngoscopy and tracheal intubation) greatly increases venous pressure and IOP.
Glaucoma is characterized by increased IOP, resulting in impairment of capillary blood flow to the optic nerve.
Treatment consists of topical medication to produce miosis and trabecular stretching.
Atropine premedication in the dose range used clinically has no effect on IOP in patients with glaucoma. (Scopolamine may have a greater mydriatic effect, and its use may be avoided.)
III. Effects of Anesthesia and Adjuvant Drugs on Intraocular Pressure
Equipotent paralyzing does of all the nondepolarizing neuromuscular blocking drugs directly lower IOP by relaxing the extraocular muscles.
Intravenous (IV) injection of succinylcholine (SCh) transiently increases IOP by about 8 mm Hg with return to baseline in 5 to 7 minutes (reflects the cycloplegic action of SCh and is not reliably prevented by pretreatment with nondepolarizing muscle relaxants or IV administration of lidocaine).
It is no longer valid to recommend that SCh be used only with extreme reluctance in ocular surgery (any
SCh-induced increase in IOP would be dissipated before surgery is started), but SCh is not the ideal drug for penetrating ocular wounds.
Table 48-2 Events that Alter Intraocular Pressure
Decrease
Increase
Volatile anesthetics
Increased venous pressure (coughing, vomiting)
Injected anesthetics (? ketamine)
Direct laryngoscopy
Hyperventilation
Hypoventilation
Hypothermia
Arterial hypoxemia
Mannitol
Succinylcholine
Glycerin
Nondepolarizing muscle relaxants
Timolol
Betaxolol
SCh may interfere with interpretation of the force duction (FDT) test used to determine if strabismus is caused by muscle paresis or a restrictive force (need to wait about 20 minutes after administering SCh to perform the FDT).
In light of the boxed warning issued by the Food and Drug Administration stating that use of SCh in children may rarely be associated with hyperkalemia and cardiac arrest, it should be reserved for emergency intubation or when immediate airway control is needed (reason SCh is typically avoided in pediatric strabismus surgery).
IV. Oculocardiac Reflex
This reflex manifests as bradycardia (and occasionally cardiac dysrhythmias) that is elicited by pressure on the globe and by traction on the extraocular muscles (strabismus surgery), especially the medial rectus.
Monitoring of the electrocardiogram is useful for early recognition of this reflex.
Atropine given intravenously within 30 minutes of surgery is thought to lead to a reduced incidence of the reflex (controversial). Atropine as administered intramuscularly for preoperative medication is not effective for preventing this reflex.
V. Anesthetic Ramifications of Ophthalmic Drugs
Anticholinesterase Agents. Echothiophate is a long-acting anticholinesterase miotic that decreases IOP and prolongs the duration of action of SCh.